If you’ve ever wished there were a way to produce more of your own natural tears—without the constant cycle of eye drops—TrueTear may be the solution you’re looking for. This handheld neurostimulation device taps into your body’s innate tear-producing mechanisms, targeting the nerves that help lubricate the eyes naturally. Rather than masking discomfort with topical agents, TrueTear addresses the root cause of dryness for many people: insufficient or unbalanced tear production. Below, we explore how neurostimulation devices like TrueTear work, what to expect from daily usage, and the latest evidence behind their growing popularity among eye care professionals and patients alike.
A Closer Look at TrueTear and Its Science-Backed Approach
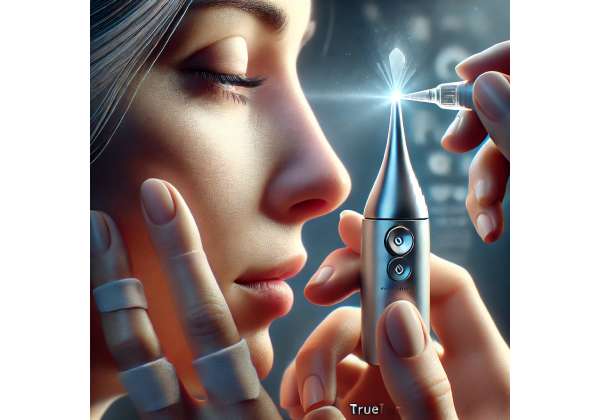
TrueTear is a small, battery-powered device designed to stimulate the lacrimal functional unit (LFU)—the interconnected glands and nerves that regulate tear secretion. By inserting a disposable tip into the nasal passage, the device delivers gentle electrical pulses to branches of the trigeminal nerve, prompting increased tear flow. This approach stands in stark contrast to artificial tears or ointments, which provide surface lubrication but do not necessarily help the eye achieve healthier, more consistent tear production on its own.
How Neurostimulation Became a New Frontier
Neurostimulation devices have been around for decades in various forms of therapy, from spinal cord stimulation for chronic pain to vagus nerve stimulation for epilepsy. Eye care specialists took notice when research confirmed that the trigeminal nerve supplies key signals to the lacrimal glands and meibomian glands. If these nerves aren’t activated sufficiently—whether due to aging, medication side effects, or other systemic factors—tear production suffers.
Dry Eye Disease (DED) occurs when your eyes can’t produce enough tears or the right kind of tears to keep the ocular surface moisturized. Traditional treatments often revolve around artificial lubrication or anti-inflammatory drops, which can help but do not directly address nerve-driven tear secretion. That’s why neurostimulation caught on: it offers a way to tap into the body’s own natural tear-producing ability.
Understanding the TrueTear Device
TrueTear is handheld, roughly the size of an electric toothbrush, with a slender, disposable tip that fits comfortably inside the nostril. A control panel allows you to adjust the intensity of the electrical pulses. Most people describe the sensation as a mild tingling or tickling, which they quickly adapt to.
Key features include:
- Disposable Nasal Tips: For hygiene and effectiveness, each tip is intended for single-day use or a designated number of uses. These tips ensure the pulses are delivered precisely.
- Customizable Intensity Levels: Not everyone’s trigeminal nerve responds the same way. TrueTear allows for variation in pulse strength so you can find the setting that best promotes tear production without causing significant discomfort.
- Built-In Safety Measures: The device automatically shuts off if it detects malfunctions or if it’s used longer than recommended. These safety checks help prevent overstimulation and preserve device integrity.
Why Trigeminal Stimulation Works for Tear Production
The nerves inside your nose are part of the ophthalmic branch of the trigeminal nerve, which not only helps with sensation but also ties into reflex loops that govern tear output. When you smell something pungent like onions, for instance, your tears often ramp up. TrueTear’s approach is essentially harnessing that reflex—minus the unpleasant odor—to coax the lacrimal glands and meibomian glands into delivering a healthier tear film.
