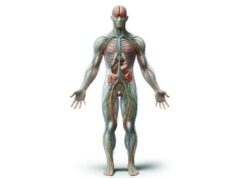
Peripheral nerves serve as vital communication highways between the central nervous system and the rest of the body. They are responsible for transmitting sensory information, initiating motor responses, and regulating involuntary functions essential for survival. In this guide, we explore every facet of peripheral nerves—from their intricate anatomical structures and essential roles in physiology to the various conditions that affect them and the cutting‐edge treatments available. Whether you’re a healthcare professional or a curious reader, this comprehensive resource offers expert insights, practical advice, and evidence-based recommendations to help you understand and maintain optimal nerve health.
Table of Contents
- Structural Overview and Anatomy
- Functional Physiology and Role
- Peripheral Nerve Disorders
- Diagnostic Approaches
- Management and Therapeutic Options
- Nutritional and Supplement Support
- Lifestyle Strategies for Wellness
- Reliable References and Resources
- Frequently Asked Questions
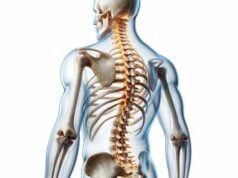
Structural Overview and Anatomy of Peripheral Nerves
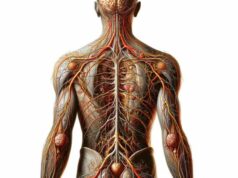
Peripheral nerves are marvels of biological engineering, designed to efficiently relay electrical impulses over long distances. At the core of these nerves lie bundles of axons—long, slender extensions of neurons—that serve as conduits for transmitting information. These axons are organized into groups known as fascicles, which are then enveloped by multiple protective layers of connective tissue.
The outermost layer, known as the epineurium, is a dense sheath that provides robust structural support and shields the nerve from mechanical stresses. Beneath the epineurium lies the perineurium, a delicate barrier that encases each fascicle, preserving the internal environment and protecting nerve fibers from external contaminants. Inside each fascicle, the endoneurium ensconces individual axons, offering both insulation and nutritional support. This multilayered organization not only ensures structural integrity but also allows for the compartmentalization of nerve fibers, which can be classified as sensory, motor, or autonomic based on their function.
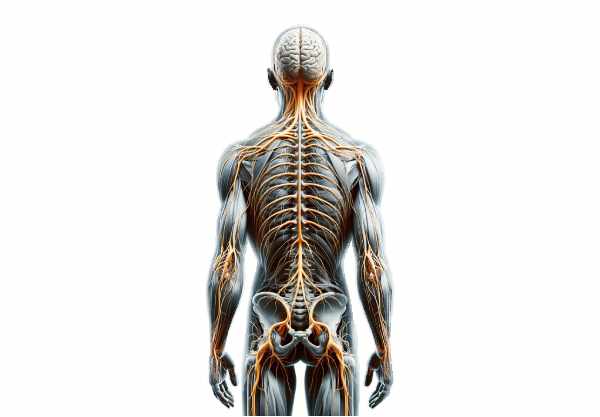
The nerve fibers themselves vary in size and myelination. Myelin, produced by Schwann cells in the peripheral nervous system, acts as an insulator that dramatically increases the speed of electrical impulse transmission. Based on their diameter and the extent of myelination, nerve fibers are categorized into three primary types:
- A fibers: Large, heavily myelinated fibers responsible for rapid signal conduction, including those that control proprioception and fine motor functions.
- B fibers: Medium-sized myelinated fibers that primarily facilitate autonomic functions.
- C fibers: Small, unmyelinated fibers that conduct impulses slowly, yet play a crucial role in transmitting pain and temperature sensations.
The blood supply to peripheral nerves is provided by a network of tiny blood vessels known as the vasa nervorum. These vessels, which branch off from larger arteries, infiltrate the nerve through the epineurium and perineurium, delivering vital oxygen and nutrients. This vascular network is essential, as nerve tissue has a high metabolic demand; glucose, transported into the cells via specific carriers, is metabolized to generate adenosine triphosphate (ATP), which fuels nerve impulse propagation.
When peripheral nerves suffer injury, their capacity for regeneration sets them apart from many other tissues in the body. Nerve injuries are generally classified into three categories:
- Neurapraxia: A transient block of nerve conduction without structural damage, typically resolving within days to weeks.
