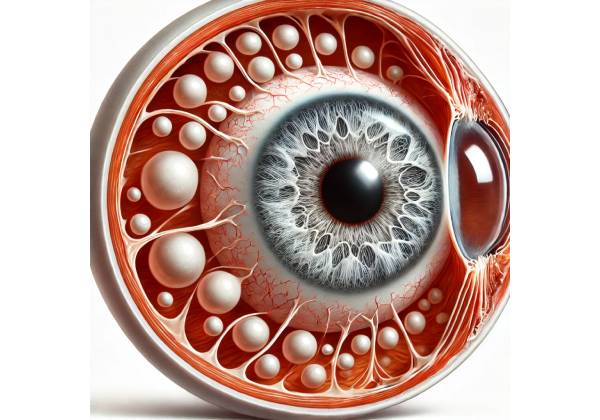
What is Scleral Staphyloma?
Scleral staphyloma is a rare and serious ocular condition characterized by the abnormal thinning and outward bulging of the sclera, the white, tough outer layer of the eye. This condition results in the formation of a localized or diffuse protrusion of the uveal tissue (which includes the iris, ciliary body, and choroid) through the weakened scleral wall. The bulging typically occurs in areas of the eye where the sclera has been compromised by disease, trauma, or degeneration, leading to a decrease in its structural integrity.
Scleral staphylomas can occur in different parts of the eye and are classified based on their location. The most common types are anterior staphyloma, which involves the cornea and the anterior segment of the sclera; equatorial staphyloma, which occurs around the equator of the eyeball; and posterior staphyloma, which affects the back of the eye, often involving the optic nerve and surrounding retina. Among these, posterior staphyloma is the most frequently encountered and is most commonly associated with high myopia (severe nearsightedness).
Pathophysiology of Scleral Staphyloma
The pathophysiology of scleral staphyloma involves a combination of factors that lead to scleral thinning and weakening. These factors may include chronic inflammation, increased intraocular pressure (IOP), degenerative changes, or trauma. The sclera, composed primarily of collagen fibers, provides structural support to the eye and maintains its shape. When the sclera is compromised, it can no longer withstand the internal pressure exerted by the vitreous body and other intraocular contents, leading to the outward bulging of the uveal tissue.
- Degenerative Changes: In conditions such as high myopia, the elongation of the eyeball leads to stretching and thinning of the sclera, particularly in the posterior segment. Over time, this thinning can progress to form a posterior staphyloma, which can cause significant visual disturbances and increase the risk of retinal complications, including retinal detachment and macular degeneration.
- Inflammation and Scleritis: Chronic inflammation of the sclera, as seen in conditions like scleritis, can lead to the breakdown of collagen and other extracellular matrix components, weakening the scleral tissue. Scleritis-associated staphylomas are often seen in the anterior segment and may be accompanied by redness, pain, and other signs of inflammation.
- Trauma: Ocular trauma, including blunt or penetrating injuries, can result in localized damage to the sclera. If the scleral tissue is not properly repaired or if the healing process is compromised, a staphyloma may develop at the site of injury. This is more likely to occur in cases where the trauma has led to a rupture of the sclera or where there has been surgical intervention that weakens the scleral wall.
- Increased Intraocular Pressure: Conditions that cause sustained elevation of intraocular pressure, such as glaucoma, can exert additional stress on the scleral wall, particularly in areas where the sclera is already weakened. Over time, this pressure can contribute to the formation of staphylomas, particularly in the posterior segment of the eye.
- Infectious and Autoimmune Disorders: Certain infectious and autoimmune diseases can affect the sclera, leading to its thinning and degeneration. For example, syphilitic scleritis, tuberculosis, and other granulomatous diseases can cause localized damage to the sclera, increasing the risk of staphyloma formation.
Clinical Presentation of Scleral Staphyloma
The clinical presentation of scleral staphyloma varies depending on the location, size, and underlying cause of the condition. Patients may present with a range of symptoms, including visual disturbances, pain, and cosmetic concerns.
