Retinal vein occlusion (RVO) is a serious eye condition in which the veins responsible for draining blood from the retina become blocked, leading to swelling, fluid leakage, and potential vision loss. Depending on whether the main central vein or smaller branch veins are affected, RVO is categorized as central retinal vein occlusion (CRVO) or branch retinal vein occlusion (BRVO). For many patients, the most noticeable sign might be blurry vision or dark spots in their field of sight, sometimes appearing suddenly. In severe cases, daily tasks such as reading or driving can quickly become challenging.
Modern ophthalmology offers several treatment approaches, including anti-VEGF injections and laser interventions, to help control complications like macular edema and neovascularization. One innovative technology receiving growing attention is micropulse laser therapy. Unlike conventional lasers, which emit a continuous beam, micropulse breaks the energy into bursts, potentially lessening tissue damage while still delivering targeted benefits. Below, we explore how this treatment works, its potential advantages, and the supporting research that indicates a promising role for micropulse laser therapy in managing retinal vein occlusion.
A Closer Look at Micropulse Laser for RVO
Understanding the Rationale Behind Laser Therapy
Laser treatment has historically been a cornerstone of retinal care, particularly for complications stemming from vascular disorders such as diabetic retinopathy or RVO. Standard photocoagulation lasers create thermal burns in the retina, sealing off leaking vessels and reducing fluid buildup. While often effective, this method can damage adjacent retinal tissues and cause scarring, which sometimes translates into reduced peripheral or night vision.
Micropulse laser therapy arose to tackle one core issue: the detrimental heat buildup associated with continuous-wave lasers. By pulsing energy on and off in microsecond intervals, micropulse technology aims to keep overall tissue temperature lower. This approach seeks to minimize scarring while still prompting beneficial cellular responses. For patients with RVO, where edema (swelling of the macula) significantly impairs central vision, micropulse laser can potentially reduce fluid accumulation without creating extensive thermal injury.
Differentiating Micropulse from Conventional Lasers
In conventional retinal laser photocoagulation (for example, grid or focal laser treatment in macular edema), the laser’s energy is delivered in a continuous wave that heats localized regions of retinal tissue. The subsequent thermal impact can help close leaking microaneurysms or abnormal vessels, but it may also lead to collateral harm.
Micropulse, on the other hand, divides this continuous energy into discrete pulses separated by “off” periods, which last long enough to allow partial cooling. This method—often described as “subthreshold”—means the retina does not sustain the same degree of burn or discoloration typically seen in standard photocoagulation. Some physicians even characterize micropulse as more of a “bio-stimulatory” process rather than a destructive one. The result is often less visible scarring, reduced patient discomfort, and a potentially faster recovery.
How Micropulse May Assist in RVO
Retinal vein occlusion frequently leads to increased vascular pressure, fluid leakage, and macular edema. Swollen retinal layers compromise visual acuity. Micropulse laser therapy may help in two main ways:
- Enhancing Fluid Clearance: The heat from the laser pulses, even at subthreshold levels, can stimulate retinal pigment epithelium (RPE) cells to pump fluid more efficiently out of the retina. By supporting these natural “pumps,” macular edema might be alleviated.
- Reducing Cytokines and Inflammatory Markers: Some studies suggest that micropulse energy, delivered at carefully calibrated levels, may modulate local inflammatory processes. This could help stabilize or regress fluid leakage over time, potentially decreasing the reliance on repeated anti-VEGF injections.
Clinical Scenarios Where It Shines
Micropulse laser therapy is commonly considered for patients experiencing persistent edema or who are not candidates for frequent intravitreal injections due to systemic health or personal considerations. It can serve as either a primary or adjunct treatment strategy alongside anti-VEGF drugs:
- Adjacent to Anti-VEGF Injections: Some retina specialists employ micropulse to reduce injection frequency, believing that improved fluid control might lengthen the interval between injections.
- Resistant or Recalcitrant Edema: In cases where standard therapies have produced limited results or a partial response, micropulse may add an extra layer of fluid management.
- Patient-Specific Considerations: Individuals with cardiovascular issues or a strong aversion to frequent invasive procedures might appreciate a non-injection-based method for controlling macular edema.
Potential Benefits Over Traditional Approaches
- Minimal Tissue Damage: The subthreshold design targets retina tissues in short bursts, limiting the risk of permanent scarring or chorioretinal atrophy that can occur with continuous-wave lasers.