- Axonotmesis: Characterized by damage to the axons while the surrounding connective tissue remains intact; here, regeneration is possible along existing pathways.
- Neurotmesis: The most severe form, where both axons and their supporting structures are disrupted, often requiring surgical intervention for any potential recovery.
Following injury, Schwann cells play an indispensable role by proliferating and secreting growth factors that guide regenerating axons. Although the regenerative process can be impressive, the extent of recovery depends on factors such as the severity of the injury, the distance the regenerating axons must travel, and the presence of scar tissue that may impede re-growth. Understanding the detailed anatomy of peripheral nerves provides a foundation for appreciating their remarkable functions and the complex challenges associated with nerve injury and repair.
Beyond their structural components, the spatial arrangement of nerve fibers also contributes to the selective routing of signals. Sensory fibers are often arranged peripherally within a nerve bundle, while motor fibers tend to be more centrally located. This organizational principle not only facilitates efficient signal transmission but also plays a significant role in how nerves respond to injury, with some fibers being more vulnerable to damage than others. Advances in imaging technologies, such as magnetic resonance neurography, now allow clinicians to visualize these intricate structures in vivo, enhancing our ability to diagnose and treat nerve disorders.
The interplay between the structural organization and the physiological demands of peripheral nerves highlights the evolutionary sophistication of these systems. Their complex architecture supports a diverse range of functions, from rapid reflexes to the modulation of autonomic processes, underscoring the essential role they play in maintaining homeostasis and enabling interaction with the environment.
Furthermore, recent research into the molecular composition of the various connective tissue layers has revealed potential targets for therapeutic intervention. By understanding how proteins within the epineurium, perineurium, and endoneurium interact with each other and with surrounding cells, scientists are developing innovative approaches to enhance nerve regeneration and reduce scarring following injury. This integration of structural biology with clinical practice holds promise for significantly improving outcomes in patients with peripheral nerve injuries.
In summary, the anatomical configuration of peripheral nerves—with its multiple protective layers, diverse fiber types, and rich vascular supply—creates an optimal environment for rapid and reliable signal transmission. This sophisticated structure not only facilitates complex sensory, motor, and autonomic functions but also provides a blueprint for the nerve’s impressive capacity to repair itself after injury. The detailed understanding of peripheral nerve anatomy is thus integral to both basic neuroscience and the development of advanced therapeutic strategies.
Functional Physiology and Role of Peripheral Nerves
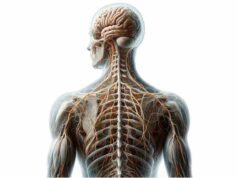
Peripheral nerves are central to nearly every aspect of bodily function, acting as the communication bridges between the brain, spinal cord, and the myriad tissues and organs that compose our body. Their role extends far beyond mere signal transmission—they are fundamental to sensation, movement, and the regulation of involuntary processes.
Sensory Transmission
Sensory nerves are tasked with collecting data from specialized receptors located in the skin, muscles, and internal organs. These receptors, which include mechanoreceptors, thermoreceptors, nociceptors, and proprioceptors, detect a wide range of stimuli such as pressure, temperature, pain, and body position. Once stimulated, these receptors convert physical energy into electrical signals, which travel along afferent nerve fibers to the central nervous system. The brain then processes these signals, enabling us to perceive and react to our environment. This sophisticated sensory network is essential for everyday activities, from recognizing harmful stimuli to appreciating subtle textures and temperatures.
Motor Command and Coordination
Motor nerves are responsible for converting neural signals into action. They transmit instructions from the central nervous system to skeletal muscles, triggering voluntary movements such as walking, writing, or even smiling. These somatic motor nerves are crucial for fine motor control and complex coordinated activities. Moreover, motor nerves extend their influence to the autonomic system, innervating smooth muscles and glands to control involuntary processes like digestion, respiratory rate, and heart function. The neuromuscular junction—a specialized synapse between a nerve terminal and a muscle fiber—ensures that signals are efficiently translated into mechanical action.
