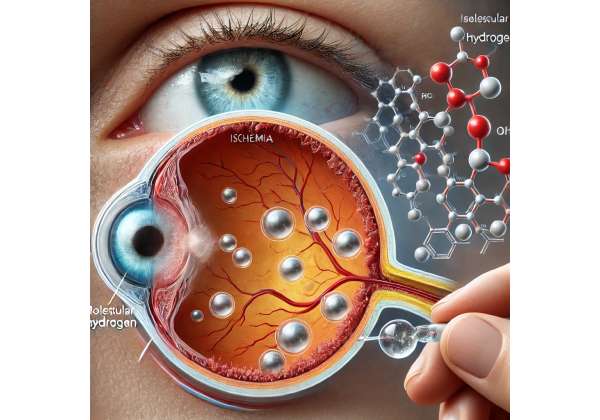
Have you ever wondered what protects our eyes from damage when blood supply is suddenly compromised? Ischemic retinopathy—a condition where the retina suffers from reduced blood flow—can be life-changing, especially if left untreated. In recent years, researchers have been paying close attention to the potential of molecular hydrogen in preventing or slowing down the vision loss associated with ischemic retinopathy. By scavenging harmful free radicals and mitigating inflammation, molecular hydrogen offers fresh hope to many patients faced with the stark reality of progressive retinal damage.
People often think about their eyes only after something goes wrong, but our retinas are at work every second we’re awake, converting light into the images we perceive. That’s exactly why it’s crucial to explore all viable protective strategies. Molecular hydrogen therapy, while still relatively new on the scene, has shown promising results in supporting overall retinal function. In the sections below, we’ll delve into the many ways this therapy may benefit those dealing with ischemic retinopathy, examining protocols, recent research, and what you need to know before considering treatment.
A Closer Look at the Power of Hydrogen in Retinal Healing
Molecular hydrogen, often described by the chemical formula H₂, might not immediately seem like a groundbreaking therapeutic agent. After all, hydrogen is the simplest element in the universe. But when administered correctly, it has demonstrated remarkable antioxidant properties that could be highly beneficial in eye conditions marked by ischemic damage. Ischemic retinopathy is one such condition—a type of retinal disease that arises from reduced blood supply to the retina. To understand how molecular hydrogen fits into the picture, it’s helpful to start with the pathophysiology of ischemic retinopathy and the role of oxidative stress.
Oxidative Stress and the Retina
Oxidative stress occurs when harmful molecules called reactive oxygen species (ROS) accumulate in the body and surpass our natural antioxidant defenses. This imbalance can cause cells to function poorly or even self-destruct. In ischemic retinopathy, the retina is already stressed due to limited blood flow. The shortage of oxygen and nutrients triggers inflammatory responses and an increase in ROS production. Over time, these free radicals cause damage to retinal cells and the delicate blood vessels that support them.
How Molecular Hydrogen Works
Molecular hydrogen’s main claim to fame is its selective antioxidant effect, meaning it can neutralize particularly harmful ROS like hydroxyl radicals without wiping out other important reactive species involved in normal cellular signaling. This selective action is crucial. In many conditions, especially ocular diseases, it’s not always beneficial to reduce every kind of radical. Certain reactive molecules help regulate physiological processes. Hydrogen therapy aims to strike a better balance—lowering destructive ROS without interfering with normal cell functions.
Interestingly, molecular hydrogen is thought to have anti-inflammatory properties as well. In the setting of ischemic retinopathy, inflammation is a central player. It contributes to retinal edema, disrupts blood vessel integrity, and can even accelerate abnormal blood vessel growth (known as neovascularization). By counteracting parts of the inflammatory cascade, molecular hydrogen may help maintain healthier conditions within the retina.
Mechanisms of Retinal Protection
When blood flow is restricted, retinal cells rapidly become starved of oxygen (hypoxia). The body responds by releasing pro-inflammatory agents and growth factors, such as vascular endothelial growth factor (VEGF), in an attempt to form new blood vessels. While VEGF can temporarily improve oxygen delivery, the newly formed vessels are often weak and prone to leakage, which further jeopardizes retinal health.
Molecular hydrogen could help in the following ways:
- Reducing Oxidative Injury: By neutralizing particularly damaging free radicals, hydrogen can help preserve the integrity of retinal cells, reducing the overall burden of oxidative stress.
- Modulating Inflammatory Responses: Hydrogen may lessen the production of pro-inflammatory cytokines, thus reducing the damage caused by local inflammation in the retina.
