Glaucoma is a complex eye condition often linked to elevated intraocular pressure (IOP), which can damage the optic nerve over time. For many individuals, standard therapies like medicated eye drops or filtration surgeries effectively control IOP. However, not everyone responds well to these interventions, and concerns about side effects or post-operative recovery sometimes lead patients to seek alternative solutions. In recent years, micropulse laser therapy has gained attention as a gentler, yet potent, approach to regulating eye pressure without the typical downsides associated with more invasive procedures.
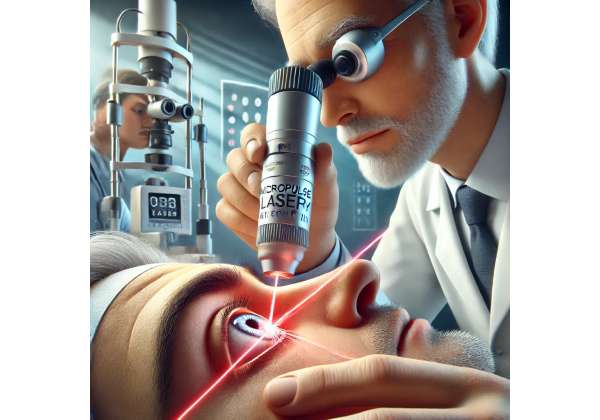
Many people are intrigued by this technology but may be unfamiliar with how it differs from conventional laser treatments. While older laser procedures have proven beneficial in certain cases, they sometimes carry a risk of long-term tissue damage. Micropulse technology, on the other hand, targets the same structures in a less disruptive manner. By breaking down the energy beam into smaller, pulsatile bursts, surgeons can achieve the therapeutic benefits of laser intervention while preserving surrounding tissue health. Below, we explore micropulse laser therapy in depth, including how it works, who might benefit, and the growing body of research highlighting its promise in modern glaucoma management.
Understanding the Potential of Micropulse Laser Therapy
Micropulse laser therapy, sometimes referred to by brand names like the “Cyclo G6” or using terms like “subthreshold laser,” relies on an idea that’s both deceptively simple and scientifically advanced. Instead of delivering one continuous beam of laser energy, the system rapidly pulses short, on-off intervals. Each pulse is carefully measured in microseconds, giving the tissue momentary breaks that allow heat to dissipate. This design aims to reduce the risk of collateral damage and scarring, making it distinct from traditional continuous-wave laser therapies.
Foundations of Laser in Glaucoma
To appreciate why micropulse emerged, it helps to review how traditional lasers are employed in glaucoma:
- Trabeculoplasty: A laser is applied to the trabecular meshwork, improving aqueous fluid outflow. These procedures include argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT). Although commonly done, repeated sessions may become less effective over time, and there’s potential for inflammation or scar tissue formation.
- Cyclodestructive Procedures: Used mainly for advanced, refractory glaucoma, continuous-wave lasers like Nd:YAG or diode devices ablate part of the ciliary body to decrease aqueous humor production. Despite success in lowering IOP, these treatments can lead to complications such as hypotony (overly low IOP) or tissue necrosis.
Micropulse technology grew out of a desire to harness the benefits of these cyclodestructive methods without the significant tissue destruction and side effects. By employing cyclical short pulses, the device can target the ciliary processes—the regions that secrete fluid within the eye—in a more controlled manner, potentially reducing the risk of permanent damage.
How the Micropulse Mechanism Works
When a micropulse laser is applied to the ciliary body (usually through the sclera, or white of the eye), the energy is segmented into bursts. Each burst raises the tissue temperature slightly but not enough to cause immediate thermal damage. The off-period between pulses allows the tissue to cool. Repeated pulses over a specific area can gently disrupt the cells involved in fluid production, thereby lowering IOP in a gradual, less traumatic way.
- Sublethal Thermal Impact: Because the tissue is not heated continuously, the risk of extensive scarring is minimized. This subthreshold approach may preserve more of the ciliary body’s function while still providing the necessary therapeutic effect.