Autonomic Regulation
The autonomic nervous system, divided into sympathetic and parasympathetic branches, maintains internal balance and regulates vital functions without conscious effort. The sympathetic division mobilizes the body in response to stress or danger, increasing heart rate, dilating the airways, and redirecting blood flow to essential muscles. Conversely, the parasympathetic division promotes restorative activities, such as reducing heart rate and stimulating digestion. These opposing yet complementary systems ensure that the body can adapt rapidly to changing circumstances while conserving energy during periods of rest.
Reflex Arcs and Rapid Response
Reflex arcs exemplify the efficiency of peripheral nerves by enabling rapid, involuntary responses to external stimuli. In a typical reflex arc, sensory receptors detect a stimulus and send a signal to the spinal cord. Here, interneurons process the information and immediately relay a command to motor neurons, which in turn activate the appropriate muscle groups. This streamlined circuit bypasses the brain, ensuring that responses such as the knee-jerk reaction occur almost instantaneously—a critical mechanism for protecting the body from injury.
Neurotransmission Mechanisms
At the core of nerve function is the process of neurotransmission. When an action potential (an electrical impulse) reaches the nerve terminal, it triggers the release of neurotransmitters into the synaptic cleft. These chemical messengers, such as acetylcholine, norepinephrine, glutamate, and gamma-aminobutyric acid (GABA), bind to receptors on adjacent neurons or muscle cells, thereby propagating the signal. After transmission, the neurotransmitters are either reabsorbed, enzymatically degraded, or diffuse away, ensuring that signals are both precise and transient.
Modulation of Pain and Sensation
Pain perception, a critical survival mechanism, is mediated by specialized nerve fibers that detect noxious stimuli. Aδ fibers quickly transmit sharp, localized pain, alerting the body to immediate harm, whereas C fibers convey slower, more diffuse pain signals that help monitor ongoing tissue damage. This dual system of pain transmission allows for both rapid response and sustained awareness of potentially harmful conditions, prompting timely protective actions.
Integration and Coordination
The interplay of these various functions demonstrates the intricate coordination required for proper nerve function. Sensory inputs, motor outputs, and autonomic controls must all work in harmony to maintain balance and ensure appropriate reactions to internal and external changes. Disruptions in any part of this network can lead to significant functional deficits, emphasizing the importance of each component of peripheral nerve physiology.
Emerging research is uncovering even more nuanced roles for peripheral nerves, including their involvement in immune responses and tissue repair. Studies suggest that nerves can modulate inflammation and even influence local healing processes by releasing specific signaling molecules. This growing body of evidence not only enhances our understanding of nerve physiology but also opens new avenues for therapeutic interventions aimed at harnessing the regenerative potential of the nervous system.
In essence, peripheral nerves are the operational backbone of the human body. Their ability to rapidly transmit complex signals underlies our capacity to sense, move, and respond to the world around us. By delving into the mechanisms of sensory detection, motor coordination, and autonomic regulation, we gain a comprehensive understanding of how these neural pathways contribute to overall health and function.
Peripheral Nerve Disorders: Common Conditions
Despite their robust design, peripheral nerves are susceptible to a range of disorders that can impair their function and diminish quality of life. These conditions vary widely in cause, severity, and treatment, but they all share the common feature of disrupting the normal transmission of nerve signals.
Diabetic Neuropathy
One of the most prevalent forms of peripheral nerve damage is diabetic neuropathy. Chronic high blood sugar levels in individuals with diabetes can lead to nerve damage, particularly in the extremities such as the feet and legs. Patients may experience burning sensations, numbness, and tingling, along with muscle weakness. Effective management hinges on tight glycemic control, pain management strategies, and lifestyle modifications that include regular exercise and a nutrient-rich diet.
Carpal Tunnel Syndrome
Carpal tunnel syndrome arises when the median nerve is compressed as it traverses the narrow carpal tunnel in the wrist. This condition is common among individuals who perform repetitive hand movements, such as typists or assembly line workers. The symptoms typically include numbness, tingling in the thumb and first three fingers, and sometimes pain that radiates up the arm. Treatment ranges from conservative approaches, like splinting and anti-inflammatory medications, to surgical decompression for more severe cases.
