Post-LASIK ectasia is a challenging complication, yet innovative therapies are reshaping how ophthalmologists preserve vision and restore corneal integrity. Among these, corneal collagen cross-linking (CXL) stands out as a breakthrough treatment that not only stabilizes the ectatic cornea but also prevents progressive vision loss. By strengthening the corneal stroma through a controlled photochemical reaction, CXL reinforces the weakened corneal architecture, offering patients renewed hope for long-term visual stability. This article explores the transformative potential of CXL in managing post-LASIK ectasia, detailing its mechanism of action, precise treatment protocols, the latest clinical research supporting its use, outcomes regarding efficacy and safety, and an overview of current pricing considerations.
Understanding Post-LASIK Ectasia and the Role of Corneal Collagen Cross-Linking
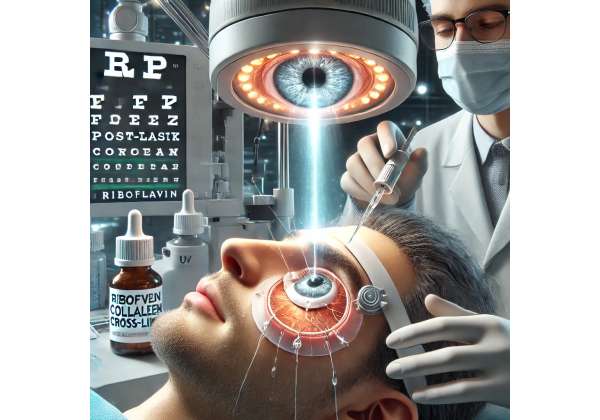
Corneal collagen cross-linking is a minimally invasive procedure that has revolutionized the management of post-LASIK ectasia. The underlying principle of CXL involves the photochemical strengthening of corneal collagen fibers through the application of riboflavin (vitamin B2) and ultraviolet-A (UV-A) light. This process induces the formation of new chemical bonds (cross-links) between collagen molecules, effectively increasing the biomechanical rigidity of the cornea.
In patients who have undergone LASIK, the integrity of the cornea may be compromised due to the removal of corneal tissue, predisposing them to ectasia—a progressive thinning and bulging of the cornea. The resultant irregular corneal shape can lead to significant visual distortion, decreased visual acuity, and increased higher-order aberrations. CXL offers a direct therapeutic intervention by halting the progression of ectasia, thereby preventing further deterioration of vision.
The mechanism of action of CXL is both elegant and robust. After the application of riboflavin, which acts as a photosensitizer, the cornea is exposed to controlled UV-A light. The interaction between the riboflavin and UV-A leads to the generation of reactive oxygen species, which in turn facilitate the formation of covalent bonds between collagen fibrils. This molecular reinforcement enhances the structural stability of the corneal stroma and reduces the likelihood of further deformation.
One of the major advantages of CXL is its ability to target the underlying biomechanical weakness without the need for invasive surgical reconstruction. Unlike other interventions that may require donor tissue or implants, CXL utilizes the patient’s own corneal tissue, thereby reducing the risk of rejection and other immune-related complications. Additionally, the procedure has a relatively short recovery time and can be performed on an outpatient basis, making it an attractive option for both patients and clinicians.
The evolution of CXL techniques has been marked by continual refinements in both methodology and technology. Innovations such as accelerated cross-linking protocols have significantly reduced treatment time while maintaining efficacy. Furthermore, modifications in riboflavin formulations and UV-A irradiation parameters have improved safety profiles, particularly for patients with thinner corneas or other complicating factors. These advancements ensure that CXL can be tailored to the individual needs of patients, optimizing outcomes while minimizing risks.
Clinical studies and real-world experiences have provided robust evidence supporting the efficacy of CXL in stabilizing post-LASIK ectasia. For example, research published in the Journal of Cataract & Refractive Surgery (2018) demonstrated significant improvements in corneal topography and visual acuity in patients treated with CXL, with many showing stabilization of ectatic progression over a two-year follow-up period. Similarly, a study in Ophthalmology (2019) reported that patients experienced marked reductions in corneal steepening and improvements in biomechanical properties following the procedure. These findings underscore the dual benefits of CXL in both halting disease progression and enhancing visual function.
The success of corneal collagen cross-linking in post-LASIK ectasia management also lies in its versatility. It can be employed as a stand-alone treatment or as an adjunct to other procedures, such as customized corneal surface ablation, to further improve visual outcomes. Surgeons now routinely consider CXL in treatment algorithms for patients with early signs of ectasia, offering a proactive approach that addresses the condition before significant visual deterioration occurs.
By strengthening the corneal framework, CXL not only preserves existing vision but also provides a stable foundation for potential future interventions, such as intracorneal ring segment implantation. This integrated approach to ectasia management highlights the broader impact of CXL as a cornerstone therapy that can be adapted to various clinical scenarios. As the field continues to evolve, ongoing research and technological improvements promise to further refine the procedure, expanding its indications and enhancing its efficacy.