- Repeatability: Because micropulse is gentler, repeated sessions pose a lower risk of cumulative retinal harm. This is especially relevant for chronic conditions like RVO that might need ongoing management.
- Synergy with Other Treatments: Micropulse does not generally conflict with anti-VEGF or steroid regimens. Instead, it can complement them, aiming to yield a more sustained reduction in swelling.
- Possible Cost and Convenience Benefits: For patients who respond favorably, micropulse therapy may reduce the frequency of intravitreal injections, which can lower both costs and time spent at medical appointments.
Limitations and Considerations
Despite the enthusiasm surrounding micropulse therapy, it’s crucial to note that results can vary. Some patients might see modest or no improvement, especially in severe or longstanding retinal vein occlusions where extensive ischemia has compromised retinal function. The technique demands skillful execution and individualized settings (power, duration, duty cycle) based on each patient’s disease severity and anatomical nuances. Overly aggressive parameters could still risk damaging the retina, while insufficient energy might fail to deliver meaningful therapeutic benefits.
Moreover, micropulse laser therapy doesn’t negate the potential need for anti-VEGF therapy altogether. Many patients discover that combining both methods yields the most effective control of macular edema. In such scenarios, micropulse is part of an integrated care plan rather than a standalone cure.
Evolving Role in Retinal Care
A decade ago, micropulse technology was still considered experimental by many specialists. Today, it’s rapidly finding a place in mainstream retinal practice for various conditions, from diabetic macular edema to RVO-related swelling. Continued research is refining technique protocols—identifying optimal pulse durations, cycles, and patterns to maximize fluid reduction while safeguarding healthy retinal structures. The synergy between micropulse and newer drug therapies also remains an area of active investigation.
For those affected by retinal vein occlusion, the prospect of a targeted, low-damage therapy that may preserve or even enhance vision is undeniably compelling. As with any medical decision, the choice to pursue micropulse laser therapy should be made in consultation with a retina specialist, taking into account disease status, personal treatment preferences, and the possible need for combination therapy. Yet, as evidence mounts, micropulse stands as a valuable addition to the arsenal of treatments aiming to restore or maintain sight in individuals with RVO.
Steps in Administering Micropulse Laser
Treating RVO with micropulse laser therapy requires careful planning, accurate execution, and structured follow-up. Although the procedure itself tends to be brief, both patient preparation and post-treatment measures play a critical role in optimizing visual outcomes.
Pre-Treatment Preparations and Assessments
- Comprehensive Ophthalmic Exam:
Before considering micropulse therapy, a retina specialist conducts a thorough examination. This likely includes dilated funduscopy, measuring visual acuity, and obtaining optical coherence tomography (OCT) scans to assess macular thickness. Fluorescein angiography or OCT angiography may also be utilized to evaluate the extent of capillary non-perfusion or the presence of microaneurysms. These findings shape the treatment plan, confirming whether micropulse is suitable and pinpointing where to concentrate the laser. - Setting Realistic Goals:
Because micropulse therapy aims to reduce edema rather than physically remove blockages, patients should understand that the laser won’t dissolve clots in the retinal vein. Instead, it helps the retina better manage fluid leakage and reduce swelling. Clear communication about the potential for multiple sessions or adjunct treatments (like anti-VEGF injections) fosters better patient satisfaction and adherence. - Medication Review:
Some specialists prefer adjusting or stopping certain eye drops or systemic medications prior to laser treatment. For instance, if a patient is already on steroid drops for uveitis, the physician may coordinate usage to minimize the risk of steroid-induced elevations in intraocular pressure. Pre-existing comorbidities like poorly controlled diabetes or hypertension may need optimization to ensure the best therapeutic effect.