- Controlled Inflammatory Response: In traditional laser surgeries, significant post-operative inflammation sometimes occurs. Micropulse can still induce mild inflammation—part of the body’s healing process—but it’s generally less intense, reducing the need for high-dose steroids or extended recovery times.
Advantages Over Conventional Methods
One of the biggest draws of micropulse laser therapy is its versatility. Patients at varying stages of glaucoma—mild, moderate, or advanced—may be candidates, though it’s particularly compelling for those who have not found success with eye drops or who have high surgical risks. Other potential benefits include:
- Less Pain and Faster Recovery: Many patients tolerate the procedure well, often requiring only topical anesthesia or mild sedation. They can typically resume normal activities soon after.
- Repeatable Approach: Unlike certain continuous-wave lasers that can cause cumulative tissue damage, micropulse treatments can be repeated more safely if IOP creeps back up. This offers a longer-term management solution for chronic conditions like glaucoma.
- Reduced Medication Burden: By achieving meaningful drops in IOP, micropulse therapy can sometimes help patients reduce their reliance on multiple daily eye drops—a welcome improvement in convenience and treatment adherence.
- Preservation of Overall Ocular Integrity: Because the therapy is more tissue-friendly, it often preserves the eye’s structural integrity better, potentially lowering the risk of complications like persistent hypotony or leaks.
Suitability for Different Glaucoma Variants
Micropulse laser therapy primarily focuses on lowering intraocular pressure by modulating ciliary body function. This approach can be relevant for multiple glaucoma subtypes:
- Primary Open-Angle Glaucoma (POAG): The most common form, where fluid outflow is impeded gradually. By decreasing fluid production, micropulse laser may enhance the overall outflow dynamics.
- Angle-Closure Glaucoma: Patients with narrow angles might benefit if other interventions fail or if they cannot undergo certain filtering surgeries due to comorbidities.
- Secondary Glaucomas: Conditions like uveitic glaucoma, steroid-induced glaucoma, or neovascular glaucoma may also see improvement, although care must be taken to address underlying causes.
- Refractory or End-Stage Glaucoma: Individuals who have undergone previous surgeries or exhausted medical options might find micropulse beneficial in stabilizing or further reducing IOP.
Considerations and Precautions
While micropulse therapy is generally safer, it isn’t devoid of potential complications or limitations:
- Partial Efficacy: Some patients might not achieve the desired IOP reduction, necessitating multiple sessions or adjunctive treatments.
- Visual Acuity Concerns: Although less common, a minority may experience transient vision fluctuations or mild discomfort during the recovery phase.
- Anatomical Challenges: Thick sclera, unusual eye shape, or scarring from prior surgeries can impede effective laser delivery.
- Ongoing Monitoring: As with all glaucoma procedures, regular follow-up is essential to confirm that the therapy is working and to detect any late complications.
Micropulse laser technology continues to evolve, with refinements in probe design, energy settings, and treatment protocols. In many specialized clinics, it’s transitioning from a last-resort measure to a front-line or second-tier therapy for those with moderate to advanced glaucoma. Growing acceptance among ophthalmologists and a robust pipeline of ongoing research bode well for micropulse therapy’s future. For anyone looking to minimize surgical risk or medication dependence, discussing micropulse laser with an eye specialist can offer fresh insight into a safer, effective way to keep glaucoma in check.
How This Laser Approach Is Used in Practice
Micropulse laser therapy doesn’t have to be a complicated process, but it does require careful planning and expertise. Understanding how and why it’s applied can provide reassurance to patients contemplating the procedure. Below is a look at the general steps and common protocols guiding micropulse treatments for glaucoma.