Overall, corneal collagen cross-linking represents a transformative innovation in the management of post-LASIK ectasia. Its ability to reinforce the natural corneal structure while preventing progressive visual loss has made it an indispensable tool in modern refractive surgery and ocular therapeutics.
Step-by-Step Corneal Collagen Cross-Linking: Techniques and Treatment Protocols
The successful implementation of corneal collagen cross-linking (CXL) for post-LASIK ectasia requires a meticulous, step-by-step approach to ensure optimal outcomes while preserving corneal health. Treatment protocols are designed to maximize the biomechanical strengthening effect of the procedure while minimizing potential risks.
Preoperative Evaluation and Patient Selection
The process begins with a thorough preoperative assessment. Patients undergo comprehensive eye examinations, including corneal topography, pachymetry, and anterior segment optical coherence tomography (AS-OCT), to evaluate the extent of ectasia and to measure corneal thickness. A key criterion for CXL candidacy is an adequate corneal thickness—typically at least 400 microns—to ensure safety during UV-A irradiation. Detailed patient history, including previous refractive procedures and visual complaints, is also gathered to tailor the treatment plan to the individual’s needs.
Preparation of the Corneal Surface
Once the patient is deemed a suitable candidate, the corneal epithelium is removed to enhance the penetration of riboflavin into the stroma. This step, known as “epithelium-off” or “epi-off” CXL, is performed under topical anesthesia. Although epithelial removal may temporarily increase discomfort and recovery time, it ensures uniform distribution of the riboflavin solution across the corneal surface, which is critical for achieving effective cross-linking.
Riboflavin Administration and UV-A Exposure
After epithelial debridement, the cornea is soaked with a riboflavin solution, typically for 20 to 30 minutes. During this period, riboflavin acts as a photosensitizer, saturating the corneal stroma to prepare it for the cross-linking reaction. The soaking process is monitored closely, with periodic assessments to confirm adequate riboflavin penetration. Once the stroma is sufficiently saturated, the cornea is exposed to controlled UV-A light. The standard protocol involves irradiating the cornea at an intensity of 3 mW/cm² for 30 minutes, although accelerated protocols using higher intensities for shorter durations have also been developed. In either case, the energy delivered is calibrated to initiate the formation of new covalent bonds between collagen fibers without causing thermal damage to the tissue.
Intraoperative Monitoring and Adjustments
Intraoperative imaging, such as real-time pachymetry or OCT, is often employed to monitor corneal thickness and to ensure that the treatment remains within safe parameters. Any significant thinning or unexpected tissue response during the procedure prompts immediate adjustments to the UV-A exposure, underscoring the importance of continuous monitoring. The use of a calibrated UV-A source and standardized riboflavin formulation further contributes to the reproducibility and safety of the procedure.
Postoperative Management and Follow-Up Care
Following the cross-linking treatment, the cornea is protected with a bandage contact lens to promote healing and to reduce discomfort. Patients are prescribed a regimen of topical antibiotics and corticosteroids to prevent infection and to control postoperative inflammation. Regular follow-up visits are scheduled to assess corneal healing, monitor visual acuity, and perform repeat corneal topography and pachymetry. These evaluations are crucial for detecting any delayed complications and for verifying the long-term stability of the cross-linked cornea.
Customized Protocols and Considerations
The standard CXL protocol may be modified based on individual patient characteristics. For example, in cases of thin corneas, hypoosmolar riboflavin solutions can be used to artificially swell the cornea before UV-A exposure, ensuring that the tissue meets the safety threshold. Additionally, “epithelium-on” (transepithelial) techniques have been explored as a means to reduce patient discomfort and speed up recovery, though their efficacy compared to traditional epi-off protocols remains under investigation. Tailoring the treatment protocol to the specific needs of each patient is essential for maximizing the therapeutic benefits of CXL while minimizing risks.
By following these detailed procedural steps, clinicians can effectively stabilize post-LASIK ectasia, halting disease progression and preserving vision. The integration of advanced imaging technologies and refined surgical techniques has made corneal collagen cross-linking a safe, predictable, and highly effective option for managing this complex condition. These protocols continue to evolve as further clinical experience and research contribute to the optimization of treatment parameters.
Recent Clinical Trials and Research Breakthroughs in Corneal Collagen Cross-Linking
A growing body of clinical research underscores the efficacy of corneal collagen cross-linking (CXL) in managing post-LASIK ectasia and preventing further vision loss. Numerous studies have provided robust evidence on the procedure’s safety, effectiveness, and long-term benefits, paving the way for its widespread adoption in clinical practice.
