Age-related macular degeneration (AMD) is a chronic eye condition that gradually diminishes central vision, impacting everyday activities such as reading, driving, and recognizing faces. Many people associate the disease with irreversible damage to the retina, believing that once sight is lost, little can be done beyond slowing further deterioration. Yet rapid advances in stem cell research are challenging this view. One particularly intriguing development centers on mesenchymal stem cell exosomes—tiny, extracellular vesicles carrying signals and proteins capable of stimulating tissue repair.
In recent years, scientists and ophthalmologists have turned to these exosomes for their potential to regenerate vital retinal pigment epithelium (RPE) cells. RPE cells form a critical layer at the back of the eye, nourishing photoreceptors and maintaining the overall health of the macula. By facilitating better communication between cells and delivering growth factors, mesenchymal stem cell exosomes may offer a novel approach to restoring function in areas previously affected by AMD. Below, we explore how this innovative therapy works, its emerging role in vision care, and what it might mean for those seeking fresh hope in managing or reversing AMD.
Key Insights into Exosome-Based Therapy for AMD
Mesenchymal stem cell (MSC) exosomes have gained attention for their versatility in tissue repair and regenerative medicine. These nano-scale vesicles are packed with molecular cargos such as proteins, lipids, RNA, and other signaling molecules. Released naturally by MSCs to facilitate cell-to-cell communication, exosomes function somewhat like “biological mail carriers,” transferring essential messages that drive tissue healing. As researchers began to understand this mechanism, interest in applying exosomes to degenerative eye disorders, particularly AMD, soared.
What Makes Exosomes Stand Out
Exosomes differ from the stem cells themselves in several ways. While MSC transplantation involves placing living cells into the body—carrying both potential benefits and immunologic risks—exosomes are acellular. Essentially, they deliver the therapeutic payload without introducing the complexities of whole cells. This attribute can significantly reduce safety concerns such as graft-versus-host disease or the risk of uncontrolled cell proliferation.
Moreover, because exosomes are nanosized and lipid-based, they can traverse extracellular barriers more efficiently than cells. In the context of AMD, getting therapeutic agents precisely to the retina and RPE cells is challenging. Some treatments struggle to cross ocular barriers or remain stable in the vitreous humor. Exosomes’ small size and composition enable them to diffuse through ocular tissues, reaching target cells with less invasiveness.
The Role of RPE Cells in AMD
The retinal pigment epithelium is a single layer of cells located beneath the photoreceptors (rods and cones). Its responsibilities include:
- Nourishment: RPE cells deliver essential nutrients to photoreceptors, ensuring their optimal function.
- Waste Management: They clear out debris like shed photoreceptor outer segments.
- Barrier and Immune Regulation: RPE cells help form the blood-retinal barrier and modulate immune responses in the eye.
When AMD progresses—particularly the “dry” form—RPE cells degrade or die. Without healthy RPE, photoreceptors lose their source of nutrients and can eventually stop functioning. This cellular loss is what leads to the characteristic central vision impairment. Standard treatments for dry AMD have historically been limited to nutritional supplements (like antioxidants and zinc), as well as lifestyle modifications. While these measures can slow progression, they rarely restore lost RPE function. Introducing exosomes offers an alternative route: by encouraging RPE regeneration and improving cellular vitality, it aims to directly tackle one of the key pathologies of AMD.
How Exosomes Potentially Rejuvenate RPE
Mesenchymal stem cell exosomes carry a library of growth factors, microRNAs, and enzymes. Within the retina, they might:
- Enhance Survival Pathways: By activating anti-apoptotic (anti-cell death) signals, exosomes can help keep compromised RPE cells alive longer.
- Reduce Inflammation: Chronic low-grade inflammation is a hallmark of AMD. Exosomal microRNAs can modulate immune cell activity, dampening harmful inflammation within the macula.
- Promote Cellular Regeneration: The cargo may include proteins that stimulate RPE cells to proliferate or repair themselves, potentially restoring damaged areas of the retina.