- Visual Impairment: The most common symptom associated with scleral staphyloma is a progressive decline in visual acuity. This is particularly true for posterior staphylomas, which can affect the macula, the central part of the retina responsible for sharp, detailed vision. Patients may experience blurred vision, distortion of images (metamorphopsia), and difficulty with activities such as reading or recognizing faces. In advanced cases, staphylomas can lead to complications like retinal detachment, which can cause sudden, severe vision loss.
- Pain and Discomfort: Anterior staphylomas, which involve the cornea and anterior sclera, may be associated with significant pain and discomfort, particularly if the underlying cause is inflammatory, such as scleritis. Patients may report eye redness, tenderness, and sensitivity to light (photophobia). The presence of a visible bulge on the surface of the eye can also be a source of discomfort.
- Cosmetic Concerns: The outward bulging of the sclera and the associated uveal tissue can lead to a noticeable deformity of the eye, particularly in cases of anterior or equatorial staphylomas. This cosmetic deformity can be distressing for patients and may lead to self-consciousness or social anxiety.
- Complications: Scleral staphylomas are associated with a number of serious complications that can further impair vision and ocular health. These include retinal detachment, which occurs when the retina separates from the underlying tissue due to traction from the staphyloma. Macular degeneration and choroidal neovascularization are also potential complications of posterior staphylomas, particularly in patients with high myopia.
Classification of Scleral Staphylomas
Scleral staphylomas are classified based on their anatomical location within the eye. The main types include:
- Anterior Staphyloma: This type involves the cornea and anterior sclera and is often associated with conditions like scleritis, corneal ulcers, or trauma. The protrusion is usually visible on the surface of the eye and may be associated with pain and inflammation.
- Intercalary Staphyloma: This type occurs between the limbus and the equator of the eye and is typically associated with a history of uveitis or trauma. It often involves the ciliary body and can lead to significant visual impairment if not properly managed.
- Equatorial Staphyloma: Equatorial staphylomas occur around the equator of the eyeball and are often seen in conditions like high myopia or after scleral surgery. These staphylomas can cause distortion of the retina and are associated with a higher risk of retinal detachment.
- Posterior Staphyloma: The most common and clinically significant type, posterior staphylomas involve the back of the eye and are strongly associated with high myopia. These staphylomas can lead to progressive myopic maculopathy, a condition characterized by degenerative changes in the macula, and are a major cause of visual impairment in patients with severe myopia.
Epidemiology and Risk Factors
Scleral staphyloma is a relatively rare condition, with its prevalence varying based on the underlying cause and population studied. Posterior staphyloma is more commonly seen in individuals with high myopia, particularly in populations where myopia is prevalent. The condition is more likely to develop in middle-aged and older adults, although it can occur at any age, depending on the underlying factors.
Key risk factors for developing scleral staphyloma include:
- High Myopia: Severe nearsightedness is one of the most significant risk factors for posterior staphyloma. The elongation of the eyeball in high myopia leads to stretching and thinning of the sclera, increasing the likelihood of staphyloma formation.
- Chronic Inflammation: Conditions such as scleritis, uveitis, and other inflammatory eye diseases can weaken the sclera and predispose individuals to staphyloma development.
- Trauma: Previous ocular trauma or surgery, particularly procedures that involve manipulation of the sclera, can increase the risk of staphyloma formation, particularly if the scleral tissue does not heal properly.
- Genetic Predisposition: Certain genetic conditions, such as connective tissue disorders (e.g., Ehlers-Danlos syndrome), may increase the susceptibility to scleral thinning and staphyloma formation.
- Infectious Diseases: Infectious conditions that affect the sclera, such as syphilis or tuberculosis, can lead to localized scleral thinning and increase the risk of staphyloma.
Understanding the pathophysiology, clinical presentation, and risk factors of scleral staphyloma is crucial for accurate diagnosis and effective management. Early detection and appropriate intervention are key to preventing the serious complications associated with this condition.