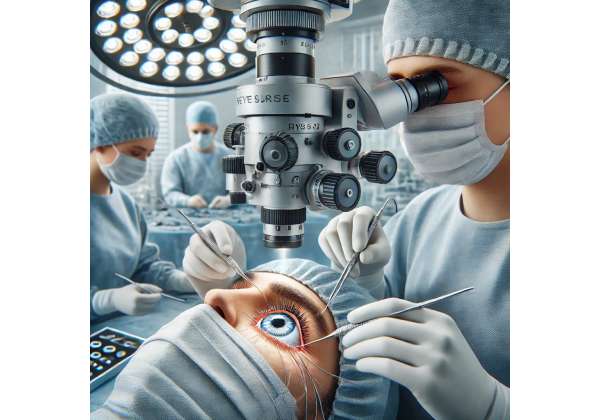
The Treatment Environment
Micropulse laser therapy is generally performed in an outpatient setting, often within a laser suite or specialized procedure room. On the day of treatment:
- Topical Anesthesia:
Eye drops are administered to numb the eye surface. The patient remains awake, typically with minimal discomfort. A contact lens or specialized laser lens is placed on the eye to focus and stabilize the laser beam accurately. - Laser Settings:
Micropulse laser devices allow customization of power, duration, duty cycle (proportion of “on” time within each pulse cycle), and spot size. Many protocols revolve around a 10-15% duty cycle and moderate power levels, although each retina specialist tailors parameters based on personal experience and the condition at hand. The objective is to deliver a subthreshold dose that triggers beneficial changes without creating visible burns. - Laser Application:
The surgeon carefully targets areas of edema or leaking microvasculature in the macula, often guided by prior angiographic or OCT findings. Each session might last just a few minutes as multiple laser spots or sweeps are delivered. The patient typically sees flashes of light but should not feel significant pain. If any discomfort arises, additional anesthetic drops can be applied. - Immediate Post-Session Check:
Following therapy, the lens is removed, the eye is irrigated if necessary, and a quick evaluation is done to ensure no acute complications, like increased intraocular pressure. Some specialists may provide a mild steroid or NSAID drop to calm inflammation.
Post-Treatment Care and Monitoring
- Symptom Management:
Patients often leave the clinic with minimal irritation. Mild redness or slight grittiness in the eye might occur but usually resolves within a day or two. Artificial tears or prescribed drops can ease any dryness or transient discomfort. - Follow-Up Appointments:
The retina specialist schedules follow-ups—often around 4-6 weeks after treatment—to review visual acuity and repeat OCT imaging. This allows for an assessment of macular thickness changes and any potential fluid reaccumulation. If improvements are modest or edema persists, a second micropulse session or complementary therapy may be considered. - Retreatment Protocols:
Because micropulse therapy’s effect can be cumulative and less destructive, repeated sessions may be performed if clinical signs warrant. However, it’s typical to wait until at least one or two follow-up OCT checks confirm the therapy’s initial impact (or lack thereof) before deciding on additional laser. - Integration with Other Therapies:
If patients remain prone to macular edema or experience repeated bouts of swelling, the physician might incorporate anti-VEGF injections, intravitreal corticosteroids, or other interventions. With micropulse, one benefit is that it usually doesn’t limit or complicate subsequent use of other treatments. This synergy is valuable in chronic or refractory cases.
When to Adjust or Adapt Approaches
While micropulse often yields favorable outcomes, certain situations call for alternative or supplementary steps:
- Minimal Response After Multiple Sessions:
If the patient’s macular thickness remains high or visual gains are lacking despite two to three micropulse treatments, the specialist may pivot to more traditional laser methods or intensify medical therapy. - Excessive Inflammation or Unstable Retinal Condition:
Rarely, some eyes react with significant inflammation or show signs of vitreous hemorrhage if the RVO is complicated. In these cases, more urgent interventions—like vitrectomy—might be necessary, overshadowing micropulse as a first line. - Recurrent Edema from Comorbidities:
In individuals with poorly controlled systemic factors (e.g., high blood pressure, abnormal cholesterol levels), better systemic management can enhance laser therapy’s impact. Persistent or severe macular edema may reflect an unmet systemic need.
Recovery Timeline and Expected Outcomes
Micropulse laser therapy is considered a relatively gentle procedure. Many patients resume everyday activities quickly, sometimes the same day if they aren’t experiencing sedation or discomfort. Visual changes, if any, tend to be subtle at first. Over subsequent weeks, as the retinal layers equilibrate, fluid can diminish, potentially revealing improvements in clarity or reading ability. Yet it’s important to remember that RVO is often a long-term management issue; success hinges on consistent monitoring, timely additional treatments, and proactive care of one’s overall vascular health.
In essence, micropulse therapy for RVO tries to strike a balance between laser’s proven capacity to stabilize leaky vessels and the desire to preserve as much healthy retinal tissue as possible. The structured, precise approach to delivering subthreshold energy underscores a broader shift in ophthalmology: harnessing advanced technology to refine existing interventions, reduce side effects, and help patients achieve better visual preservation in the face of chronic, potentially sight-threatening diseases.
