Posterior uveitis is an inflammatory condition that affects the back portion of the uveal tract in the eye. The uveal tract consists of the iris, ciliary body, and choroid, with posterior uveitis primarily affecting the choroid and retina. If not diagnosed and treated promptly, this condition can cause significant visual impairment. Posterior uveitis is a subset of uveitis that is classified as anterior, intermediate, posterior, or panuveitis according to the anatomical location of the inflammation.
Anatomy and Physiology
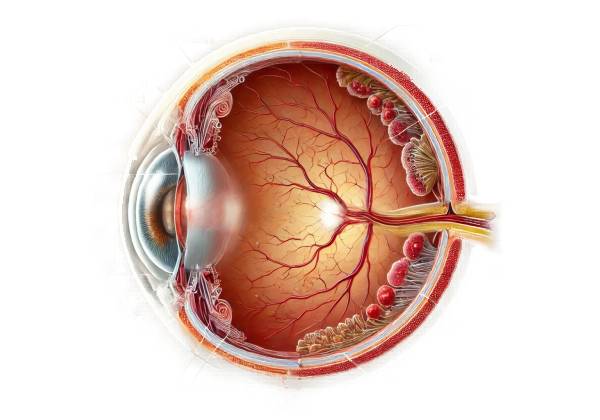
Understanding posterior uveitis requires a basic understanding of the eye’s anatomy, particularly the uveal tract. The uveal tract, also known as the uvea, is the eye’s middle layer, located between the sclera (the outer protective layer) and the retina. The uvea is highly vascular and composed of three parts:
- Iris: The colored part of the eye that surrounds the pupil and controls how much light enters the eye.
- Ciliary Body: Located behind the iris, it generates aqueous humor and houses the ciliary muscle, which aids in lens accommodation.
- Choroid: A layer of blood vessels and connective tissue located between the sclera and the retina that supplies nutrients and oxygen to the retina’s outer layers.
Posterior uveitis affects the choroid and can spread to the retina (chorioretinitis), retinal vessels (vasculitis), and optic nerve (neuroretinitis).
Etiology and Risk Factors
Infectious, non-infectious, and idiopathic factors can all contribute to posterior uveitis. Identifying the underlying cause is critical for successful treatment and management. Common etiological factors include the following:
- Infectious causes:
Toxoplasmosis, caused by the parasite Toxoplasma gondii, is one of the most common causes of infectious posterior uveitis.
- Cytomegalovirus (CMV): Especially in immunocompromised people, like those with HIV/AIDS.
- Tuberculosis (TB): Caused by Mycobacterium tuberculosis.
Treponema pallidum causes syphilis, a sexually transmitted infection. - Herpes Viruses: This includes the herpes simplex virus (HSV) and the varicella-zoster virus.
- Noninfectious Causes:
- Autoimmune diseases include sarcoidosis, Behçet’s disease, and Vogt-Koyanagi-Harada (VKH) disease.
- Idiopathic: In some cases, the cause is unknown despite extensive investigation.
- Systematic Associations:
- Systemic Lupus Erythematosus (SLE): An autoimmune disease that affects several organs, including the eyes.
- Rheumatoid Arthritis is another autoimmune condition that can cause ocular symptoms.
- Inflammatory Bowel Disease (IBD): This includes Crohn’s disease and ulcerative colitis.
Clinical Presentation
The symptoms of posterior uveitis vary according to the underlying cause, severity, and duration of the inflammation. Common symptoms include:
- Visual Disturbances: Common complaints include blurry vision, floaters, and reduced visual acuity. Floaters are small, dark shapes that move across the field of vision as a result of inflammatory cells and debris in the vitreous humor.
- Photophobia: Extreme light sensitivity that causes significant discomfort.
- Eye Pain: Although less common than anterior uveitis, some patients may experience dull, aching pain.
- Redness and Tearing: Mild to moderate redness of the eye and increased tear production may occur.
Pathophysiology
The pathophysiology of posterior uveitis includes an inflammatory response that targets the choroid and may spread to other structures within the eye. This inflammation can cause the blood-retinal barrier to break down, allowing inflammatory cells and mediators into the retinal tissue. If left untreated, the resulting inflammation can cause tissue damage, edema, and scarring, eventually leading to vision loss.