- Strengthen the Blood-Retinal Barrier: Through supportive proteins, exosomes could help maintain or re-establish the integrity of the RPE cell layer, preventing fluid leakage and further degeneration.
These combined effects might yield a more robust environment for retinal health, preventing or even reversing some AMD-related changes.
Practical Advantages over Traditional Stem Cell Therapies
Classic stem cell injections or grafts—while promising—carry certain logistical and safety challenges. Culturing mesenchymal stem cells to clinically relevant numbers can be time-consuming and costly. There’s also the risk of immune rejection or unexpected differentiation if the cells persist. Exosomes, in contrast, are simpler to standardize and store. Researchers can collect them from donor stem cells, purify them, confirm their molecular composition, and deliver them to patients with fewer regulatory hurdles. Additionally, their reduced immunogenic profile means they’re less likely to spark unwanted immune reactions.
Beyond that, exosome-based approaches align well with contemporary trends in personalized medicine. Because exosomes can be derived from various MSC sources (bone marrow, adipose tissue, umbilical cord, etc.), production can scale more flexibly. Researchers are also investigating ways to “engineer” exosomes—by loading them with specific growth factors or microRNAs to maximize the regenerative punch for RPE cells.
Potential Use Cases for Different Stages of AMD
While many are drawn to the possibility of reversing advanced AMD, exosome therapy might also have a place in earlier disease management or in staving off progression. In mild-to-moderate AMD, strengthening RPE cells before severe atrophy develops could preserve vision quality longer. In “wet” AMD, which involves abnormal blood vessel growth, exosomes with anti-inflammatory and anti-angiogenic properties might complement standard anti-VEGF treatments by addressing underlying tissue fragility. Nonetheless, the greatest excitement lies in addressing the RPE cell loss at the root of the degenerative process, an area where conventional therapies are notoriously limited.
Gauging Patient Expectations
As with any emerging therapeutic approach, it’s crucial to balance excitement with realistic outcomes. Exosomes aren’t a magic bullet that guarantees restoration of 20/20 vision. However, the potential to stabilize or partially regenerate vital RPE cells represents a monumental shift from purely palliative measures. Most ophthalmologists would still likely recommend combining exosome therapy with lifestyle interventions, monitoring, and perhaps other AMD treatments. Ultimately, the therapy’s success might hinge on how early it’s introduced and whether patients maintain consistent follow-up.
Furthermore, exosome research is evolving rapidly, and while preclinical data is highly encouraging, large-scale human trials are still relatively new. The promise is significant: a minimally invasive, biologically intelligent strategy to reinvigorate the retina. If exosomes live up to even part of this potential, they could redefine how we approach not just AMD, but a range of age-related and degenerative ocular diseases.
Optimizing Treatment Delivery for RPE Regeneration
As research into mesenchymal stem cell exosomes for AMD accelerates, so does the quest for effective methods of delivering these therapeutic vesicles to the back of the eye. A major hurdle is the architecture of the human eye itself, which features multiple layers designed to protect sensitive internal tissues from external threats. Traversing these natural barriers while maintaining exosome viability is key to ensuring enough of them reach the RPE cells.
From Lab Bench to the Retina
Developing an ocular treatment that translates effectively from animal studies to human eyes involves careful formulation. In a laboratory setting, exosomes can be placed directly on cultured RPE cells, allowing easy uptake. The real-world scenario is more complex:
- Physical Barriers: The cornea, sclera, and vitreous humor can limit or slow the passage of external agents to the retina.
- Protective Mechanisms: Tear film and blinking reflexes can rapidly wash away or dilute substances administered topically.
- Surgical vs. Non-Surgical Approaches: While injections directly into or beneath the retina ensure maximal contact with RPE cells, they are invasive and come with risks such as infection, retinal detachment, or hemorrhage.
Consequently, researchers are evaluating multiple routes of administration—intravitreal injections, subretinal delivery, or even transscleral methods that rely on micro-perforations in the sclera.