- Stabilizing the Blood-Retinal Barrier (BRB): The BRB acts as a gatekeeper, preventing unwanted substances from entering the retinal tissue. Excessive inflammation compromises this barrier, but hydrogen’s protective effects might help maintain barrier function, limiting further harm.
- Regulating Angiogenic Signals: Through its antioxidant and anti-inflammatory effects, hydrogen could indirectly help normalize the signals that stimulate abnormal blood vessel growth.
Why Timing Matters
Ischemic retinopathy doesn’t typically manifest overnight; it follows a pattern that depends on how quickly blood flow decreases and how the retina adapts. Catching the condition early is key, as are interventions aimed at stabilizing retinal structures. For some patients, addressing the issue right when symptoms begin—or even before they appear, in at-risk populations—could be the difference between retaining functional eyesight and facing irreversible impairment.
Complementary Nature of Hydrogen Therapy
It’s important to emphasize that molecular hydrogen isn’t a standalone cure. Traditional treatments for ischemic retinopathy can include laser therapy to obliterate abnormal blood vessels, intravitreal injections of anti-VEGF medications to curb abnormal vessel growth, and, in some cases, surgical intervention. Hydrogen therapy appears to complement these approaches by:
- Alleviating oxidative stress and inflammation, potentially making other treatments more effective.
- Offering a noninvasive adjunct that can be integrated into daily life.
- Providing a long-term supportive measure, given its relatively low toxicity and ease of application (as you’ll learn in the next section).
Thanks to these multifaceted benefits, hydrogen therapy is gaining interest from ophthalmologists and researchers looking for ways to protect delicate retinal cells without compromising safety. While more large-scale clinical trials are in progress, existing research has laid the groundwork for a plausible, biology-based rationale supporting hydrogen’s use in ischemic retinopathy.
Administering Molecular Hydrogen: Practical Guidelines for Retinal Health
The thought of using hydrogen for therapy may sound unconventional, but it’s been explored in various forms, including inhalation, oral tablets, and even saline infusions. These different delivery methods each come with their own set of considerations, from patient compliance and ease of use to how effectively the hydrogen reaches ocular tissues. Understanding these protocols is pivotal for anyone looking to explore molecular hydrogen as an adjunct in the management of ischemic retinopathy.
Inhalation of Hydrogen Gas
Inhalation remains one of the most common ways to harness hydrogen’s therapeutic effects. Specially designed machines produce hydrogen-enriched air, usually at concentrations of around 2–5%. Patients then breathe in this mixture through a nasal cannula or mask over a period that can range from 30 minutes to several hours. For retinal conditions, the goal is to ensure that enough hydrogen penetrates the bloodstream and subsequently reaches the retinal cells. Proponents of this method highlight its relatively direct route into the body. While hydrogen gas is very safe when administered at clinically recommended concentrations, proper protocols must be followed to avoid any risk of combustion with pure oxygen sources.
Hydrogen-Enriched Saline
Another avenue is intravenous or intraperitoneal delivery of hydrogen-enriched saline. This method has been studied in animal models with promising outcomes on oxidative stress markers. In a clinical setting, hydrogen-enriched saline may be administered through an IV drip, making it a more controlled option for acute care, such as immediately after a significant ischemic event. However, availability of hydrogen-enriched saline is still limited, and its use is generally confined to specialized facilities with the equipment needed to infuse hydrogen into solutions.
Oral Intake and Hydrogen Tablets
For long-term management and convenience, many individuals use oral hydrogen tablets. When dropped into water, these tablets release molecular hydrogen that can be ingested. This approach is often praised for its simplicity; patients can take hydrogen water on a schedule similar to any oral supplement, without specialized equipment. But the concentration of hydrogen in water decreases over time, so timing and proper storage are crucial. Moreover, oral tablets may provide a lower hydrogen concentration compared to inhalation, so they might serve better as a maintenance strategy rather than a frontline treatment.
Eye Drops and Topical Applications
While less common, there is ongoing research into hydrogen-infused eye drops, specifically designed to deliver antioxidant benefits straight to the ocular surface. The rationale is that direct application could bypass systemic circulation and concentrate the beneficial effects in the eye. However, the retina lies behind several protective barriers, so whether topical hydrogen solutions can penetrate deeply enough remains an open question. Preliminary studies, especially in animal models, have been somewhat promising, but more human trials are needed before these products become mainstream.