- Immune Response: In autoimmune or idiopathic conditions, the immune system mistakenly targets healthy tissues within the eye, resulting in chronic inflammation.
- Infectious Inflammation: In infectious conditions, the body’s immune response to pathogens causes localized inflammation in the eye.
Complications
If not treated properly, posterior uveitis can cause a number of complications:
- Cystoid Macular Edema (CME): Swelling of the macula, the central part of the retina, that can severely impair vision.
- Retinal Detachment: Severe inflammation can cause retinal tears and detachments.
- Glaucoma: Increased intraocular pressure due to inflammation and scarring can result in glaucoma.
- Cataracts: Chronic inflammation and corticosteroid use can both cause cataracts.
- Optic Neuropathy: Involvement of the optic nerve can cause permanent vision loss.
Epidemiology
Posterior uveitis is less common than anterior uveitis, but it is more severe and vision-threatening. It can affect people of all ages, but the prevalence and causes differ by region and population. Toxoplasmosis, for example, is a more common cause of posterior uveitis in specific areas due to environmental and dietary factors.
Differential Diagnosis
Differential diagnosis is critical for distinguishing posterior uveitis from other conditions with similar symptoms:
- Retinal Detachment: Can cause visual disturbances and floaters.
- Central Serous Chorioretinopathy (CSC) is characterized by fluid accumulation beneath the retina.
- Age-Related Macular Degeneration (AMD) is a common cause of vision loss in older adults, characterized by drusen and geographic atrophy.
- Diabetic Retinopathy is a diabetes complication that causes retinal changes and vision loss.
Diagnosing Posterior Uveitis Effectively
Diagnosing posterior uveitis requires a multifaceted approach that includes clinical evaluation, advanced imaging techniques, and laboratory tests to determine the underlying cause and severity of inflammation.
Clinical Examination
- Visual Acuity Test: This basic test determines how well a patient can see at different distances. It is useful in determining the impact of inflammation on vision.
- Slit-Lamp Examination: This procedure involves examining the anterior and posterior segments of the eye with a specialized microscope. It can detect inflammatory cells in the vitreous humor, retinal lesions, and choroidal thickening.
- Fundus Examination: Using ophthalmoscopy or fundus photography, the ophthalmologist can directly visualize the retina and choroid to assess inflammation and structural changes.
Imaging Studies
- Optical Coherence Tomography (OCT) is a non-invasive imaging technique that generates detailed cross-sectional images of the retina. It is especially effective at detecting macular edema, retinal thickening, and structural abnormalities.
- Fluorescein Angiography: This test involves injecting a fluorescent dye into the bloodstream and photographing the dye as it travels through the retinal vessels. It aids in detecting areas of leakage, blockage, or abnormal blood vessels.
- Indocyanine Green Angiography (ICG): ICG uses a different dye to provide a better view of the choroidal circulation. It is effective at detecting choroidal inflammation and other vascular abnormalities.
- Ultrasound B-Scan: This imaging technique creates detailed images of the posterior segment of the eye using high-frequency sound waves. It is especially useful when opacities in the vitreous or lens obscure the view of the retina.
Lab Tests
- Blood Tests: Routine blood tests, such as complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), aid in the detection of systemic inflammation or infection. To identify infectious agents and autoimmune markers, specific blood tests may include:
- Toxoplasmosis Serology: Look for antibodies to Toxoplasma gondii.
- Syphilis Serology: Includes RPR and FTA-ABS tests.
- Tuberculosis Testing: A tuberculin skin test (TST) or interferon-gamma release assays (IGRAs) can detect latent tuberculosis infection.
- Viral Serology: Detects antibodies to herpes simplex virus (HSV), cytomegalovirus (CMV), and varicella-zoster virus (VZV).
- Autoimmune Markers: Testing for antinuclear antibodies (ANA), rheumatoid factor (RF), and specific autoantibodies linked to conditions such as sarcoidosis and Behçet’s disease.
- Aqueous or Vitreous Humor Analysis: In some cases, samples of the aqueous or vitreous humor may be collected using a fine needle and tested for infectious agents or inflammatory markers.
- Chest X-Ray or CT Scan: These imaging modalities can be used to diagnose systemic conditions like sarcoidosis or tuberculosis, which can cause posterior uveitis.
