What is Post-surgical Glaucoma?
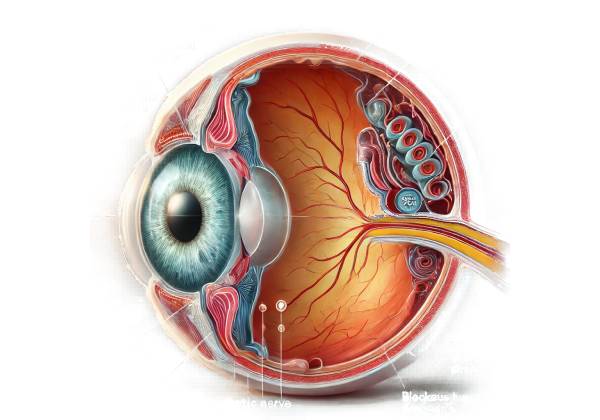
Post-surgical glaucoma, also known as secondary glaucoma, is a condition characterized by an increase in intraocular pressure (IOP) following ocular surgery. This condition can develop following a variety of eye surgeries, such as cataract extraction, corneal transplantation, retinal surgery, and glaucoma surgery itself. Increased IOP can cause optic nerve damage and vision loss if not treated promptly and effectively.
Types of Post-Surgical Glaucoma
There are several types of post-surgical glaucoma, each with a different surgical procedure and mechanism of IOP elevation:
- Acute Postoperative Glaucoma: This type develops soon after surgery, typically within the first few days. It is frequently the result of inflammation, hemorrhage, or mechanical blockages.
- Chronic Postoperative Glaucoma: This develops weeks or months after surgery and can be caused by scarring, prolonged inflammation, or changes in the eye’s drainage system.
- Secondary Angle-Closure Glaucoma: This occurs when the angle between the iris and the cornea closes, preventing the outflow of aqueous humor. It can be caused by lens-related issues or changes in the iris configuration following surgery.
Pathophysiology
The pathophysiology of post-surgical glaucoma involves various mechanisms based on the type of surgery and individual patient factors:
- Inflammation: Surgery causes an inflammatory response in the eyes. This can cause trabecular meshwork swelling and decreased aqueous humor outflow, resulting in high IOP. Chronic inflammation can cause fibrosis and scarring, which further obstructs drainage pathways.
- Hemorrhage: Intraoperative or postoperative bleeding can clog the trabecular meshwork or Schlemm’s canal, preventing fluid flow.
- Lens-Related Factors: In cataract surgery, lens fragments or residual lens material may obstruct the trabecular meshwork. Furthermore, an improperly positioned intraocular lens (IOL) can result in mechanical blockage.
- Mechanical Blockage: Various surgical instruments or devices used during eye surgery may unintentionally obstruct aqueous outflow pathways.
- Scarring and Fibrosis: Postoperative healing can result in scarring around the trabecular meshwork or within the drainage angle, obstructing fluid outflow and causing chronic intraocular pressure elevation.
Risk Factors
Several factors increase the risk of developing postoperative glaucoma:
- Preexisting Glaucoma: Patients with a history of glaucoma are at an increased risk due to preexisting damage and compromised outflow pathways.
- Inflammatory Conditions: Previous inflammatory eye conditions can worsen postoperative inflammation, increasing the risk of glaucoma.
- Complex Surgeries: Longer or more complicated surgeries, such as those with multiple procedures, may increase the risk of inflammation and mechanical complications.
- Age: Older patients are at a higher risk due to decreased regenerative capacity and preexisting ocular conditions.
- Systemic Conditions: Diabetes and hypertension can slow healing and increase the risk of postoperative complications, such as glaucoma.
Clinical Presentation
The symptoms of post-surgical glaucoma can differ depending on the type and timing of the condition:
- Acute Postoperative Glaucoma: Patients may experience symptoms within a few days of surgery, such as:
- Severe Eye Pain: Acute and intense pain in the affected eye.
- Redness: Eye redness caused by inflammation or hemorrhage.
- Blurred Vision: A sudden decrease in vision.
- Halos Around Lights: The perception of halos, especially at nighttime.
- Nausea and vomiting: These can occur as a result of a sudden increase in IOP.
- Chronic Postoperative Glaucoma: This type develops more gradually and can present with:
- Gradual Vision Loss: A progressive loss of peripheral vision.
- Mild to Moderate Eye Pain: Persistent but not as severe as acute glaucoma.
- Ocular Hypertension: Increased IOP detected during routine check-ups.