Combining Hydrogen with Other Therapies
If you’re already receiving treatment for ischemic retinopathy—be it laser therapy, anti-VEGF injections, or lifestyle interventions—introducing molecular hydrogen should ideally complement these strategies rather than replace them. For instance, patients undergoing anti-VEGF injections might also benefit from hydrogen inhalation sessions, especially if local inflammation or oxidative stress is a concern. Similarly, individuals who have been prescribed nutritional supplements (like vitamins A, C, E, and zinc) may find hydrogen water or tablets to be a straightforward addition to their daily regimen.
Patient Suitability and Customization
While molecular hydrogen is generally considered safe, it’s not necessarily ideal for everyone. Factors such as overall health status, the severity of ischemic retinopathy, and existing medical therapies can influence outcomes. For example, those with advanced diabetic retinopathy or severe vascular occlusions might require more aggressive treatment approaches, where hydrogen therapy serves as an adjunctive measure. As with any medical treatment, an individualized plan devised in collaboration with an ophthalmologist or retina specialist is the gold standard.
Scheduling and Frequency
When it comes to hydrogen therapy, consistency is key. Some treatment plans call for daily sessions of inhalation lasting 30–60 minutes, while oral tablets could be taken multiple times a day depending on dosage. Adjustments are often based on clinical improvements or changes in retinal examination findings—like a reduction in neovascularization or stabilization of visual acuity test results. Follow-up is crucial, as are routine screenings for possible complications of ischemic retinopathy, such as macular edema.
From ease of use to long-term benefits, each protocol comes with its own upsides and challenges. What’s important is finding a method that fits seamlessly into a patient’s life while effectively delivering molecular hydrogen to the retina. Ongoing research and technological advancements are steadily improving the availability and efficacy of these treatments, making it more feasible for patients to consider hydrogen as part of their comprehensive eye care plan.
Recent Breakthroughs and Eye-Opening Case Studies
Molecular hydrogen’s journey from a seemingly inert molecule to a notable antioxidant has captured the attention of ophthalmic researchers worldwide. Multiple peer-reviewed studies and clinical trials are lending credibility to the idea that hydrogen can act as a potent defense mechanism in conditions like ischemic retinopathy. By investigating both lab-based and real-world outcomes, scientists are laying the groundwork for broader acceptance and refined treatment guidelines.
Landmark Studies in Cellular Models
One of the earliest breakthroughs came from a study published in Nature Medicine (Ohsawa et al., 2007), where researchers highlighted hydrogen’s capacity to selectively scavenge hydroxyl radicals. This work wasn’t specifically on the retina, but it established a biochemical foundation for hydrogen’s protective properties. Soon, ophthalmology-focused researchers began to connect the dots, asking whether hydrogen’s selective antioxidant effect could guard sensitive retinal cells against ischemic damage.
A subsequent study in Free Radical Research (2015) used an in vitro model of retinal ischemia, showing that hydrogen supplementation significantly reduced cell death markers. By observing how retinal cells respond to oxidative stress with and without hydrogen exposure, investigators concluded that hydrogen might mitigate the inflammatory responses triggered by ischemic conditions.
Clinical Trials and Human Subjects
More recently, a pilot clinical trial reported in the Journal of Ophthalmic Inflammation and Infection (2020) explored the impact of hydrogen-rich saline infusion in patients diagnosed with diabetic retinopathy—a form of ischemic retinopathy common in long-standing diabetes. Over a span of four weeks, participants received regular hydrogen-enriched saline injections alongside standard care. Although the trial was small, patients receiving hydrogen-enriched saline showed fewer markers of inflammation in blood tests and reported subjective improvements in visual clarity. While objective measures like optical coherence tomography (OCT) scans also hinted at reduced retinal edema, researchers cautioned that larger-scale studies would be necessary to confirm these findings definitively.
Rodent and Primate Models
Animal studies offer invaluable insights into the mechanisms at play. In rodent models of retinal ischemia—often induced by raising intraocular pressure or occluding the retinal artery—molecular hydrogen delivered via inhalation was associated with:
- Lower levels of pro-inflammatory cytokines like TNF-α (tumor necrosis factor alpha).
- Better preservation of the retina’s layered structure.
- Reduced vascular leakage, indicating a healthier blood-retinal barrier.
