Recurrent corneal erosion (RCE) is an ocular condition in which the corneal epithelium, the cornea’s outermost layer, breaks down or sloughs off repeatedly. This condition causes severe eye pain, redness, tearing, and light sensitivity, which have a significant impact on quality of life. Previous corneal trauma or underlying corneal dystrophies, such as epithelial basement membrane dystrophy, are common causes of RCE. The corneal epithelium fails to adhere properly to the underlying basement membrane, resulting in recurrent detachments.
Patients frequently experience a sudden onset of symptoms, usually upon waking, because the eyelids adhere to the corneal surface during sleep and pull away the weakly attached epithelium when opened. Visual disturbances are frequently present during the episodes, which can range from mild discomfort to severe pain. RCE can affect people of any age, but it is more common in adults who have a history of corneal injury or hereditary corneal dystrophies.
Understanding the underlying mechanisms and contributing factors to RCE is critical for developing effective management and treatment plans. Early detection and intervention can help prevent complications like persistent epithelial defects, scarring, and secondary infections, preserving vision and improving patient outcomes.
Recurrent Corneal Erosion Management
The goal of managing and treating recurrent corneal erosion is to promote epithelial healing, prevent recurrence, and alleviate symptoms. Depending on the severity and frequency of the erosions, different strategies are used, ranging from conservative to surgical interventions.
Conservative Treatments
Initial management of RCE frequently involves non-surgical approaches, particularly for patients with infrequent or mild episodes:
- Lubricating Eye Drops and Ointments: Using preservative-free artificial tears and lubricating ointments on a regular basis, particularly before bedtime, helps to maintain corneal hydration and reduce friction between the eyelids and the corneal surface. This can help prevent recurring episodes and promote healing.
- Hypertonic Saline Drops and Ointments: Hypertonic saline solutions (5% sodium chloride) drain fluid from the cornea, reducing edema and strengthening the epithelial attachment to the basement membrane. These are especially useful for nighttime use.
- Bandage Contact Lenses: Soft bandage contact lenses protect the corneal surface, relieve pain, and promote epithelial healing. They act as a mechanical barrier, preventing additional trauma to the eyelids.
- Oral Tetracyclines and Topical Steroids: Low-dose oral tetracyclines (such as doxycycline) and topical corticosteroids can reduce inflammation and regulate matrix metalloproteinases (MMPs), which degrade the basement membrane. This combination is commonly used for chronic or severe conditions.
Surgical Treatments
When conservative measures fail, or in cases of recurrent and severe episodes, surgical interventions are considered to improve epithelial adhesion and stability.
- Debridement: The mechanical removal of loose or poorly adherent epithelial cells, followed by smoothing the underlying basement membrane, promotes more stable epithelial regrowth. This procedure is frequently performed in-office using topical anesthesia.
- Anterior Stromal Puncture (ASP): ASP is the process of creating tiny punctures in the anterior stroma with a fine needle to promote stronger epithelial adhesion by facilitating fibroblast migration and basement membrane production. It is most commonly used on patients with localized erosions.
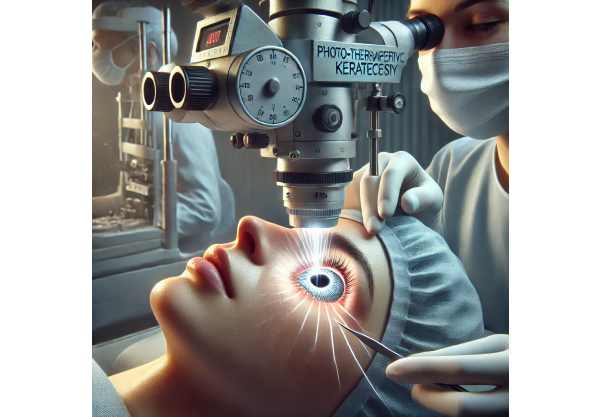
- Phototherapeutic Keratectomy (PTK): An excimer laser removes superficial corneal layers and smoothes the basement membrane, promoting uniform epithelial adhesion. This precise and controlled technique is particularly effective for patients with extensive epithelial basement membrane dystrophy or diffuse erosions.
- Amniotic Membrane Transplantation: In cases of persistent epithelial defects or recurrent erosions despite other treatments, amniotic membrane transplantation acts as a biological bandage, promoting healing and reducing inflammation. The amniotic membrane contains growth factors and anti-inflammatory properties that promote epithelialization and reduce scarring.
Post-operative Care
Postoperative care after surgical interventions is critical for ensuring optimal outcomes and preventing recurrences.
- Antibiotic and Anti-inflammatory Drops: To prevent infection and inflammation, post-surgical care usually includes the use of antibiotic and anti-inflammatory eye drops.