The tear film itself has three layers—aqueous, lipid, and mucin—and each must be balanced for optimal eye comfort. By stimulating the nerves, TrueTear can encourage both watery (aqueous) tear production and meibomian gland secretions, potentially improving tear quality as well as quantity.
Clinical Rationale for Neurostimulation
For many patients, the concept of using an electrical device in the nostril to reduce eye dryness may seem unusual at first. However, the scientific underpinnings are solid. Dry eye often stems from a breakdown in the lacrimal functional unit, which includes the cornea, conjunctiva, meibomian glands, and sensory nerves that trigger tear production. If nerves aren’t firing correctly or if certain feedback loops are dulled, the eyes don’t receive the command to produce enough tears—resulting in dryness, irritation, and vision fluctuations.
This approach stands out because it:
- Targets root causes rather than merely applying surface solutions.
- Offers a drug-free alternative, which can be especially beneficial for those sensitive to preservatives or who’ve experienced side effects from topical drops.
- Enables real-time control: By adjusting intensity settings, patients can fine-tune tear stimulation to their immediate comfort level.
The Big Picture: A Shift in Dry Eye Management
Overall, TrueTear and similar devices mark a turning point in how ophthalmologists approach Dry Eye Disease. While eye drops and ointments remain helpful in many circumstances, particularly for immediate relief, neurostimulation paves the way for a more active, internally driven process. Combining TrueTear with dietary adjustments, hydration, blinking exercises, and other interventions can yield a more robust, sustainable tear film. For patients eager to reduce their reliance on artificial tears—or for whom traditional therapies haven’t been fully effective—neurostimulation stands as a compelling, science-backed option.
Integrating TrueTear into Your Daily Routine
For those ready to adopt neurostimulation as part of their dry eye management plan, it’s important to know how TrueTear fits into your day. From preparing the device to coordinating with other therapies, establishing a consistent routine can maximize benefits.
Preparing for Your First Use
Before bringing the device home, you’ll typically meet with an eye care professional who will:
- Assess Your Suitability: Certain nasal conditions (like a deviated septum or chronic sinus problems) could affect how the stimulator fits or functions. Likewise, severe cases of ocular surface disease may require a combination of therapies rather than relying on TrueTear alone.
- Demonstrate Usage: A trained technician or ophthalmologist will show you how to insert the nasal tip, position the device, and adjust the intensity settings. They’ll also offer guidelines for how frequently to use it each day or week.
Your first session often occurs in the clinic, letting you and your provider see how your eyes respond. You might be asked to rate discomfort, dryness levels, and how quickly tears start forming. This early feedback helps fine-tune your regimen from the get-go.
Step-by-Step Application
- Cleanliness and Hygiene: Always wash your hands thoroughly before handling the device or your face. This cuts down on potential infections or contamination.
- Attach a New Tip: Slide on the disposable nasal tip, ensuring it clicks into place. The tip’s shape guides its position in your nostril.
- Insert and Position: Gently place the tip into the nostril, aiming upward and slightly outward following the device’s instructions. Over time, you’ll learn the angle that yields the best tear response.
- Adjust Settings: Power on the device and begin with the lowest comfortable setting. Slowly increase if you aren’t experiencing the desired tear production. Some trial and error is normal at first.
- Monitor Duration: Sessions can last anywhere from 30 seconds to a couple of minutes, depending on how quickly your tears begin to flow. The device’s screen or app (if applicable) may guide you.
- Repeat in the Other Nostril (Optional): Many people stimulate just one nostril per session, but if dryness is severe, alternating sides is an option.
Coordinating with Eye Drops and Other Treatments
You don’t have to abandon your existing dry eye treatments once you start using TrueTear. In fact, many patients find dual or multi-modal therapy produces the best results:
- Artificial Tears: Using preservative-free drops before or after a neurostimulation session can give the ocular surface an immediate moisture boost while the device works on your underlying tear reflex.
- Warm Compresses: Softening and loosening meibomian gland secretions can further improve tear quality. Consider applying a warm compress at least once a day, especially if you have meibomian gland dysfunction.