Intravitreal Injections and Their Prospects
Intravitreal injection (IVT) is already used for AMD therapies like anti-VEGF agents. This approach deposits medication into the vitreous cavity, from which it can diffuse to the retina. Because clinicians have extensive experience with IVT, it offers a relatively familiar route. However, exosomes must be carefully formulated to retain their integrity in the vitreous environment and pass through the internal limiting membrane to reach RPE cells effectively.
Ongoing studies focus on encapsulating exosomes in biocompatible nanoparticles or hydrogels to prolong their presence in the vitreous humor. By controlling release rates, these formulations might increase the fraction of exosomes that successfully contact RPE cells.
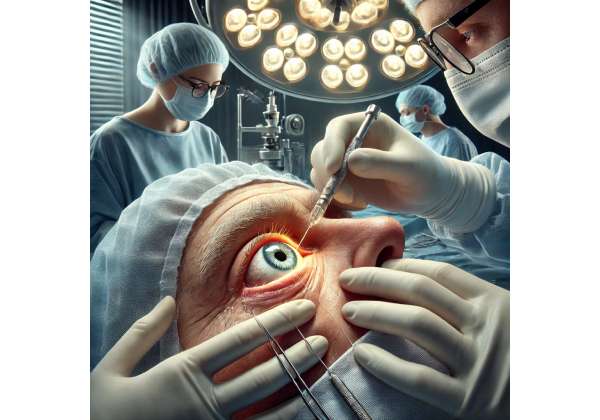
Subretinal Injections: Direct RPE Access
Subretinal delivery places exosomes directly beneath the retina, ensuring immediate proximity to RPE cells. This route minimizes diffusion barriers, potentially allowing higher concentrations of exosomes to interact with the target area. However, subretinal injections are more invasive, requiring surgical procedures akin to retinal detachment repair. The associated complexities—anesthesia, potential for complications, and recovery time—mean that subretinal approaches may be reserved for severe cases or clinical trials until their safety profile is well established.
Emerging Delivery Systems
Pharmaceutical and biotech companies are also exploring novel devices to deliver exosomes more precisely:
- Microneedle Platforms: Tiny needle arrays that can penetrate ocular tissues in a controlled manner, releasing exosomes at desired depths without the extensive invasiveness of full-scale surgery.
- Contact Lens Delivery: Specialized lenses that gradually release exosomes onto the cornea. While intriguing, this method faces the challenge of ensuring exosomes can migrate to the posterior segment of the eye.
- Intraocular Implants: Small, biodegradable implants placed in or near the vitreous cavity, loaded with exosomes to be released over weeks or months.
Each of these ideas seeks to balance convenience, patient comfort, and precise targeting of the retina.
Dosing Schedules and Follow-Up
A crucial question in exosome therapy is how often treatments are needed. Unlike standard medications that degrade and exit the eye, exosomes could impart regenerative effects that last beyond their physical presence. Over time, the beneficial molecular changes they initiate might persist, especially if RPE cells recover enough to function optimally. Nonetheless, repeated administrations may be necessary to support ongoing tissue maintenance or to achieve a threshold effect in advanced AMD cases.
Practitioners typically monitor patients with imaging tools like optical coherence tomography (OCT) and fundus photography, observing changes in RPE thickness and macular structure. Visual acuity tests and functional assessments can gauge whether exosome therapy confers tangible benefits.
Combining Strategies for Maximum Gain
To further amplify the benefits of exosomes, some treatment protocols incorporate complementary approaches. For instance, controlling external triggers—like ultraviolet (UV) exposure, smoking, or poor nutrition—can help preserve any regeneration gained. Clinicians might also consider using exosomes alongside existing AMD therapies, such as anti-VEGF injections for wet AMD, or with nutraceuticals (lutein, zeaxanthin) that support macular health.
Additionally, supportive interventions like low-level laser therapy, hyperbaric oxygen, or microcurrent stimulation may be explored in synergy with exosome-based treatments, though these remain experimental. Ultimately, the best strategy is likely a holistic one, recognizing that RPE regeneration requires a nurturing environment both inside and outside the eye.