Step-by-Step Guide to the Procedure
- Preoperative Assessment:
Before any laser session, an ophthalmologist will conduct a thorough exam, measuring IOP, assessing visual fields, and possibly using imaging tools like optical coherence tomography (OCT) to understand the eye’s anatomy. If micropulse therapy seems appropriate, patients might stop certain eye drops (like prostaglandins) a few days before treatment, though instructions vary among clinics. - Anesthesia and Preparation:
In most cases, the procedure is done on an outpatient basis under topical anesthesia—eye drops that numb the surface of the eye. Patients are typically awake, with only mild sedation if they feel anxious. The eye is then prepped with a coupling solution that helps the laser energy pass through the sclera more effectively. - Laser Delivery:
The surgeon uses a specialized probe (often shaped like a pen or handpiece) designed to position the laser energy over the ciliary body area. This part of the eye is located behind the iris, so external landmarks guide the treatment zones. With micropulse mode engaged, the laser pulses in rapid bursts, usually applied in a slow arc around the sclera for a set duration. Some protocols specify 100–200 seconds of total laser “on” time, broken into segments. - Completion and Immediate Aftercare:
Once the set dose is delivered, the eye is gently rinsed, and a topical antibiotic or anti-inflammatory drop may be administered. Patients can rest briefly, then return home the same day. Most experience little to no discomfort aside from mild irritation, typically managed with artificial tears or short-term anti-inflammatory drops.
Typical Dosages and Settings
Micropulse laser systems typically rely on diode lasers with a wavelength of around 810 nm. However, the exact energy levels and time settings can vary. Ophthalmologists might customize the pulse duration (e.g., 0.5 ms on, 1.1 ms off) and total passes over each quadrant based on factors like:
- Patient’s Baseline IOP and Target IOP
- Severity of Glaucoma
- Previous Laser History
- Surgeon’s Comfort and Experience
Each pass aims to deliver enough energy to slow fluid production without over-treating and risking hypotony. Adjusting these parameters is part of the “art” of micropulse therapy, balancing efficacy against unwanted side effects.
Single vs. Repeat Treatments
An advantage of micropulse laser is the ability to repeat sessions if necessary. For instance, a patient may see a modest drop in IOP initially but require a second or third application several months later to reach optimal levels. This flexibility sets it apart from some continuous-wave lasers that carry a higher risk of cumulative tissue damage if performed multiple times. Typically, clinicians wait at least 8–12 weeks to gauge the full effect before deciding on additional treatment.
Adjunctive Role with Medications
Even if micropulse effectively lowers IOP, many patients remain on at least one or two eye drops, especially if they had advanced disease. The procedure’s main goal might be to reduce the medication burden rather than eliminate it entirely. When significant synergy is needed, micropulse can pair with other interventions like minimally invasive glaucoma surgery (MIGS) or filtration operations. The sequence—whether to do micropulse first or MIGS first—often depends on the patient’s unique presentation.
Post-Treatment Follow-Up
Follow-up visits usually occur within the first week, then at 1 month and 3 months post-procedure. During these exams, the ophthalmologist measures IOP, checks for any rebound spikes, and looks for signs of inflammation. Some patients receive short-term steroid drops or non-steroidal anti-inflammatory drugs (NSAIDs) to calm any mild irritation. If a patient’s IOP remains stable and vision is good, subsequent check-ups might extend to 6 months or longer.
Managing Potential Complications
Although micropulse is gentler than traditional laser ablation, minor complications can still arise:
- Transient Blurred Vision: The eye might feel blurry for a few days, but it usually resolves.
- Mild Eye Redness or Discomfort: Over-the-counter lubricants often help, and significant pain is rare.
- Pressure Spikes or Drops: While uncommon, a short-lived IOP rise can occur if the eye becomes inflamed. Conversely, if the laser effect is robust, some individuals could experience a bigger-than-expected drop in IOP, though it’s generally not as dramatic as with older cyclodestructive techniques.
- Inadequate Response: If IOP remains high after 2–3 months, either a higher dose of micropulse or an alternative treatment might be considered.
Overall, most patients find micropulse therapy seamless and straightforward. Recovery is faster than many surgical options, and the risk of scarring or serious complications is notably lower. By following the ophthalmologist’s post-procedure instructions and attending regular check-ups, patients can optimize their chances of success, whether micropulse is used as a standalone therapy or part of a broader, integrated approach to glaucoma care.
