What is Conjunctivitis?
Conjunctivitis, also known as pink eye, is an inflammation or infection of the conjunctiva, the clear membrane that lines your eyelid and protects the white part of your eyeball. When small blood vessels in the conjunctiva become inflamed, they become more visible, giving the whites of your eyes a reddish or pink appearance. Conjunctivitis is a common and typically minor eye infection, but because it is highly contagious, early detection and treatment are critical to preventing its spread. Understanding its causes, symptoms, and prevention can help you manage the condition more effectively and reduce the risk of transmission.
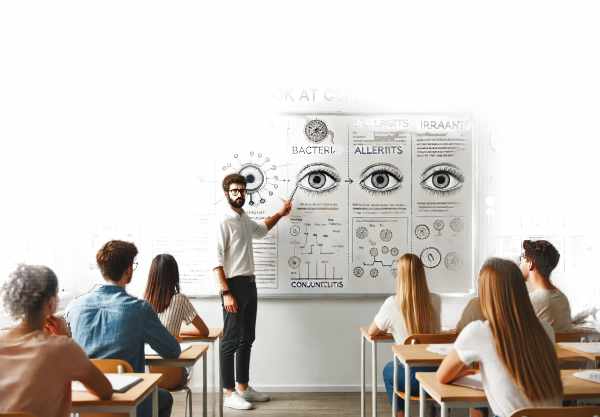
In-depth Look at Conjunctivitis
Conjunctivitis can be caused by a number of factors, including viruses, bacteria, allergens, and irritants. Each cause has its own set of characteristics, and understanding them can help you recognize and manage the condition better.
Viral conjunctivitis
The most common type is viral conjunctivitis, which is typically caused by adenoviruses. It is highly contagious and can be transmitted via direct or indirect contact with an infected person’s eye secretions. Symptoms usually include redness, watery discharge, and itching. Unlike bacterial conjunctivitis, viral conjunctivitis does not result in thick pus. Instead, the discharge is typically watery or mucoid. This type of conjunctivitis is often associated with a cold or upper respiratory infection.
The incubation period for viral conjunctivitis typically ranges from 12 hours to three days. The condition can last one to two weeks and affect either one or both eyes. During this time, patients may experience photophobia (sensitivity to light) and a gritty sensation in their eyes. Antibiotics are ineffective against viruses, so the treatment is primarily supportive. Cool compresses, artificial tears, and good hygiene can all help relieve symptoms and prevent infection from spreading.
Bacterial conjunctivitis
Bacterial conjunctivitis is caused by bacteria like Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae. This type is also contagious and can be transmitted through direct contact with infected secretions or contaminated objects. Bacterial conjunctivitis usually produces a thick, yellow-green discharge that can cause the eyelids to stick together, especially after sleeping.
Symptoms include redness, swelling, and discomfort in the affected eye. Unlike viral conjunctivitis, bacterial infections usually affect only one eye, but they can spread to the other. The condition usually goes away within a few days to a week with proper antibiotic treatment. Topical antibiotics, such as eye drops or ointments, are frequently prescribed to shorten the duration of symptoms and avoid complications.
Allergic conjunctivitis
Allergic conjunctivitis develops when the eyes are exposed to allergens like pollen, dust mites, or pet dander. This type is not contagious and is frequently linked to other allergic conditions like hay fever, asthma, and eczema. The symptoms include redness, itching, tearing, and swollen eyelids. In most cases, both eyes are affected simultaneously.
Seasonal allergic conjunctivitis is common during periods of high pollen counts. Perennial allergic conjunctivitis, on the other hand, can develop year-round due to constant exposure to allergens such as dust mites or pet dander. Treatment consists of avoiding known allergens and using antihistamines or anti-inflammatory eye drops to relieve symptoms. In severe cases, corticosteroid eye drops may be recommended.