Unveiling the Clinical Evidence and Observational Insights
Micropulse laser therapy’s traction in the realm of retinal vein occlusion is owed in large part to studies evaluating its safety, efficacy, and application procedures. While the technology initially saw widespread adoption in diabetic macular edema (DME), its principles naturally extended to macular edema from RVO. As a result, multiple investigators have examined how micropulse compares to conventional laser or injection-only regimens. Below, we delve into key findings, interesting data, and the real-world lessons gleaned from both formal research and everyday clinical practice.
Early Foundations in Diabetic Macular Edema
The earliest published experiences with micropulse date back to efforts in DME management. In the American Journal of Ophthalmology (2010), a small trial showcased that subthreshold micropulse led to comparable or better fluid reduction compared to standard photocoagulation, with fewer laser burns. Although not directly assessing RVO, this evidence laid the groundwork: if micropulse could preserve more retina while controlling edema in diabetes, the same approach might translate effectively to other vascular diseases like RVO.
Dedicated RVO Investigations
- Randomized Prospective Trial (Retina Journal, 2015):
One of the first direct RVO-centric micropulse studies enrolled 60 patients with BRVO and persistent macular edema. Participants were divided into two groups: one received micropulse alone, and the other had conventional continuous-wave laser. At the 6-month point, both groups showed a statistically significant reduction in central macular thickness, but the micropulse group experienced less scarring and subjectively reported fewer visual disturbances like night-vision difficulty. This trial was a milestone, suggesting micropulse’s gentler approach didn’t sacrifice efficacy. - Comparative Cohort with Anti-VEGF (Ophthalmic Research, 2017):
As anti-VEGF injections are standard in RVO management, another study sought to compare micropulse plus reduced-frequency anti-VEGF to anti-VEGF monotherapy in CRVO patients. Over a 12-month follow-up, those who combined micropulse with injections required fewer injections overall—on average, 30% fewer—and their final visual acuities were on par with the monotherapy group. While not a large sample, this data hinted that micropulse might effectively serve as an adjunct, lowering the burden of repeated injections. - Branch RVO Real-World Analysis (British Journal of Ophthalmology, 2019):
A retrospective study reviewed 90 patients with BRVO-induced macular edema. About half were managed with micropulse as a first-line laser approach, whereas the others underwent standard grid laser therapy. Six months post-treatment, the micropulse cohort exhibited slightly better improvement in best-corrected visual acuity (BCVA) and fewer complications, reinforcing that the technique is clinically feasible and potentially superior in vision outcomes.
Data on Long-Term Outcomes
Retinal vein occlusion, particularly in older adults, is often chronic. Knowing how micropulse therapy stands up over multiple years is crucial. Some observational follow-ups have documented stable edema control at 24 months for many patients. While not every person maintains dryness of the macula, re-treatment with micropulse or combination therapy can sustain functional gains without introducing significant laser-induced scarring. This long-term perspective is critical for conditions like CRVO or BRVO where recurrences of swelling can be expected.
Key Observations from Case Reports and Smaller Series
- Refractory Cases Finding Hope:
Multiple case studies detail patients who, despite monthly injections for RVO-related edema, saw minimal improvement. Upon adding micropulse, these individuals experienced a notable decline in central macular thickness and fewer monthly injections. Although anecdotal, such results illustrate micropulse’s potential in recalcitrant disease. - Flexibility in Laser Parameters:
Different retina centers reported success using a variety of subthreshold protocols—some employing lower power and more passes, others using slightly higher power but fewer passes. The uniform thread is that micropulse’s off-cycles allow for safe customization. This flexibility helps adapt treatment to each patient’s unique anatomy and disease severity. - Minimal Systemic Risk:
Because micropulse is purely localized to the retina, it doesn’t introduce the systemic side effects possible with repeated high-dose steroids or certain anti-VEGF agents (though anti-VEGF systemic effects are generally low risk). Patients who are elderly or who have multiple comorbidities might welcome this aspect of micropulse.
Emphasizing Combination Therapy
It’s increasingly clear that micropulse doesn’t necessarily aim to replace anti-VEGF or steroid injections. Instead, many protocols revolve around synergy:
- Rescue Approach: Initiate with anti-VEGF for quick edema resolution, then follow up with micropulse to maintain dryness.
- Maintenance and Injection-Sparing: For patients stable on monthly or bimonthly injections, a session or two of micropulse may extend intervals between shots.
- Sequential Strategy: Some specialists hold micropulse until partial regression from injections is achieved, then treat any residual fluid or microaneurysms. This can help target localized pockets of leakage in the macula.
By leveraging micropulse in tandem with pharmacologic solutions, retina specialists can adopt a more personalized, stepwise approach—fostering better outcomes and possibly lowering financial and logistic burdens.