- No Symptoms: Many patients may remain asymptomatic until significant vision loss occurs.
Complications
If left untreated, post-surgical glaucoma can cause a number of serious complications:
- Optic Nerve Damage: Prolonged elevated IOP can irreversibly damage the optic nerve, resulting in permanent vision loss.
- Corneal Edema: High IOP can cause swelling of the cornea, resulting in pain and blurred vision.
- Secondary Infections: Inflammation and mechanical blockages can make the eye vulnerable to secondary infections.
- Retinal Detachment: In rare cases, severe inflammation or hemorrhage can cause retinal detachment, which is a vision-threatening condition.
Differential Diagnosis
Diagnosing post-surgical glaucoma requires distinguishing it from other causes of elevated IOP and similar ocular conditions.
- Primary Open-Angle Glaucoma is chronic and progressive, with no recent surgical history.
- Primary Angle-Closure Glaucoma: Acute onset, typically unrelated to recent surgery.
- Uveitis: Inflammation of the uveal tract can cause elevated IOP, but the causes vary.
- Ocular Hypertension: Elevated intraocular pressure (IOP) without optic nerve damage, usually without symptoms.
- Infectious Endophthalmitis: A post-surgical infection that causes pain, redness, and vision loss, but often includes signs of severe infection.
Epidemiology
The prevalence of post-surgical glaucoma varies according to the type of surgery and population studied. According to studies, the incidence can range between 1% and 10% in various surgical contexts. It is more common in patients undergoing complex surgeries, those with preexisting glaucoma, and certain high-risk groups, such as the elderly or those with inflammatory eye conditions.
Effects on Quality of Life
Post-surgical glaucoma can have a significant impact on a patient’s quality of life. Acute cases can cause severe pain and immediate vision loss, whereas chronic cases can result in gradual but irreversible vision loss. The need for ongoing monitoring, as well as the possibility of multiple treatments or surgeries, can place a financial and emotional burden on patients.
Prognosis
The prognosis for post-surgical glaucoma is determined by when the disease is diagnosed and how effective treatment is. Early detection and treatment can prevent serious vision loss and improve outcomes. However, delayed diagnosis or inadequate treatment can result in permanent optic nerve damage and blindness.
Diagnostic Techniques for Post-Surgical Glaucoma
To confirm the diagnosis and understand the underlying cause, a clinical examination, imaging studies, and, in some cases, laboratory tests are used.
Clinical Examination
A comprehensive clinical examination is the first step in diagnosing post-surgical glaucoma:
- Visual Acuity Test: This test determines how well a patient sees at different distances. It aids in determining how elevated IOP affects vision.
- Intraocular Pressure (IOP) Measurement: The eye care professional uses tonometry to measure the pressure within the eye. Elevated IOP is a strong indicator of glaucoma.
- Slit-Lamp Examination: This procedure uses a specialized microscope to examine the anterior and posterior segments of the eye. It can detect inflammation, hemorrhage, lens position, and other abnormalities.
- Gonioscopy: This procedure uses a special lens to examine the angle between the iris and the cornea, allowing for the detection of angle closure or drainage system abnormalities.
Imaging Studies
Imaging studies provide detailed views of the eye’s internal structures and aid in diagnosing and monitoring post-surgical glaucoma.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve. It is useful for detecting optic nerve damage and retinal changes caused by glaucoma.
- Ultrasound Biomicroscopy: This imaging technique uses high-frequency sound waves to visualize the anterior segment of the eye. It is especially useful for examining the ciliary body, angle structures, and any postoperative changes.
- Anterior Segment Optical Coherence Tomography (AS-OCT): This technique evaluates anterior segment structures, such as the angle and positioning of intraocular lenses.
Lab Tests
In some cases, laboratory tests may be required to identify underlying causes or associated systemic conditions.
- Blood Tests: Routine blood tests can detect systemic conditions such as diabetes or inflammatory diseases, which can lead to postoperative complications.
- Aqueous Humor Analysis: In cases of suspected infection or inflammation, a sample of aqueous humor may be tested for pathogens or inflammatory markers.
Effective Post-surgical Glaucoma Management options
Managing post-surgical glaucoma requires a multifaceted approach that includes medical treatments, laser procedures, and surgical interventions. The goal is to reduce intraocular pressure (IOP) to avoid optic nerve damage and preserve vision.
Medical Management
- Topical Medications: The first line of treatment is usually eye drops to reduce IOP. These medications fall into several categories:
- Prostaglandin Analogues: Drugs such as latanoprost and bimatoprost increase the flow of aqueous humor, lowering IOP.