Looking at the Evidence and Real-World Outcomes
Micropulse laser therapy may sound promising, but how does it stack up in clinical research? Over the past decade, multiple studies and real-world data analyses have provided insights into its effectiveness, safety, and overall place in the glaucoma treatment landscape.
Landmark Clinical Trials and Observational Studies
- Initial Feasibility Research (Ophthalmology Journal, 2012): Early feasibility investigations introduced the concept of subthreshold diode laser therapy. In a group of 40 patients with refractory glaucoma, micropulse therapy reduced IOP by an average of 30% at the 6-month mark. Complication rates were minimal, and only a few participants reported post-operative pain exceeding mild levels.
- Prospective Study on Micropulse Diode Laser (American Journal of Ophthalmology, 2015): A larger prospective trial enrolled 80 subjects who were either poor candidates for incisional surgery or had already undergone multiple procedures. Participants received micropulse in a standardized setting of 100 seconds per hemisphere. At the 1-year follow-up, about 70% achieved at least a 20% reduction in IOP with stable or improved visual acuity. The authors noted fewer inflammatory sequelae compared to historical data on continuous-wave transscleral cyclophotocoagulation (TSCPC).
- Comparative Analysis Against Traditional Lasers (Clinical Glaucoma Practice, 2018): Investigators compared micropulse cyclophotocoagulation (mCPC) to conventional diode laser therapy for advanced glaucoma. The micropulse group reported higher satisfaction and less post-op pain. While both modalities effectively lowered IOP, the micropulse approach required fewer rescue medications over 9 months of follow-up, suggesting a more durable impact.
Real-World Insights
Beyond formal trials, clinicians worldwide have embraced micropulse, generating observational data that underscore its practicality. Ophthalmology practices often share case reports illustrating how micropulse therapy allowed certain complex glaucoma patients—some with multiple prior failed surgeries—to stabilize their IOP without proceeding to more invasive procedures. Notably:
- Suitability for Elderly or Medically Frail Patients: Because the procedure involves minimal trauma and can be done under local anesthesia, older patients with systemic comorbidities often find it safer than standard incisional surgeries. Real-world registries reflect a growing number of such patients opting for micropulse with favorable outcomes.
- Efficacy in Secondary Glaucomas: Secondary glaucoma from steroid use or inflammation (e.g., uveitic glaucoma) can be particularly challenging to treat. Case series reveal that micropulse can significantly reduce steroid requirements and maintain lower IOP in these groups, potentially staving off more aggressive surgical interventions.
- Long-Term Sustainability: Although some critics worry about IOP drifting upward over time, many case reports highlight stable pressure control 1–2 years post-procedure. Occasional top-up laser sessions can bolster these results if modest rises occur.
Patient Profiles Showing Greatest Benefit
Data suggest that while micropulse can be widely applied, certain profiles show particularly robust results:
- Moderately Advanced Glaucoma: Those with moderate nerve damage who cannot tolerate further medication or who have mild to moderate field loss often achieve consistent outcomes.
- High Surgical Risk: People with cardiovascular or respiratory issues, where general anesthesia or incisional surgery poses extra risk, appreciate the less invasive nature of micropulse.
- Add-On to MIGS or Prior Surgeries: In patients who have had MIGS devices (e.g., iStent or Hydrus) placed, but still register elevated IOP, micropulse can fine-tune the ocular pressure management.
- Pediatric or Youthful Patients: Although less frequently studied in children, anecdotal experiences indicate micropulse may spare younger patients from multiple incisional surgeries, though further large-scale pediatric research is needed.
Comparing Outcomes to Incisional Surgeries
Traditional glaucoma surgeries like trabeculectomy or tube shunts can dramatically lower IOP but come with higher complication rates (e.g., bleb leaks, hypotony, infection risks). Studies placing micropulse therapy side by side with these procedures highlight a less dramatic but still meaningful drop in IOP, achieved with fewer severe adverse events. This trade-off appeals to those seeking a mid-range solution: stronger than eye drops or conventional laser trabeculoplasty, but less invasive than full-blown surgery.