Guillain-Barré Syndrome
Guillain-Barré syndrome is an autoimmune condition in which the body’s immune system mistakenly attacks peripheral nerves, often following an infection. This disorder can progress rapidly, leading to weakness, tingling sensations, and even paralysis. The severity of Guillain-Barré syndrome can vary, and in some instances, patients may require respiratory support due to impaired nerve function in the muscles controlling breathing. Immunotherapies, such as intravenous immunoglobulin (IVIG) and plasmapheresis, are commonly used to mitigate the autoimmune response.
General Peripheral Neuropathy
Peripheral neuropathy is a broad term encompassing various conditions that affect the nerves. Causes can range from physical trauma and infections to autoimmune disorders and exposure to toxins. Nutritional deficiencies, especially of B vitamins, are also common contributors. Patients typically report pain, numbness, and weakness, which may progress over time. Treatment is generally aimed at addressing the underlying cause, alleviating symptoms, and preventing further nerve damage.
Hereditary Neuropathies
Inherited conditions such as Charcot-Marie-Tooth disease (CMT) affect the peripheral nerves by progressively weakening them over time. Individuals with CMT experience muscle atrophy, foot deformities, and difficulties with balance and coordination. Although there is no cure, various interventions—including physical therapy, orthotic devices, and sometimes surgical procedures—can help manage symptoms and improve mobility.
Amyotrophic Lateral Sclerosis (ALS)
ALS, or Lou Gehrig’s disease, is a devastating neurodegenerative condition that affects both upper and lower motor neurons. The progressive degeneration of these neurons leads to severe muscle weakness, difficulties in speaking and swallowing, and respiratory failure. While the exact cause of ALS remains unclear, treatment typically focuses on symptom management, supportive care, and the use of disease-modifying therapies to slow progression.
Other Neuropathies
In addition to the conditions described above, peripheral nerves can be compromised by factors such as physical injury, exposure to toxins (including heavy metals and certain drugs), and infections like Lyme disease or shingles. Autoimmune conditions such as lupus and rheumatoid arthritis can also lead to neuropathic symptoms, underscoring the diverse origins of nerve disorders. Early diagnosis and targeted treatment are crucial for mitigating symptoms and preserving nerve function.
The diverse manifestations of peripheral nerve disorders underscore the complexity of these conditions. Treatment strategies must be tailored to the individual, addressing not only the symptoms but also the underlying cause. This approach is critical for improving long-term outcomes and maintaining a good quality of life for those affected.
Diagnostic Approaches for Peripheral Nerve Issues
Accurate diagnosis of peripheral nerve disorders is paramount in crafting effective treatment plans. A comprehensive diagnostic evaluation typically involves a combination of clinical assessments, electrophysiological testing, imaging studies, laboratory analyses, and sometimes even invasive procedures.
Clinical Assessment
The diagnostic process generally begins with a thorough clinical evaluation. This includes obtaining a detailed medical history, which provides insight into the onset, duration, and progression of symptoms, as well as any potential risk factors like diabetes, recent infections, or exposure to toxins. During the physical examination, healthcare providers assess muscle strength, reflexes, coordination, and sensory perception. Special tests—such as Tinel’s sign or Phalen’s maneuver—are often employed to pinpoint the location and severity of nerve compression, particularly in conditions like carpal tunnel syndrome.
Electrophysiological Studies
Electrophysiological tests are instrumental in evaluating the functional integrity of peripheral nerves.
- Nerve Conduction Studies (NCS): In these tests, electrodes are placed along the skin over specific nerves, and small electrical impulses are delivered. The speed and amplitude of the responses are measured, helping to identify abnormalities in nerve conduction that may indicate demyelination or axonal loss.
- Electromyography (EMG): This technique involves inserting a fine needle electrode into muscles to record electrical activity both at rest and during contraction. EMG helps distinguish between nerve and muscle disorders, providing essential information about the severity and distribution of nerve damage.
Imaging Techniques
Modern imaging modalities have revolutionized the diagnosis of peripheral nerve conditions.
- Magnetic Resonance Imaging (MRI): MRI, including specialized techniques such as magnetic resonance neurography (MRN), offers high-resolution images of nerve structures. It is particularly valuable in detecting nerve compression, inflammation, and tumors.
- Ultrasound: A non-invasive and real-time imaging tool, ultrasound allows clinicians to visualize the nerve’s size, structure, and any entrapments or cystic formations that may be present.