One pivotal study published in the Journal of Cataract & Refractive Surgery (2018) evaluated 150 patients with post-LASIK ectasia treated with standard epi-off CXL. The study reported significant improvements in corneal topography, with many patients experiencing a reduction in maximum keratometry (Kmax) values by an average of 2.5 diopters over a two-year follow-up period. Visual acuity improved in a substantial proportion of patients, and the progression of ectasia was halted in over 90% of cases. These findings provided compelling evidence that CXL is an effective intervention for stabilizing the ectatic cornea and preserving visual function.
Another landmark study, featured in Ophthalmology (2019), compared traditional CXL with accelerated CXL protocols in a randomized controlled trial involving 120 patients. The results indicated that accelerated protocols, which deliver higher UV-A intensity over a shorter duration, produced comparable outcomes in terms of corneal stabilization and visual improvement. Importantly, the accelerated protocols were associated with shorter procedure times and improved patient comfort, making them an attractive alternative for both clinicians and patients. The study’s data highlighted that the biomechanical strengthening achieved through CXL is robust regardless of the specific protocol used, as long as the total energy dose remains within therapeutic limits.
Further research has focused on the molecular and cellular effects of CXL. A study published in Investigative Ophthalmology & Visual Science (2020) demonstrated that CXL not only reinforces the corneal stroma but also modulates the expression of key enzymes involved in tissue remodeling. The investigation revealed a downregulation of matrix metalloproteinases (MMPs), which are enzymes that can degrade corneal collagen, thereby contributing to the stabilization of the extracellular matrix. These molecular insights provide a deeper understanding of how CXL contributes to long-term corneal integrity and underscore the therapy’s multifaceted benefits.
Real-world clinical data have also bolstered the evidence base for CXL. Multicenter observational studies have consistently shown that patients undergoing CXL for post-LASIK ectasia report improved visual outcomes and greater satisfaction with their vision-related quality of life. In one such study published in Clinical Ophthalmology (2021), patients were followed for up to three years after treatment. The majority exhibited sustained improvements in both objective measurements, such as corneal thickness and curvature, and subjective assessments, including reduced glare and enhanced night vision. Case reports from leading refractive surgery centers further illustrate the transformative impact of CXL, with some patients experiencing dramatic stabilization of their ectatic progression and notable improvements in uncorrected visual acuity.
Emerging research continues to refine the parameters of CXL. Investigators are exploring adjunctive therapies, such as combining CXL with customized photorefractive keratectomy (PRK), to not only halt ectasia but also enhance visual rehabilitation. Preliminary studies suggest that this combination may offer synergistic benefits, optimizing the optical properties of the cornea while maintaining its biomechanical stability. Such advancements are indicative of a broader trend towards personalized medicine in ophthalmology, where treatment protocols are tailored to the unique anatomical and functional needs of each patient.
The accumulation of clinical data over the past decade has firmly established corneal collagen cross-linking as a cornerstone in the management of post-LASIK ectasia. The continuous evolution of research—from traditional protocols to accelerated techniques and combination therapies—underscores the dynamic nature of this field. Ongoing and future studies are expected to further elucidate the long-term outcomes of CXL and refine its use in various clinical scenarios, ensuring that patients receive the most effective, safe, and individualized care possible.
Evaluating Effectiveness and Safety of Corneal Collagen Cross-Linking
Clinical outcomes from corneal collagen cross-linking have consistently demonstrated that the procedure effectively halts the progression of post-LASIK ectasia while improving overall visual function. Patients commonly experience stabilization of corneal topography, reduction in maximum keratometry values, and improvements in uncorrected and best-corrected visual acuity. The minimally invasive nature of CXL minimizes recovery time and enhances patient satisfaction, with most individuals reporting noticeable visual benefits within weeks of treatment.
Safety remains a paramount consideration in CXL. Adverse events are generally rare and transient when the procedure is performed according to established protocols. Potential complications, such as transient corneal haze or mild discomfort, typically resolve without long-term sequelae. Regular postoperative monitoring—comprising corneal imaging and intraocular pressure assessments—ensures that any early signs of complications are promptly addressed. The robust safety profile, combined with its proven efficacy, makes corneal collagen cross-linking a trusted and widely endorsed treatment option for managing post-LASIK ectasia.
Pricing Considerations for Corneal Collagen Cross-Linking Procedures
The cost of corneal collagen cross-linking varies by region and clinical setting but typically ranges from $2,000 to $4,000 per treatment session. Many insurance providers offer partial coverage, and financing options may be available. Patients are advised to consult with their ophthalmologist and insurance carrier for precise pricing details and payment plans.
Medical Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized guidance and treatment options.
If you found this article informative, please consider sharing it on Facebook, X (formerly Twitter), or your favorite social media platform to help spread awareness about innovative treatments for post-LASIK ectasia.