- Trabeculectomy vs. Micropulse: Although trabeculectomy can yield IOP levels in the low teens or single digits, the risk of infection or bleb failure is not negligible. Micropulse, while sometimes yielding pressure in the mid-teens to high teens, offers a safer risk profile and faster return to daily life.
- Tube Implants vs. Micropulse: Shunts are often reserved for complicated or refractory glaucoma. Some real-world case series show that micropulse can defer the need for a tube in a significant fraction of patients, especially if repeated sessions are employed.
Incorporating Advances in Technology
As micropulse technology gains traction, device manufacturers continue refining energy delivery systems. Upgraded handpieces with improved contact sensors or better heat dissipation are in development. Some research teams are exploring synergy with advanced imaging like ultrasound biomicroscopy to guide laser placement, ensuring the ciliary body is optimally targeted. Future directions may include:
- Personalized Laser Settings: Adapting energy levels to a patient’s scleral thickness or baseline ciliary body morphology.
- Combination with Pharmacological Agents: Pairing micropulse with anti-fibrotic drugs to further minimize inflammation or scarring.
- Real-Time Feedback Mechanisms: Implementing sensors that read tissue responses during treatment, fine-tuning energy pulses on the fly.
Key Research Takeaways
Across both structured trials and everyday clinical practice, a consensus emerges: micropulse laser therapy offers a compelling balance of efficacy and safety for patients with mild to advanced glaucoma who either cannot or do not wish to endure more invasive operations. While it may not replace well-established surgeries in the most severe or highly refractory cases, it often extends the window of time before incisional interventions become necessary.
Additionally, it stands out for its repeatability: patients who experience partial success can easily undergo a second or third session without accumulating the same risk of scarring and tissue damage typical of continuous-wave lasers. With ongoing refinements and larger-scale randomized trials in progress, micropulse therapy looks poised to become a mainstay in the modern glaucoma treatment toolkit, offering flexibility for a broad swath of patient needs.
Weighing the Efficacy and Potential Risks
Micropulse laser therapy is generally recognized for providing moderate but meaningful reductions in intraocular pressure. Many patients see IOP drops ranging from 20% to 40% compared to baseline, though individual responses can vary. For those who are good candidates, the procedure can deliver a stable, long-term solution or serve as a bridge before more definitive surgery. Despite these advantages, it’s crucial to keep expectations realistic: not everyone hits their target pressure with micropulse alone, and adjunctive medications or repeated treatments may remain necessary.
From a safety standpoint, micropulse’s design inherently aims to minimize damage to ocular tissues. Transient side effects—mild eye discomfort, temporary visual haze—are relatively common but tend to resolve quickly. Serious complications, such as persistent hypotony or severe inflammation, are rare but can occur, especially if the energy settings are excessively high or the patient has other complicating ocular pathologies. Proper technique and post-procedure monitoring help mitigate these risks. Overall, micropulse offers a more conservative profile than older cyclophotocoagulation methods, a distinction that draws many ophthalmologists and patients to consider it as a primary laser choice.
What to Expect in Terms of Pricing
Costs for micropulse laser therapy can differ widely based on geographic region, clinical setting, and insurance coverage. In the United States, a single session might range from \$1,500 to \$2,500 if paying out of pocket. Many private insurance plans and Medicare will cover portions of the procedure, especially if it’s deemed medically necessary due to uncontrolled glaucoma. Outside the U.S., prices depend on local healthcare policies and currency rates, but the therapy generally falls somewhere between the cost of standard laser trabeculoplasty and more invasive operations. It’s advisable to verify insurance reimbursements and any necessary pre-authorizations prior to scheduling the treatment.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider regarding personal health questions or decisions.
If you found this information useful, please consider sharing it on Facebook or X (formerly Twitter) so others can learn more about micropulse laser therapy as a promising option in glaucoma management.