Laboratory Analyses
Blood tests and other laboratory studies can reveal metabolic or systemic conditions that contribute to neuropathy. For instance, tests for blood sugar levels, vitamin deficiencies, autoimmune markers, and infections provide critical clues that help tailor treatment strategies. In cases where autoimmune neuropathies are suspected, specific antibody tests can confirm the diagnosis.
Invasive Diagnostic Procedures
When non-invasive tests are inconclusive, more direct methods may be required.
- Nerve Biopsy: In complex or atypical cases, a small sample of nerve tissue may be surgically extracted for microscopic analysis. This can reveal structural abnormalities, inflammatory infiltrates, or degenerative changes that might not be evident through other tests.
- Skin Biopsy: Particularly useful for diagnosing small fiber neuropathies, a skin biopsy assesses the density and morphology of nerve fibers in the skin, offering insights into conditions that might be missed by nerve conduction studies.
Specialized Functional Testing
Other diagnostic tools include quantitative sensory testing (QST), which measures responses to controlled stimuli such as temperature and vibration, and autonomic testing, which assesses heart rate variability and sweat production to evaluate the function of the autonomic nerves. Together, these tests provide a comprehensive picture of nerve health, enabling clinicians to design personalized treatment plans.
The integration of these diagnostic modalities not only aids in pinpointing the exact nature of a nerve disorder but also informs the prognosis and treatment approach. As diagnostic technologies continue to evolve, our ability to detect subtle nerve impairments at an earlier stage will undoubtedly improve, paving the way for more effective interventions.
Management and Therapeutic Options for Nerve Disorders
Treating peripheral nerve disorders requires a multidisciplinary approach that is as diverse as the conditions themselves. The overarching goal is to alleviate symptoms, preserve or restore nerve function, and address the underlying cause of the damage. Treatment modalities range from pharmacological management to physical rehabilitation and advanced surgical procedures.
Pharmacological Interventions
Medications play a central role in managing neuropathic pain and other symptoms.
- Pain Management: Drugs such as anticonvulsants (gabapentin, pregabalin) and antidepressants (amitriptyline, duloxetine) are commonly prescribed to stabilize nerve activity and reduce pain. Topical agents like capsaicin cream and lidocaine patches offer localized relief, while opioids are generally reserved for severe cases due to their potential for dependency.
- Immunomodulatory Therapies: In autoimmune neuropathies, treatments such as intravenous immunoglobulin (IVIG) and plasmapheresis are utilized to curb the immune system’s attack on nerve tissues. Corticosteroids and other immunosuppressants can also reduce inflammation and slow disease progression.
Physical and Occupational Rehabilitation
Rehabilitation is a cornerstone of therapy, particularly for patients recovering from nerve injury or managing chronic neuropathic conditions.
- Physical Therapy: Tailored exercise programs focus on restoring muscle strength, improving balance, and enhancing coordination. Stretching and range-of-motion exercises help reduce muscle stiffness, while assistive devices like braces or orthotics can provide additional support.
- Occupational Therapy: This discipline helps patients adapt to functional limitations in daily activities. Occupational therapists introduce adaptive techniques and recommend assistive technologies that facilitate independence in routine tasks such as dressing, eating, and writing.
Surgical Solutions
When conservative measures fail to alleviate symptoms, surgical intervention may be necessary.
- Decompression Surgeries: Procedures such as carpal tunnel release aim to alleviate nerve compression by cutting ligaments that constrict the nerve.
- Nerve Repair and Grafting: In cases of traumatic injury, microsurgical techniques can reconnect severed nerve fibers or graft new nerve tissue to restore function. Although these procedures are complex, advancements in surgical techniques and postoperative care have significantly improved outcomes.
- Innovative Procedures: Emerging techniques, such as targeted nerve stimulation, are being developed to modulate nerve activity and offer relief for chronic neuropathic pain.
Emerging and Regenerative Therapies
Recent scientific advances have introduced novel therapies that target nerve regeneration and repair at a cellular level.
- Stem Cell Therapy: Research is underway to harness the regenerative potential of stem cells for repairing damaged nerves, with early studies showing promising results in restoring function.
- Growth Factor Administration: Delivering nerve growth factors directly to the injury site has been shown to stimulate axonal regeneration and enhance the healing process.