- Beta-Blockers: Timolol and betaxolol reduce the production of aqueous humor, which helps to lower IOP.
- Alpha Agonists: Brimonidine and apraclonidine decrease aqueous humor production while increasing outflow.
- Carbonic Anhydrase Inhibitors: These drugs, available as eye drops (e.g., dorzolamide, brinzolamide) or oral medications (e.g., acetazolamide), reduce the production of aqueous humor.
- Rho Kinase Inhibitors: Netarsudil promotes aqueous humor outflow via the trabecular meshwork.
- Oral Medications: If topical medications are ineffective, oral carbonic anhydrase inhibitors such as acetazolamide may be prescribed to further reduce IOP.
- Anti-Inflammatory Agents: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids can be used to treat inflammation, which is a common cause of high IOP after surgery.
Laser Therapy
Laser procedures can be extremely effective in treating post-surgical glaucoma:
- Laser Trabeculoplasty: This procedure utilizes a laser to improve aqueous humor drainage through the trabecular meshwork.
- Argon Laser Trabeculoplasty (ALT): This procedure uses an argon laser to create small burns in the trabecular meshwork, which improves fluid outflow.
- Selective Laser Trabeculoplasty (SLT): A low-energy laser that targets pigmented cells in the trabecular meshwork while minimizing damage to surrounding tissue.
- Laser Iridotomy: Used to treat angle-closure glaucoma, this procedure creates a small hole in the iris to improve aqueous fluid flow.
Surgical Management
Surgery is frequently required when medical and laser treatments fail to control IOP effectively:
- Trabeculectomy: This common surgical procedure creates a new drainage pathway by removing a portion of the trabecular meshwork. It allows aqueous humor to drain into the space beneath the conjunctiva, resulting in a bleb. Regular monitoring is required to ensure that the bleb remains operational.
- Glaucoma Drainage Devices: These devices, also known as tube shunts, help drain excess aqueous humor from the eye and into an external reservoir. Examples include the Ahmed valve, the Baerveldt implant, and the Molteno implant.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures are less invasive than traditional surgeries and frequently used in conjunction with cataract surgery. Examples include the iStent, Hydrus Microstent, and Xen Gel Stent. These devices improve aqueous outflow by reducing complications and shortening recovery time.
- Cyclophotocoagulation: This procedure employs a laser to inhibit the ciliary body’s ability to produce aqueous humor. It is possible to perform it either externally (transscleral cyclophotocoagulation) or internally (endocyclophotocoagulation).
Post-operative Care and Monitoring
Effective postoperative care is critical for ensuring successful outcomes and avoiding complications.
- Medications: Typically, patients are given antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation. It is critical to adhere to the ophthalmologist’s medication regimen.
- Follow-Up Visits: Regular follow-up visits are scheduled to monitor the healing process, check the IOL’s positioning, and evaluate visual acuity. These visits aid in the early detection and treatment of complications such as infection, raised intraocular pressure, and lens displacement.
- Activity Restrictions: Patients should avoid strenuous activities, heavy lifting, and rubbing their eyes during the initial healing period. Protective eyewear may be prescribed to protect the eye from injury and bright light.
Lifestyle and Supportive Measures
- Diet and Exercise: A healthy lifestyle, which includes a well-balanced diet and regular exercise, can help to improve overall eye health. Patients should avoid activities that cause significant increases in IOP, such as heavy lifting and certain yoga positions.
- Protective Eyewear: Wearing protective eyewear during activities that could injure the eye is critical, especially after surgery.
Trusted Resources and Support
Books
- “Cataract Surgery: A Patient’s Guide to Treatment” by Robert S. Feder, MD
- This book provides comprehensive information on cataract surgery, postoperative care, and managing complications such as glaucoma.
- “Glaucoma: A Patient’s Guide to the Disease” by Graham E. Trope, MD
- An informative resource that covers various types of glaucoma, including secondary glaucoma, and offers insights into diagnosis and treatment options.
Organizations
- American Academy of Ophthalmology (AAO)
- Website: www.aao.org
- The AAO provides extensive resources on glaucoma, including patient education materials, research updates, and professional guidelines.
- Glaucoma Research Foundation (GRF)
- Website: www.glaucoma.org
- The GRF offers valuable information on glaucoma types, treatment options, and ongoing research, along with support resources for patients and caregivers.