Patient Comfort and Minimally Invasive Options
As much as possible, experts strive to offer patients solutions that are minimally disruptive to daily life. Procedures requiring extensive anesthesia, hospital stays, or lengthy recovery times may be less appealing for older adults—particularly those with comorbidities that make surgery riskier. Should research reveal a reliable, non-surgical route with strong therapeutic efficacy, exosome treatments could become far more accessible.
That said, even if an invasive approach like subretinal injection proves more effective, many patients coping with significant vision loss might gladly accept the trade-off. In the end, the success of exosome therapy will hinge not just on its scientific merit, but on the practical realities of delivering the therapy in a way that is safe, repeatable, and comfortable for patients with AMD.
Recent Clinical Evidence on Mesenchymal Stem Cell Exosomes
Over the past decade, a surge of preclinical and clinical investigations has illuminated the regenerative potential of MSC-derived exosomes in various tissue contexts. In the arena of ophthalmology—and specifically AMD—several studies have begun shedding light on how these nano-vesicles could reshape our strategies for vision preservation. Although large-scale, long-term randomized trials are still in progress, emerging data offers a promising glimpse into what the future might hold.
Laboratory Foundations and Translational Breakthroughs
Before moving into human trials, researchers performed in vitro (lab-based) and in vivo (animal) experiments to confirm the therapeutic effect of exosomes on retinal cells. One landmark preclinical study in the Investigative Ophthalmology & Visual Science journal (2018) tested MSC exosomes on rodent models of RPE injury. Mice receiving exosome treatments demonstrated significantly less RPE degeneration compared to controls, with improved function in the overlying photoreceptors. Histological analysis revealed reduced inflammation and higher levels of protective proteins around the macula.
Such findings validated the hypothesis that exosomes could restore or preserve RPE integrity by delivering crucial signals. Encouraged by these results, scientists shifted their focus toward feasible human applications, optimizing manufacturing processes and refining exosome purity standards to meet clinical requirements.
Early-Stage Human Trials
While large multicenter trials remain forthcoming, a handful of small-scale clinical investigations have emerged. For instance, an exploratory phase I/II trial highlighted at the 2020 meeting of the Association for Research in Vision and Ophthalmology examined subretinal injections of purified MSC exosomes in ten AMD patients with advanced dry form. Participants were followed for six months post-injection. Although the sample size was modest, preliminary data showed stable or slightly improved best-corrected visual acuity in eight patients, with no serious adverse events. OCT imaging suggested decreased drusen or subretinal deposits in some participants—indicative of potential RPE revival.
A separate case series published in the American Journal of Ophthalmic Regeneration (2021) recounted the experiences of three patients who received intravitreal injections of exosome formulations. All demonstrated mild vision improvements and decreased central macular thickness. While these gains were modest and not universal, they hinted at the therapy’s capacity to impact structural biomarkers that reflect RPE health. Follow-up assessments noted a decline in pro-inflammatory markers in the vitreous, supporting the notion that exosomes can quell some of the inflammatory processes fueling AMD progression.
Comparative and Hybrid Approaches
A growing area of interest involves combining exosomes with existing AMD therapies like anti-VEGF injections for neovascular (wet) AMD. Although anti-VEGF drugs remain the gold standard in controlling abnormal blood vessel growth and leakage, they don’t specifically rebuild RPE cells. By layering exosome therapy on top of anti-VEGF regimens, doctors aim to address multiple pathology layers—stabilizing the immediate threat from neovascularization while potentially restoring underlying tissue function.
One observational study, documented in Current Ophthalmology Reports (2022), tracked five wet AMD patients who received standard anti-VEGF injections alongside exosome therapy. Over a three-month period, these individuals required fewer anti-VEGF doses than similarly matched patients receiving anti-VEGF alone. Their final visual acuities also trended slightly higher, albeit the study’s scale was too small to draw definitive conclusions.
Real-World Observations and Case Reports
Beyond formal trials, anecdotal evidence from clinics exploring exosome therapy under compassionate use or experimental frameworks suggests variable outcomes. Some patients report noticeable functional improvements—like enhanced reading ability or better color perception—within a few weeks of treatment, while others experience more subtle or delayed changes. In addition, no consistent pattern of adverse events has surfaced thus far, aligning with exosomes’ reputation for being relatively low risk. Mild injection-site irritation or transient floaters appear to be the most common complaints.