Diagnostic Methods
Diagnosing scleral staphyloma involves a combination of clinical examination, imaging studies, and, in some cases, specialized tests to assess the extent of scleral thinning, the degree of uveal protrusion, and the presence of any associated complications.
Clinical Examination
A thorough clinical examination by an ophthalmologist is the first step in diagnosing scleral staphyloma. The examination typically includes:
- Visual Acuity Test: This test measures the patient’s ability to see at various distances and helps assess the impact of the staphyloma on vision. A decline in visual acuity, particularly if associated with high myopia or other risk factors, may indicate the presence of a posterior staphyloma.
- Slit-Lamp Biomicroscopy: Slit-lamp biomicroscopy is a key tool for examining the anterior segment of the eye. It allows the ophthalmologist to visualize the sclera, cornea, and anterior chamber in detail. In cases of anterior or intercalary staphyloma, slit-lamp examination can reveal the characteristic bulging of the sclera and any associated inflammation or scarring.
- Fundoscopy: Fundoscopy, also known as ophthalmoscopy, is used to examine the posterior segment of the eye, including the retina, optic disc, and choroid. This examination is particularly important for detecting posterior staphylomas, as it allows the ophthalmologist to assess the posterior sclera and identify any associated retinal changes, such as retinal detachment, macular degeneration, or choroidal neovascularization. The characteristic outward bulging of the sclera in posterior staphyloma can often be seen during fundoscopy, particularly in patients with high myopia.
Imaging Studies
Imaging studies are crucial in the diagnosis and evaluation of scleral staphyloma. These techniques provide detailed information about the structure of the sclera, the extent of uveal protrusion, and the condition of the surrounding ocular tissues.
- Ultrasound Biomicroscopy (UBM): UBM uses high-frequency sound waves to create detailed images of the anterior segment of the eye, including the sclera and ciliary body. UBM is particularly useful in evaluating anterior and intercalary staphylomas, allowing the ophthalmologist to assess the depth of scleral thinning and the degree of uveal protrusion. This imaging technique can also help differentiate scleral staphyloma from other anterior segment abnormalities, such as corneal ectasia.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique that provides high-resolution cross-sectional images of the retina and optic nerve. While OCT is primarily used to evaluate the posterior segment of the eye, it is especially valuable in assessing the impact of posterior staphylomas on the macula and surrounding retinal structures. OCT can detect retinal thinning, macular degeneration, and other changes associated with posterior staphyloma, helping guide treatment decisions.
- B-Scan Ultrasonography: B-scan ultrasonography is a diagnostic imaging technique that uses sound waves to create cross-sectional images of the eye, including the sclera, retina, and choroid. This method is particularly useful for assessing posterior staphylomas, especially when the view of the retina is obscured by media opacities such as cataracts or vitreous hemorrhage. B-scan can help visualize the extent of scleral thinning and detect associated complications such as retinal detachment.
- Magnetic Resonance Imaging (MRI): MRI is a non-invasive imaging technique that provides detailed images of the eye and orbit. MRI is particularly valuable in evaluating the entire globe and surrounding orbital structures, making it useful for detecting posterior staphylomas and assessing their impact on adjacent tissues. MRI can also be helpful in cases where there is a suspicion of an underlying systemic condition, such as connective tissue disorders, that may be contributing to scleral thinning.
Additional Diagnostic Tests
In some cases, additional diagnostic tests may be required to further evaluate the scleral staphyloma and its potential impact on ocular health.
- Intraocular Pressure Measurement: Measuring intraocular pressure (IOP) is an important part of the diagnostic workup for scleral staphyloma, particularly in patients with a history of glaucoma or ocular hypertension. Elevated IOP can exacerbate scleral thinning and increase the risk of staphyloma formation. Regular monitoring of IOP is crucial for managing patients with scleral staphyloma, especially those with associated glaucoma.