Irritating conjunctivitis
Irritant conjunctivitis is caused by exposure to irritants such as smoke, chemicals, or foreign bodies in the eye. This type is also not contagious. Like other types of conjunctivitis, symptoms include redness, watering, and discomfort. The severity of symptoms is determined by the type and duration of exposure to the irritant.
Common irritants include chlorine from swimming pools, air pollution, and chemical fumes. The primary steps in treating irritant conjunctivitis are to flush the eyes with water and avoid further exposure to the irritant. Protective eyewear can help prevent exposure to harmful substances, lowering the risk of developing this condition.
Other causes of conjunctivitis
In addition to the primary causes listed above, conjunctivitis can be caused by less common factors such as autoimmune diseases, certain medications, and systemic infections. For example, conjunctivitis can be a symptom of systemic diseases such as rheumatoid arthritis or lupus. Certain glaucoma eye drops and dry eye medications can cause conjunctivitis.
Conjunctivitis in newborns can be caused by a blocked tear duct or an infection acquired during delivery. This condition, also known as neonatal conjunctivitis or ophthalmia neonatorum, requires immediate medical attention to avoid serious complications. It can be caused by bacteria like Neisseria gonorrhoeae or Chlamydia trachomatis, which require specific antibiotics.
Complications of Conjunctivitis
While conjunctivitis is typically a minor condition, complications can occur, particularly if the underlying cause is not properly addressed. Possible complications include:
- Keratitis: A corneal infection that, if left untreated, can cause vision impairment.
- Chronic Conjunctivitis: An ongoing inflammation that may necessitate long-term treatment.
- Scarring: In severe cases, particularly with certain bacterial or viral infections, the conjunctiva may scar, affecting vision.
- Secondary Infections: If not treated properly, bacterial conjunctivitis can cause secondary infections.
Conjunctivitis in Special Populations
Certain populations are more prone to conjunctivitis and may exhibit different symptoms or complications. Individuals with weakened immune systems, such as those living with HIV/AIDS or undergoing chemotherapy, may experience more severe or prolonged infections. In such cases, conjunctivitis may coexist with other opportunistic infections, necessitating a tailored treatment strategy.
Children are especially susceptible to conjunctivitis due to their close contact with peers in settings such as schools and daycare centers. Due to the high contagion rate among children, strict hygiene practices are required to prevent outbreaks.
Elderly people may also be more vulnerable to conjunctivitis due to age-related immune system changes and the use of medications that can impair eye health. They may recover more slowly and are more likely to develop complications, emphasizing the importance of receiving prompt and appropriate treatment.
How to Avoid Conjunctivitis
- Practice Proper Hygiene: Wash your hands often with soap and water, especially before touching your face or eyes. If soap and water are not available, use hand sanitizer instead.
- Avoid Touching Your Eyes: To prevent the spread of infection, do not rub or touch your eyes with unwashed hands.
- Use Clean Towels and Bedding: To reduce the risk of spreading conjunctivitis, keep towels, washcloths, and pillowcases clean and do not share them with others.
- Dispose of Contaminated Items: Remove any disposable items that come into contact with your eyes, such as tissues, cotton balls, and makeup applicators.
- Disinfect Surfaces: To reduce the spread of germs, regularly clean and disinfect frequently touched surfaces such as doorknobs, light switches, and countertops.
- Don’t Share Personal Items: Don’t share personal items like eye makeup, contact lenses, or sunglasses with others.
- Wear Protective Eyewear: When working in environments where irritants or allergens may be present, wear protective goggles or glasses.
- Managing Allergies Effectively: If you have allergies, control your symptoms and avoid known allergens to reduce your risk of allergic conjunctivitis.
- Practice Proper Contact Lens Hygiene: Clean and store contact lenses as directed, and do not wear them overnight unless specifically advised by your eye care professional.
- Seek prompt medical attention. If you have symptoms of conjunctivitis, seek medical attention right away to receive proper treatment and avoid complications.