Treatment Options for Posterior Uveitis
Managing posterior uveitis entails identifying the underlying cause of the inflammation, controlling symptoms, and avoiding complications. The treatment plan is tailored to each patient’s unique situation, including the cause of the uveitis, the severity of the inflammation, and the patient’s overall health.
Medical Management
- Corticosteroids: Corticosteroids are the main treatment for reducing inflammation in posterior uveitis. They can be administered in various ways:
Prednisone is a common oral corticosteroid used to control systemic inflammation. The dosage is based on the severity of the inflammation and the patient’s response to treatment.
- Topical Corticosteroids: Eye drops containing prednisolone acetate are used in milder cases where inflammation is limited to the eyes.
- Periocular or Intravitreal Injections: In more severe cases, corticosteroids can be injected around or into the eye to deliver a high dose of medication directly to the site of inflammation.
- Immunosuppressive Agents: Immunosuppressive medications may be required for patients who do not respond well to corticosteroids or who require long-term treatment.
- Methotrexate: A commonly used immunosuppressive medication that can help manage chronic inflammation.
- Azathioprine is another option for long-term immunosuppression.
- Mycophenolate Mofetil: Effective at reducing severe inflammation.
- Cyclosporine and Tacrolimus: Used to suppress the immune system in cases where other treatments have failed.
- Biologic Agents: Biologics target specific immune system components and can be extremely effective for severe or refractory uveitis.
- TNF Inhibitors: Infliximab and adalimumab are two widely used biologics that inhibit tumor necrosis factor (TNF), a key inflammatory cytokine.
- Interleukin Inhibitors: Tocilizumab (targeting IL-6) and secukinumab (targeting IL-17) may be effective in certain types of autoimmune uveitis.
- Antimicrobial Therapy: If an infectious cause is identified, the following antimicrobial therapy is initiated:
- Antibiotics: Used to treat bacterial infections such as tuberculosis and syphilis.
- Antivirals: For viral infections like CMV and HSV.
- Antiparasitics: Used to treat infections such as toxoplasmosis.
Adjunctive therapies
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Ibuprofen and naproxen can be used in conjunction with other treatments to reduce inflammation and pain.
- Antioxidant Supplements: Some research suggests that antioxidants such as vitamin C and E can help reduce oxidative stress in the eye.
Surgical Intervention
Surgery is considered when medical treatment fails to control the inflammation or when complications such as retinal detachment or persistent macular edema occur.
- Vitrectomy: Removing the vitreous humor can help reduce inflammation and improve retinal visibility during treatment.
- Laser Therapy: Used to treat complications such as retinal neovascularization or to close retinal tears.
Monitoring and Follow-up
Patients with posterior uveitis require regular follow-up to monitor treatment efficacy, adjust medications, and detect complications early.
- Ocular Examinations: Schedule regular eye exams to assess inflammation and visual acuity.
- Imaging Studies: Repeat OCT or angiography to track changes in the retina and choroid.
- Blood Tests: Periodic blood tests to monitor for systemic medication side effects and to assess the status of any underlying systemic disease.
Lifestyle and Supportive Measures
- Patient Education: It is critical to educate patients about the chronic nature of uveitis, the importance of medication adherence, and how to identify signs of recurrence.
- Support Groups: Linking patients with support groups can provide emotional support and shared experiences, which can be especially beneficial when managing a chronic condition.
Trusted Resources and Support
Books
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
- This book provides an in-depth understanding of uveitis, including posterior uveitis, with detailed information on diagnosis, treatment, and clinical management.
- “Ocular Immunology in Health and Disease” by Stephen Foster and Albert Vitale
- An authoritative resource covering the immune mechanisms underlying ocular diseases, including posterior uveitis, with insights into current treatment strategies.
Organizations
- American Uveitis Society (AUS)
- Website: www.uveitissociety.org
- The AUS provides resources for patients and healthcare professionals, including information on the latest research, treatment guidelines, and support networks for those affected by uveitis.
- National Eye Institute (NEI)
- Website: www.nei.nih.gov
- The NEI offers comprehensive information on eye health, research updates, and educational resources for patients and families dealing with various ocular conditions, including posterior uveitis.