- Corneal Topography: Corneal topography is a non-invasive imaging technique that maps the surface curvature of the cornea. While it is primarily used to diagnose and monitor corneal ectatic disorders, corneal topography can also be useful in cases of anterior staphyloma that involve the cornea. This technique can help assess the degree of corneal distortion and guide decisions regarding refractive correction or surgical intervention.
- Electroretinography (ERG): ERG is a diagnostic test that measures the electrical activity of the retina in response to light stimuli. In patients with posterior staphyloma, ERG can help assess the functional status of the retina, particularly in cases where there is concern about retinal degeneration or detachment. Abnormal ERG results may indicate the need for further evaluation or treatment.
Differential Diagnosis
Scleral staphyloma must be differentiated from other conditions that can cause similar symptoms or findings. These conditions include:
- Corneal Ectasia: Corneal ectasia is characterized by progressive thinning and bulging of the cornea, leading to irregular astigmatism and vision distortion. While corneal ectasia primarily affects the cornea, it can sometimes be confused with anterior staphyloma, particularly when the ectasia involves the limbus. Corneal topography is essential for distinguishing between these conditions.
- Scleral Ectasia: Scleral ectasia involves thinning and outward bulging of the sclera, similar to staphyloma. However, scleral ectasia does not involve uveal tissue protrusion. The distinction between these two conditions is important, as they have different management and prognostic implications. Imaging studies such as UBM and OCT can help differentiate scleral ectasia from scleral staphyloma.
- Orbital Masses: Tumors or masses within the orbit can cause outward displacement of the eye and may mimic the appearance of a staphyloma. Imaging studies such as MRI or CT scans are crucial for identifying and characterizing orbital masses and differentiating them from scleral staphyloma.
Scleral Staphyloma Management
Managing scleral staphyloma requires a multifaceted approach that depends on the severity of the condition, its underlying cause, and the presence of associated complications. The primary goals of management are to stabilize the scleral thinning, prevent further progression, address any associated visual impairment, and reduce the risk of complications such as retinal detachment or globe rupture. Treatment strategies may include conservative management, medical therapy, and surgical intervention, tailored to the individual needs of the patient.
Conservative Management
For patients with mild scleral staphyloma who are asymptomatic or have minimal visual impairment, conservative management may be appropriate. This approach typically involves close monitoring and lifestyle modifications to minimize further damage to the sclera.
- Observation and Regular Monitoring: Patients with scleral staphyloma should undergo regular eye examinations to monitor the condition’s progression. This includes periodic visual acuity tests, slit-lamp biomicroscopy, and imaging studies such as OCT or B-scan ultrasonography. Regular monitoring allows for the early detection of changes in the staphyloma’s size or associated complications, enabling timely intervention if necessary.
- Protective Eyewear: To reduce the risk of trauma to the affected eye, which could exacerbate the condition, patients are often advised to wear protective eyewear, especially when engaging in activities that pose a risk of ocular injury. This is particularly important for patients with a history of trauma-related staphyloma.
- Lifestyle Modifications: Patients may be advised to avoid activities that could increase intraocular pressure, such as heavy lifting or straining. Additionally, managing systemic conditions that contribute to scleral weakening, such as inflammatory or autoimmune diseases, is crucial in preventing further progression of the staphyloma.
Medical Management
Medical management focuses on treating the underlying conditions that contribute to scleral thinning and staphyloma formation. This may involve the use of medications to control inflammation, reduce intraocular pressure, and manage associated ocular conditions.
- Anti-Inflammatory Medications: For patients with staphyloma associated with chronic inflammatory conditions like scleritis, systemic or topical corticosteroids may be prescribed to reduce inflammation and prevent further scleral damage. In cases where long-term corticosteroid use is required, immunosuppressive agents such as methotrexate or azathioprine may be used to minimize side effects.
- Intraocular Pressure Control: Elevated intraocular pressure can exacerbate scleral thinning and increase the risk of staphyloma progression. Patients with glaucoma or ocular hypertension may be treated with medications such as prostaglandin analogs, beta-blockers, or carbonic anhydrase inhibitors to lower intraocular pressure. Regular monitoring of intraocular pressure is essential to ensure that it remains within a safe range.