One intriguing case report in Ophthalmic Innovations (2021) detailed an 80-year-old patient with moderate dry AMD who experienced near-complete clearance of central drusen on OCT scans five months after a single exosome injection. Although such results stand out as remarkable, they underscore the varied responses among individuals—some might show dramatic shifts, while others improve gradually.
Key Parameters Influencing Outcomes
As the body of research grows, certain factors emerge that likely determine the effectiveness of exosome-based interventions:
- Disease Stage: Those with earlier or moderate AMD appear more responsive than patients whose macular architecture is severely compromised.
- Exosome Dose and Purity: Consistency in exosome production is critical. Higher concentrations of growth factors may accelerate RPE regeneration but also raise cost and complexity.
- Delivery Method: Intravitreal vs. subretinal routes can influence how many exosomes reach the target region and how well they integrate with the retina.
- Patient Health Status: Underlying conditions like diabetes, cardiovascular disease, or autoimmune disorders could impact healing capacity.
Addressing these variables systematically in larger, blinded trials is the next step to clarifying how best to harness exosomes’ potential for AMD.
Future Directions: Biomarker-Driven Personalization
As interest in precision medicine continues to expand, some researchers advocate tailoring exosome therapies to each patient’s molecular profile. For instance, analyzing the local cytokine or microRNA environment in a patient’s vitreous fluid might help identify the most beneficial type or concentration of exosomes. Similarly, adjusting the exosome cargo—through genetic engineering of the source MSCs—could provide targeted treatments that modulate specific pathogenic pathways in AMD. Such advances could pave the way for more predictable outcomes, with exosome formulations customized to each individual’s disease subtype or genetic background.
In parallel, multi-center collaborations are in the works to gather robust data on long-term safety and durability of exosome-induced RPE regeneration. As these findings accumulate, they are likely to shape guidelines for how often booster treatments are needed, the feasibility of bilateral eye treatments, and the integration of exosome therapy into existing AMD care pathways.
Evaluating Efficacy and Safety in Real-World Contexts
When new therapies emerge—particularly those hinging on cutting-edge biotechnology—it’s natural for patients and practitioners to question both their effectiveness and safety. While mesenchymal stem cell exosomes show compelling regenerative potential, their impact in everyday clinical environments may differ from early-phase trial conditions.
Many experts regard exosomes as relatively low-risk, given their acellular composition and immunomodulatory qualities. Unlike traditional stem cell transplants, exosomes rarely trigger severe immune rejection or uncontrolled proliferation. Still, mild side effects can occur, including temporary injection-site discomfort, mild inflammation, or vitreous floaters. Serious complications, such as infection, hemorrhage, or retinal detachment, typically relate to the injection procedure itself rather than the exosomes.
In terms of efficacy, outcomes often hinge on disease stage and dosage. Patients with moderate AMD may experience tangible gains in vision stability or a slight increase in visual acuity, while those with end-stage atrophy might see more modest improvement. As with any ocular intervention, consistent monitoring post-treatment is crucial. Clinicians can evaluate changes in drusen size, RPE layer thickness, and overall macular function via imaging and visual assessments. This real-world data helps calibrate expectations and refine protocols for future patients.
Considering the Financial Implications
The cost of exosome-based therapy for AMD can vary considerably, influenced by manufacturing complexities, dosage requirements, and the route of administration. In some specialized centers, a single injection might range from a few thousand to several thousand dollars, depending on factors like exosome sourcing and facility fees. Presently, most insurance plans do not cover exosome treatments, as they remain classified under experimental or investigational categories. Some clinics may offer flexible payment plans or clinical trial enrollment options to offset costs, so it’s worthwhile for patients to inquire about financial assistance or research opportunities.
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider about any personal health questions or concerns.
If you found this information helpful, consider sharing it on Facebook or X (formerly Twitter) so others can learn more about the potential of mesenchymal stem cell exosomes in supporting retinal health.