- Anti-Inflammatory Medications: If your doctor has prescribed cyclosporine or lifitegrast drops, these can continue as normal. TrueTear addresses nerve stimulation; these drops help quell inflammation at the ocular surface.
Frequency of Use
The recommended frequency varies. Some people notice improvement with just a couple of short sessions per day; others may use TrueTear multiple times, especially during peak dryness (for instance, in the morning upon waking or after prolonged screen time). Because each disposable tip can handle several sessions within a defined time frame (check the packaging for exact guidelines), you can space out your uses while maintaining device hygiene.
Maintenance and Troubleshooting
- Battery Care: TrueTear devices usually have rechargeable batteries. Keep track of the charge level to ensure the device is ready when you need it.
- Replacing Tips: Follow manufacturer guidance on how frequently to replace the nasal tips. Some are single-use daily; others can be used multiple times in a single day but should be discarded thereafter.
- Common Issues: If you sense minimal stimulation or see a decreased tear response over time, it might be due to improper tip placement, depleted battery power, or nasal congestion. Re-evaluating your technique or contacting your eye care provider can resolve most issues.
Making It Part of Your Lifestyle
The key to success is consistency. TrueTear works best when integrated seamlessly into your daily routine, much like brushing your teeth or cleaning contact lenses. Over time, you’ll likely develop a sense of how frequently you need the device to keep dryness at bay. Many users find it more convenient than frequently reaching for artificial tears, as the added benefit is the production of natural, more balanced tears.
Ultimately, your doctor’s insights are crucial in determining when and how to use neurostimulation devices. With their guidance, you can discover a routine that delivers sustained relief—minus the hassle and potential side effects associated with around-the-clock eye drops.
Recent Findings: Clinical Evidence for TrueTear
Although neurostimulation for dry eye disease is a relatively new concept, research is mounting to confirm its safety and efficacy. Below, we delve into pivotal clinical trials, observational studies, and real-world insights that shine a light on how TrueTear fits into the broader landscape of dry eye management.
Initial Clinical Trials and FDA Approval
- Ophthalmology & Therapy (2017): In one of the early randomized controlled trials, researchers evaluated the effects of TrueTear in patients with moderate to severe Dry Eye Disease. Participants were randomly assigned to either TrueTear usage or a sham device. Over a period of four weeks, those using TrueTear experienced a statistically significant improvement in tear production, measured by the Schirmer test, as well as subjective relief in dryness and irritation.
- FDA Clearance: Soon after these findings, TrueTear received clearance in the United States for increasing tear production in adult patients with Dry Eye Disease. This official nod signified that the device met certain safety and efficacy benchmarks.
Long-Term Observational Research
- Clinical Ophthalmology (2019): A follow-up study tracked 50 individuals over six months. Most participants used TrueTear at least once daily and reported sustained tear production benefits. Researchers noted that corneal staining (a measure of dryness and ocular surface damage) was significantly reduced in the TrueTear group compared to baseline levels.
- Post-Marketing Surveillance: Multiple clinics contributed data on how patient compliance correlated with outcomes. Observations suggested that users who consistently applied TrueTear—even if just once or twice a day—maintained healthier tear films and needed fewer artificial tear applications.
Comparative Studies Against Conventional Therapies
- TrueTear vs. Artificial Tears: A small pilot study in Eye & Contact Lens (2020) pitted TrueTear usage against frequent instillation of preservative-free artificial tears. While both groups experienced symptom relief, the neurostimulation cohort exhibited better stabilization of the tear film over time and fewer episodes of ocular discomfort during screen use.
- Combining TrueTear with Prescription Drops: Another trial, published in Cornea (2021), looked at individuals already on cyclosporine drops. They added daily TrueTear sessions for half the participants, while the control group remained on cyclosporine alone. At three months, the combination group scored higher on patient-reported comfort and had reduced tear osmolarity—a sign of better tear quality.
Biological Markers of Success
More recent investigations are focusing on the biochemical and structural changes that TrueTear may induce:
- Inflammatory Markers: Studies measuring cytokines in tear fluid (like interleukin-6 and interleukin-1) found decreased levels in some users after several weeks of regular neurostimulation, hinting at broader anti-inflammatory effects beyond just mechanical tear flow.