- Antibiotics and Antiviral Therapy: If the staphyloma is associated with an infectious cause, such as syphilitic scleritis or herpetic keratitis, appropriate antimicrobial therapy is necessary to eradicate the infection and prevent further damage to the sclera. In such cases, systemic or topical antibiotics, antivirals, or antifungals may be prescribed based on the specific pathogen involved.
Surgical Intervention
Surgical intervention may be necessary for patients with advanced scleral staphyloma, particularly when there is significant visual impairment, risk of globe rupture, or the presence of complications such as retinal detachment. Several surgical techniques are available to reinforce the sclera, repair the staphyloma, and preserve vision.
- Scleral Patch Grafting: Scleral patch grafting involves placing a graft, typically harvested from donor sclera or made from synthetic material, over the area of thinning to reinforce the scleral wall and prevent further bulging. This procedure is commonly used for anterior or intercalary staphylomas. The graft is sutured into place and covered with conjunctiva to promote healing and reduce the risk of infection.
- Scleral Buckling: Scleral buckling is a surgical procedure used primarily in the management of posterior staphylomas, particularly when they are associated with retinal detachment. The procedure involves placing a silicone band around the eyeball’s equator to indent the sclera and reduce the traction on the retina. This technique can help reattach the retina and prevent further detachment, preserving vision.
- Vitrectomy and Retinal Reattachment Surgery: In cases where the staphyloma has led to retinal detachment, vitrectomy may be performed to remove the vitreous gel that is exerting traction on the retina. This is often followed by retinal reattachment surgery, which may include the use of gas or silicone oil to hold the retina in place while it heals. These procedures are critical in preventing permanent vision loss.
- Corneal Transplantation: For patients with anterior staphyloma involving the cornea, corneal transplantation (keratoplasty) may be necessary if the cornea has become severely thinned or scarred. This procedure involves replacing the damaged cornea with donor tissue to restore the eye’s structural integrity and improve vision.
Post-Surgical Care and Rehabilitation
Following surgical intervention, patients require careful post-operative care to ensure proper healing and prevent complications. This may include the use of antibiotics, anti-inflammatory medications, and close follow-up with an ophthalmologist. Additionally, visual rehabilitation may be necessary for patients with significant vision loss. This can involve the use of corrective lenses, contact lenses, or low vision aids to optimize remaining vision and improve the quality of life.
In summary, the management of scleral staphyloma is tailored to the individual patient’s needs and may involve a combination of conservative, medical, and surgical approaches. Early diagnosis and appropriate intervention are essential to prevent serious complications and preserve ocular health.
Trusted Resources and Support
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski: This comprehensive resource offers in-depth coverage of various ocular conditions, including scleral staphyloma. It is widely used by ophthalmologists and medical students for understanding the diagnosis and management of eye diseases.
- “Ocular Surgery: Scleral and Corneal Techniques” by David J. Apple: This book provides detailed guidance on surgical procedures for managing scleral and corneal conditions, including scleral staphyloma. It is an excellent resource for eye surgeons seeking advanced knowledge of ocular surgical techniques.
Organizations
- American Academy of Ophthalmology (AAO): The AAO is a leading organization providing extensive resources, clinical guidelines, and educational materials for the diagnosis and treatment of ocular conditions, including scleral staphyloma. The AAO website is a valuable resource for both healthcare professionals and patients.
- National Eye Institute (NEI): As part of the National Institutes of Health (NIH), the NEI offers comprehensive information on eye diseases and supports research aimed at improving the understanding and treatment of conditions like scleral staphyloma. The NEI website provides resources for patients, clinicians, and researchers.
- American Society of Cataract and Refractive Surgery (ASCRS): The ASCRS provides resources and support for ophthalmologists specializing in cataract and refractive surgery, including techniques for managing scleral and corneal conditions. The organization offers educational materials, surgical guidelines, and research updates.