Conjunctivitis Diagnostic Techniques
Conjunctivitis is diagnosed by conducting a thorough examination of the patient’s medical history and symptoms. The first step is usually a thorough examination of the eye with a slit lamp, which allows the healthcare provider to see the conjunctiva, cornea, and other structures under high magnification and bright lighting. This examination helps to determine the type of conjunctivitis based on the appearance of the eye and the nature of the discharge.
The diagnosis of viral conjunctivitis is primarily clinical, with a characteristic watery discharge and the presence of systemic viral symptoms such as a cold or sore throat. Additional testing, such as viral cultures or polymerase chain reaction (PCR) tests, can be performed in some cases to identify the specific virus responsible for the infection, but these tests are rarely used in routine practice due to cost and time constraints.
Bacterial conjunctivitis is diagnosed using a similar clinical evaluation. If the condition is severe or does not respond to initial treatment, a sample of the eye discharge can be collected and sent to a laboratory for Gram staining and bacterial culture. This aids in identifying the causative bacteria and determining the best antibiotic treatment.
Allergic conjunctivitis is usually diagnosed based on a patient’s allergy history and the presence of bilateral eye symptoms like itching, redness, and tearing. Patients with recurring or severe allergic conjunctivitis may benefit from allergy testing, such as skin prick tests or blood tests to identify specific allergens.
Irritant conjunctivitis is diagnosed based on a detailed history of exposure to potential irritants such as chemicals or pollutants. The diagnosis is confirmed after the irritant is removed and the symptoms have resolved.
In recent years, new diagnostic techniques for adenovirus, such as point-of-care testing, have emerged. These rapid tests can produce results in minutes, assisting in the differentiation of viral and bacterial conjunctivitis and directing appropriate treatment. Furthermore, advanced imaging techniques such as in vivo confocal microscopy and optical coherence tomography (OCT) are being investigated for their ability to provide detailed insights into the conjunctival tissue while improving diagnostic accuracy.
Effective Conjunctivitis Treatments
Conjunctivitis is treated based on the underlying cause. For viral conjunctivitis, supportive care is the primary treatment option. This includes applying cool compresses to relieve discomfort and artificial tears to alleviate dryness. Because antibiotics are ineffective against viruses, antiviral medications are rarely prescribed. However, in cases of herpes simplex virus conjunctivitis, antiviral eye drops or oral medications may be required.
Bacterial conjunctivitis is managed with antibiotic eye drops or ointments. Erythromycin, tobramycin, and fluoroquinolones are among the most commonly prescribed antibiotics. The antibiotic used is determined by the severity of the infection as well as the results of any bacterial cultures. Even if symptoms improve, completing the entire course of antibiotics is critical to ensuring the infection is completely eradicated.
To treat allergic conjunctivitis, avoid known allergens and use antihistamine or anti-inflammatory eye drops to control symptoms. Over-the-counter antihistamine eye drops, such as ketotifen, can alleviate itching and inflammation. In more severe cases, prescription-strength antihistamines or corticosteroid eye drops may be required. Mast cell stabilizers, such as olopatadine, can also help to prevent the release of histamine and other inflammatory mediators.
Irritant conjunctivitis is treated by removing the source of irritation and flushing the eyes with saline or water to eliminate any remaining irritants. Artificial tears can soothe the eyes and provide extra comfort. In cases of chemical exposure, immediate irrigation with copious amounts of water is critical, and medical attention should be sought right away.
For severe allergic conjunctivitis, immunomodulatory agents and biologics are among the innovative and emerging therapies. These therapies are intended to modulate the immune response and reduce inflammation more effectively than traditional treatments. Furthermore, research into antiviral agents that target specific viral proteins is ongoing, with the goal of developing more targeted and effective treatments for viral conjunctivitis in the future.
Trusted Resources
Books
- Ophthalmology by Myron Yanoff and Jay S. Duker
- Kanski’s Clinical Ophthalmology: A Systematic Approach by Brad Bowling
- The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease by Adam T. Gerstenblith and Michael P. Rabinowitz