- Meibography: By visualizing meibomian glands via imaging techniques, researchers have observed potential improvements in gland expressibility among those using TrueTear consistently. While the glands themselves may not regrow if lost, better function in existing glands can yield a healthier lipid layer in the tear film.
Real-World Case Reports
- Contact Lens Wearers: Eye doctors have shared anecdotal success stories about contact lens users who struggle with dryness. TrueTear helped maintain a better tear film, allowing longer and more comfortable lens wear.
- Post-Menopausal Women: Hormonal changes can drastically affect tear production. Some case reports highlight that older women found a noticeable improvement with daily TrueTear sessions, reducing the need for nighttime ointments.
Patient Satisfaction Trends
Beyond objective clinical measurements, patient experience remains paramount. Surveys referenced in various ophthalmic meetings (e.g., the American Academy of Ophthalmology) often indicate:
- High Ease of Use: The device’s simple design requires minimal training, although a short adjustment period is common.
- Quick Relief: Many users say they feel a shift in their eyes’ moisture within seconds or minutes, describing it as a more “natural” lubrication compared to drops.
- Motivation to Continue: Because patients can literally feel tears welling up, they’re motivated to stick with the device long term, leading to better overall compliance.
Remaining Questions and Ongoing Research
While the consensus around TrueTear’s value is generally positive, researchers continue to probe:
- Optimal Frequency: Is there a sweet spot for usage—say once a day or multiple sessions? This likely varies based on the severity of dryness and each patient’s unique physiology.
- Cost-Effectiveness: With ongoing expenses for disposable tips, is this approach more or less cost-effective compared to using multiple prescription drops or advanced procedures?
- Combination Therapies: Which pairings—like intense pulsed light (IPL) plus TrueTear, or LipiFlow with neurostimulation—yield the most dramatic, lasting improvements?
Overall, the clinical data suggests that TrueTear can offer measurable improvements in both tear volume and ocular comfort. While it won’t replace every other intervention for Dry Eye Disease, it stands out as a novel addition, especially for patients seeking a safe, technologically advanced, and drug-free therapy.
Evaluating Success Rates and Potential Risks
TrueTear’s appeal lies in its ability to kickstart natural tear production, but like any medical therapy, outcomes can vary. In clinical trials, a majority of participants report better lubrication, reduced dryness, and an overall improvement in eye comfort. Some experience this benefit almost immediately, whereas others note a steady increase in tear production over several weeks of consistent use.
From a safety standpoint, TrueTear has proven to be well-tolerated. The most common side effects include:
- Mild Discomfort: A tingling sensation or minor irritation at the electrode site in the nostril. Adjusting the intensity can often alleviate this.
- Nasal Congestion or Runny Nose: Temporary sinus stimulation can cause mild congestion, particularly if you’re already prone to allergies.
- Device-Related Issues: Very rarely, device malfunctions or improper tip placement might lead to localized discomfort. Following manufacturer guidelines significantly reduces this risk.
Patients with serious nasal abnormalities or chronic sinusitis may need additional assessments to ensure correct device positioning and to avoid exacerbating sinus-related issues. For most users, however, TrueTear represents a low-risk option that fits easily into a well-rounded dry eye regimen.
Breaking Down Treatment Costs
A new TrueTear device kit generally ranges from \$300 to \$500, with replacement nasal tips adding to the ongoing expense. Depending on insurance or regional health coverage, some costs may be partially reimbursed. Many practices offer bundled pricing or subscription plans for tip replacements, helping patients manage expenses more predictably.
Disclaimer: This article is intended for informational purposes only and is not a substitute for professional medical advice. Always consult a qualified eye care professional before starting any new treatment.
If you found these insights helpful, feel free to share on social media platforms like Facebook or X (formerly Twitter). You may help someone discover a fresh approach to soothing their eyes and reclaiming comfort in daily life.