- Neuromodulation Techniques: Non-invasive approaches such as transcutaneous electrical nerve stimulation (TENS) and more invasive spinal cord stimulation (SCS) provide alternatives for managing chronic pain by altering nerve signaling patterns.
- Gene Therapy: Experimental gene therapies aim to correct genetic mutations responsible for inherited neuropathies, offering hope for conditions like Charcot-Marie-Tooth disease.
Overall, the management of peripheral nerve disorders is highly individualized, requiring a careful balance of therapies tailored to the patient’s specific condition, severity, and overall health status. Continuous research and technological innovation continue to refine these treatment strategies, offering new avenues for recovery and improved quality of life.
Nutritional and Supplement Support for Nerve Health
Optimal nerve function is not solely dependent on advanced medical treatments; nutrition and targeted supplementation also play a significant role in supporting nerve health. A diet rich in essential vitamins, minerals, and antioxidants can promote nerve repair, reduce inflammation, and enhance overall neurological function.
Vital Vitamins and Minerals
B Vitamins are particularly crucial for nerve maintenance.
- Vitamin B1 (Thiamine): Enhances nerve conduction and helps prevent neuropathy, especially in individuals with diabetes.
- Vitamin B6 (Pyridoxine): Plays an important role in the synthesis of neurotransmitters, though excessive doses may lead to nerve toxicity.
- Vitamin B12 (Cobalamin): Essential for maintaining the myelin sheath—a protective covering around nerve fibers—ensuring efficient signal transmission.
Magnesium is another key mineral that supports nerve function. It is involved in nerve signal transmission and can help alleviate neuropathic pain, while also contributing to muscle relaxation and overall neuromuscular health.
Antioxidants and Neuroprotective Agents
Oxidative stress is a major contributor to nerve damage, and antioxidants can counteract this process.
- Alpha Lipoic Acid: A potent antioxidant that helps reduce oxidative damage and improve nerve conduction, particularly beneficial in diabetic neuropathy.
- Coenzyme Q10: Supports mitochondrial function and energy production in nerve cells, reducing the impact of oxidative stress on nerve tissue.
Essential Fatty Acids and Herbal Supplements
Omega-3 Fatty Acids, found in fish oil, have anti-inflammatory properties that support nerve repair and regeneration. They help maintain cell membrane integrity, ensuring that nerve signals are transmitted efficiently.
Herbal supplements such as St. John’s Wort and Ginkgo Biloba have been shown to exert neuroprotective effects. St. John’s Wort may help alleviate mild neuropathic pain, while Ginkgo Biloba improves blood flow to nerves and provides antioxidant protection.
Integrating Nutritional Strategies
In addition to specific supplements, a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is essential. Such a diet provides a broad spectrum of micronutrients that support nerve function and overall health. Combining dietary strategies with targeted supplementation can enhance nerve repair, reduce inflammation, and improve the overall quality of life for those experiencing nerve-related issues.
Lifestyle Strategies for Optimal Nerve Wellness
Maintaining robust nerve health requires more than just medical interventions; everyday lifestyle choices significantly impact the integrity and function of peripheral nerves. Adopting healthy habits can prevent nerve damage and support recovery from existing conditions.
Balanced Diet and Regular Exercise
A nutrient-dense diet combined with regular physical activity is the cornerstone of nerve wellness. Monitoring blood sugar levels, especially for individuals with diabetes, helps prevent neuropathic complications. Regular exercise improves blood circulation, promotes muscle strength, and supports nerve repair. Whether through aerobic activities, strength training, or flexibility exercises, physical activity not only enhances overall health but also reduces the risk of developing nerve-related issues.
Avoiding Toxins and Harmful Habits
Exposure to environmental toxins, heavy metals, and certain medications can negatively impact nerve function. Limiting exposure to these substances is crucial. Additionally, smoking and excessive alcohol consumption have been shown to impair blood flow and contribute to nutritional deficiencies, both of which can exacerbate nerve damage.
Injury Prevention and Ergonomic Practices
Taking proactive steps to protect nerves is essential. Adopting ergonomic practices—such as using supportive seating, taking regular breaks during repetitive tasks, and employing proper lifting techniques—can help prevent nerve injuries. For individuals at risk, assistive devices like braces or ergonomic keyboards can make a significant difference in reducing strain on peripheral nerves.