In primate studies, hydrogen supplementation seemed to shorten recovery times after experimentally induced ischemia. According to Investigative Ophthalmology & Visual Science (2021), hydrogen-treated primates displayed a more stable retinal function over time, assessed via electroretinography, which measures the electrical responses of various cell types in the retina.
Observational Data and Case Reports
Beyond controlled experiments, individual case reports paint a personal picture of hydrogen therapy’s possible benefits. For instance, a 2022 case series in Clinical and Experimental Ophthalmology discussed two patients with ischemic central retinal vein occlusion who incorporated hydrogen inhalation sessions into their routine. Both patients also received anti-VEGF injections, but clinicians noted a more rapid decrease in retinal swelling compared to what might be expected from anti-VEGF therapy alone. Though anecdotal, these case reports underscore the potential synergy between molecular hydrogen and established treatments.
Emerging Topics of Interest
Researchers are now branching out to explore how hydrogen therapy might enhance other interventions for ischemic retinopathy. A group in Japan is examining whether combining hydrogen inhalation with hyperbaric oxygen therapy could offer dual benefits—supplying extra oxygen while counteracting oxidative stress. Another area of focus involves protective strategies for post-surgical recovery; for instance, patients recovering from vitrectomy for retinal detachment could benefit from hydrogen therapy to reduce inflammation and expedite tissue healing.
Challenges in Research
Despite the growing body of evidence, certain obstacles must be addressed before hydrogen therapy becomes a widely endorsed option. For one, standardized dosing protocols are not yet firmly established. Different studies employ varying concentrations of hydrogen in either gas or liquid form, making direct comparisons across trials tricky. Also, the long-term safety profile, while appearing promising in short-term studies, needs further validation through extended clinical trials. Finally, placebo-controlled studies are essential to rule out any confounding factors and accurately gauge the magnitude of hydrogen’s benefits in ischemic retinopathy.
Overall, these converging lines of evidence—from lab-based cellular research to observational patient reports—indicate that molecular hydrogen has the potential to be a significant player in ischemic retinopathy treatment. While the field is still evolving, each new study helps refine our understanding of how hydrogen works at the molecular level and how best to deploy it in clinical settings.
Weighing Efficacy and Safety: Points to Keep in Mind
Molecular hydrogen, by most accounts, presents an intriguing blend of effectiveness and safety. Its selective antioxidant function sets it apart from broad-spectrum antioxidants that might interfere with normal cellular processes. Moreover, hydrogen’s small molecular size allows for quick absorption and wide tissue distribution—a key asset in retinal protection.
Because hydrogen primarily targets the most damaging free radicals, it is less likely to cause unwanted side effects like immunosuppression. Additionally, hydrogen is a naturally occurring gas in the body (albeit in small amounts), suggesting that moderate supplementation doesn’t drastically disrupt biological systems. Nevertheless, anyone with underlying eye conditions or systemic illnesses should consult a qualified ophthalmologist or other medical professionals before introducing hydrogen therapy into their regimen. The potential for interactions, while low, cannot be entirely dismissed without proper medical guidance.
When used alongside standard treatments for ischemic retinopathy—like anti-VEGF injections, laser therapy, or surgical interventions—hydrogen therapy often appears to heighten the overall protective effects. Many practitioners consider it a gentle but impactful addition rather than a frontline monotherapy. Ultimately, the key lies in personalized care, where an ophthalmic specialist can determine the best approach to incorporate molecular hydrogen based on each patient’s unique clinical status and treatment history.
Your Investment in Vision: A Brief Guide to Pricing
Pricing for molecular hydrogen therapy can vary widely depending on the delivery method. Inhalation devices for home use can range from a few hundred dollars to well above a thousand. Hydrogen tablets, often sold as dietary supplements, offer a more budget-friendly initial cost but require ongoing purchases for long-term use. Clinical administration of hydrogen-enriched saline may fall under specialized procedures, with expenses fluctuating based on facility fees and regional healthcare systems. It’s advisable to request a full cost breakdown from any healthcare provider or product manufacturer so you can make an informed decision.
Disclaimer: This article is intended for informational purposes only and does not replace personalized medical advice. Always consult a qualified ophthalmologist or healthcare provider regarding any questions or concerns you may have about ischemic retinopathy or the use of molecular hydrogen therapy.
If you found this exploration of molecular hydrogen’s role in ischemic retinopathy helpful, consider sharing it on your social media platforms—Facebook, X (formerly Twitter), or anywhere else you engage with friends and family who might benefit from this information.