- Follow-up Visits: Regular follow-up visits are required to monitor healing, assess epithelial integrity, and detect any signs of recurrence early on. Additional treatments or changes in management may be required depending on the patient’s response.
Innovative Approaches to Treating Recurrent Corneal Erosion
Advances in understanding and treating recurrent corneal erosion have resulted in the development of novel therapies and techniques designed to improve patient outcomes. These cutting-edge innovations include pharmacological advances, novel surgical techniques, and regenerative medicine approaches that improve the efficacy and safety of RCE treatment.
Advanced Pharmacological Therapies
The development of targeted pharmacological therapies has transformed the treatment landscape for RCE, providing new hope for patients suffering from this difficult condition.
- Matrix Metalloproteinase Inhibitors (MMPIs): MMPs degrade the epithelial basement membrane, which contributes to recurrent erosion. Newer MMPIs, both topical and systemic, are being investigated to help stabilize the basement membrane and promote epithelial adhesion. These agents can be used as supplements to standard treatments, increasing their efficacy.
- Growth Factor Eye Drops: Topical application of growth factors like EGF and TGF-β can promote corneal epithelial healing and reduce recurrences. These drops promote cell migration, proliferation, and differentiation, resulting in rapid and stable epithelialization.
- Neurotrophic Factors: Neurotrophic keratopathy, which is defined by decreased corneal sensitivity and poor epithelial healing, can contribute to RCE. Topical neurotrophic factors, such as cenegermin (NGF, nerve growth factor), have been developed to promote corneal nerve regeneration and epithelial healing, thereby addressing the underlying neurotrophic deficiency.
Innovative Surgical Techniques
Advances in surgical techniques have increased the precision and effectiveness of RCE interventions, resulting in better outcomes with fewer complications.
- Femtosecond Laser-Assisted ASP: The femtosecond laser creates stromal punctures with unparalleled precision, increasing the efficacy and safety of ASP. This laser-assisted technique allows for uniform and controlled punctures, improving epithelial adhesion and lowering recurrence rates.
- Customized PTK Algorithms: PTK algorithms based on corneal topography and pachymetry enable personalized RCE treatment. These algorithms optimize the laser ablation pattern to account for individual variations in corneal anatomy and pathology, increasing the procedure’s efficacy and safety.
- Intraoperative OCT-Guided Procedures: Intraoperative optical coherence tomography (OCT) allows for real-time imaging of the corneal layers during surgical procedures, improving the accuracy and effectiveness of interventions such as debridement and PTK. This technology allows for precise removal of abnormal tissue while preserving healthy corneal structures.
Regenerative Medicine and Tissue Engineering
The use of regenerative medicine and tissue engineering in the treatment of RCE has the potential to promote corneal healing and prevent recurrences.
- Stem Cell Therapy: The goal of stem cell therapy is to regenerate damaged epithelial cells while restoring normal corneal architecture. Research is underway to develop stem cell-based treatments, such as limbal stem cell transplantation, to improve epithelial healing and prevent recurrences. Early results are encouraging, suggesting that stem cell therapy may become a viable option for RCE management in the future.
- Amniotic Membrane Derivatives: Amniotic membrane derivatives, including amniotic fluid extract and cryopreserved amniotic membrane, contain bioactive factors that promote epithelial healing and reduce inflammation. These derivatives can be used as eye drops or during surgery to promote epithelialization and reduce scarring.
- Engineered Corneal Scaffolds: Tissue-engineered corneal scaffolds mimic the natural extracellular matrix, creating a favorable environment for epithelial cell growth and adhesion. These scaffolds can be used as biological bandages or in surgical procedures to promote stable and long-term epithelialization.
Personalized Medical Approaches
The trend towards personalized medicine is also influencing RCE management, with therapies tailored to individual patient profiles using genetic, molecular, and clinical data.
- Genetic Profiling: Genetic profiling can help identify individuals who are at a higher risk of RCE and guide personalized treatment plans. Understanding the genetic causes of corneal dystrophies and epithelial adhesion defects can help develop targeted therapies and preventive measures.
- Biomarker Analysis: Biomarkers are quantitative indicators of disease activity and treatment efficacy. Advances in biomarker research are allowing the identification of specific molecules associated with epithelial instability and basement membrane defects, which can be used to track disease progression and guide treatment.
Future Directions
The future of RCE treatment appears bright, with ongoing research and technological advancements paving the way for even more effective and minimally invasive options. Continued research into advanced pharmacological therapies, novel surgical techniques, and regenerative medicine approaches is likely to yield new breakthroughs. As our understanding of the underlying mechanisms of RCE grows, targeted treatments that address the root causes of the condition will become more feasible, providing hope for long-term improvements in patient outcomes.