Routine Health Monitoring
Regular medical check-ups are vital for early detection and intervention of nerve disorders. By staying vigilant and seeking prompt medical advice when symptoms arise, patients can avoid complications and ensure that any nerve damage is addressed swiftly. Preventative strategies, including regular screenings and lifestyle modifications, are key to long-term nerve health.
Stress Management and Mental Well-Being
Chronic stress can adversely affect the autonomic nervous system and contribute to nerve dysfunction. Techniques such as meditation, deep breathing exercises, and mindfulness practices can help reduce stress levels, indirectly supporting nerve health. By managing both physical and emotional stressors, individuals can create a holistic approach to maintaining optimal nerve function.
Incorporating these lifestyle strategies into daily routines not only protects peripheral nerves but also enhances overall well-being. The synergy between a healthy diet, regular exercise, avoidance of toxins, and proactive health management creates a strong foundation for long-lasting nerve vitality.
Reliable References and Further Resources
For those interested in further exploring the complexities of peripheral nerves, numerous authoritative resources are available. These resources span books, academic journals, and digital tools that provide in-depth information, research updates, and practical management tips.
Recommended Books
- “Peripheral Neuropathy: What It Is and What You Can Do to Feel Better” by Norman Latov
This comprehensive guide offers practical advice on managing neuropathy, with insights into both traditional and emerging treatment options. - “The Diabetic Neuropathy Handbook” by Michael T. Sheehan
Focusing specifically on nerve damage associated with diabetes, this handbook provides strategies for prevention and management, including dietary and lifestyle modifications. - “Numb Toes and Aching Soles: Coping with Peripheral Neuropathy” by John A. Senneff
An accessible resource for patients, this book discusses the challenges of living with neuropathy and offers advice on coping with the daily impacts of nerve damage.
Scholarly Journals
- Journal of Peripheral Nervous System (JPNS):
A respected source for the latest research, reviews, and clinical studies on peripheral nerve structure, function, and pathology. - Muscle & Nerve:
This journal provides a blend of basic science and clinical research, offering insights into neuromuscular diseases, including those affecting peripheral nerves.
Mobile Applications
- MyPainDiary:
A user-friendly app that helps individuals track pain levels, identify triggers, and monitor treatment responses, facilitating better management of chronic neuropathic pain. - MediSafe:
An effective medication management tool that ensures adherence to complex treatment regimens and reminds patients to take their supplements and medications on time. - PhysiApp:
Provides guided physical therapy exercises, tailored to improve muscle strength and coordination, especially for those recovering from nerve injuries or managing chronic conditions.
These trusted resources are invaluable for both patients and healthcare professionals seeking to deepen their understanding of peripheral nerve disorders and their management. Staying informed through these channels can empower individuals to make proactive decisions regarding their nerve health.
Frequently Asked Questions on Peripheral Nerves
What are peripheral nerves and why are they important?
Peripheral nerves connect the central nervous system to the rest of the body. They are essential for transmitting sensory information, controlling muscle movements, and regulating involuntary functions. Their health is critical for overall well-being and effective bodily responses.
How does nerve damage occur?
Nerve damage can occur due to various causes, including diabetes, physical trauma, infections, autoimmune reactions, and exposure to toxins. Chronic conditions and nutritional deficiencies can also lead to nerve degeneration and impaired signal transmission.
What are the common symptoms of peripheral neuropathy?
Common symptoms include numbness, tingling, burning sensations, muscle weakness, and balance problems. These symptoms typically begin in the extremities, such as the hands and feet, and may progress over time if the underlying cause is not addressed.
Can peripheral nerves regenerate after injury?
Peripheral nerves have a notable capacity for regeneration. The extent of recovery depends on the type and severity of the injury, with milder forms often recovering fully, while more severe injuries may require surgical intervention and have a more unpredictable outcome.
What lifestyle changes can support nerve health?
Maintaining a balanced diet, exercising regularly, avoiding toxins, managing chronic conditions, and reducing stress can support nerve health. Regular medical check-ups and adopting ergonomic practices also play a significant role in preventing further nerve damage.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for concerns regarding nerve health or any medical condition.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about peripheral nerve health and the latest treatment strategies.