Patients Who May Benefit Most
Based on current data, the best candidates typically:
- Have Edema that is Mild to Moderate: If the macula has massive fluid retention or severe ischemia, micropulse alone may be insufficient.
- Demonstrate Partial Response to Injections: These individuals can gain extra dryness from micropulse, potentially letting them space out injection visits.
- Desire Minimally Invasive Options: Some patients are averse to frequent needles or have difficulty adhering to injection schedules due to travel, finances, or other barriers.
- Present at an Earlier Stage of RVO: Timely intervention, before extensive photoreceptor damage, often correlates with more favorable laser outcomes.
Counterpoints and Research Gaps
While existing evidence is largely positive, there remain points to clarify:
- Optimal Parameter Consensus: Studies vary in recommended power settings, pulse duration, and coverage area. Establishing best-practice protocols can reduce outcome variability.
- Retinal Sensitivity Measures: Some investigators suggest that micropulse preserves more normal photoreceptor function, but robust data measuring this effect with microperimetry or advanced imaging remain limited.
- Head-to-Head Trials vs. Emerging Treatments: As new extended-release implants or combination drug therapies appear on the horizon, direct comparisons to micropulse can better delineate each option’s role.
Nevertheless, the consistent theme across published works is that micropulse is a valuable tool for controlling macular edema secondary to RVO. Through a less destructive mechanism than traditional lasers, it improves or stabilizes vision for many, particularly when integrated into a broader, carefully monitored plan.
Looking Ahead
Ongoing clinical trials are refining micropulse technology even further. Some research explores whether adjusting duty cycles or combining micropulse with advanced imaging guidance can amplify success rates. The concept of micropulse “neuroprotective” properties is also being investigated, suggesting that beyond fluid reduction, the subthreshold laser might support healthier retinal cell metabolism. Although these lines of inquiry remain in earlier phases, they underscore a future where micropulse could do more than just reduce swelling—it might also help preserve or restore retinal function at a cellular level.
In sum, the body of research backing micropulse laser therapy for RVO continues to grow, revealing an approach that merges efficacy with safety and repeatability. Real-world clinics are adopting it as part of a multi-modal strategy, and patient outcomes generally affirm the technology’s practical value. As additional studies refine protocols and expand the evidence base, micropulse therapy’s niche in RVO management looks poised to solidify further—offering renewed hope for individuals battling this sight-threatening vascular issue.
Safety Profile and Expected Results in Practice
Micropulse laser therapy is designed to limit collateral retinal damage by delivering laser energy in short, controlled bursts rather than a continuous beam. This subthreshold approach has proven to be relatively safe:
- Reduced Risk of Permanent Retinal Scarring: Because the energy is gentler and allows tissue cooling between pulses, visible burns on the retina occur far less frequently than with traditional photocoagulation.
- Minimal Pain or Discomfort: Most patients describe only mild sensations of warmth or see brief flashes of light. The procedure rarely requires sedation beyond topical anesthetic drops.
- Temporary Blurriness or Irritation: Immediately post-procedure, mild inflammation or transient visual haze can happen. Typically, this subsides within a few days without long-term consequences.
- Absence of Major Systemic Effects: The therapy is localized, avoiding the potential systemic risks seen with certain pharmacologic agents.
In terms of results, many patients demonstrate a meaningful decrease in macular thickness and stabilization or modest improvement in visual acuity over 1–3 months. Some see a gradual enhancement in reading clarity or less distortion when looking at straight lines. Outcomes can vary widely, but repeated sessions can maintain or incrementally build on these gains. The addition of anti-VEGF injections, where appropriate, further supports better fluid control and extended periods between injections.
Understanding the Financial Landscape
The cost of micropulse laser therapy can hinge on various factors, including geographic location, clinic fees, and whether the procedure is performed as a standalone or combined treatment. In the United States, the per-session cost often falls between \$500 and \$1,500, especially if insurance partially covers it for medically necessary indications such as RVO-related macular edema. Outside the U.S., pricing depends on local healthcare systems and exchange rates. Many insurance providers do reimburse micropulse laser under certain guidelines, but coverage details can vary, making it wise for patients to verify specifics with their plan or consult with the treating center’s billing department.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding personal health concerns.
If this information has been helpful, consider sharing it on Facebook or X (formerly Twitter) to help others explore micropulse laser therapy as an option for managing retinal vein occlusion.










