Introduction to Episcleritis
Episcleritis is an inflammatory condition that affects the episclera, which is a thin layer of tissue located between the conjunctiva and the sclera. It is usually a harmless, self-limiting condition marked by redness, mild discomfort, and no discharge. Episcleritis can affect one or both eyes and is more common in younger and middle-aged adults. While it is not usually associated with severe complications, understanding the causes, symptoms, and diagnostic methods is critical for proper management and distinguishing it from more serious ocular conditions.
Comprehensive Investigation of Episcleritis
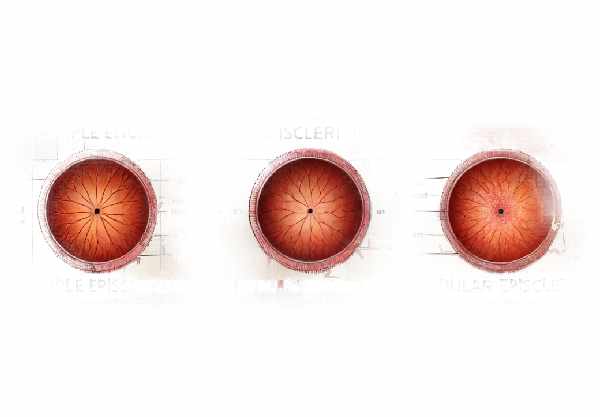
Episcleritis is divided into two types: simple and nodular episcleritis. Each type has distinct clinical characteristics and different implications for the affected individual.
Simple Episcleritis
The most common type is simple episcleritis, which is characterized by mild inflammation that occurs intermittently. Simple episcleritis causes redness that is typically sectoral, meaning it affects a specific area of the eye, though it can be diffuse at times. Symptoms typically include mild discomfort, irritation, and tenderness. Simple episcleritis episodes usually resolve spontaneously within one to two weeks, though recurrences are common.
Nodular Episcleritis
Nodular episcleritis is less common, but it can last longer and be more severe than simple episcleritis. This type appears as a localized, raised area (nodule) on the episclera that is often tender to the touch. The inflammation in nodular episcleritis can be more severe and last for several weeks. Despite the more severe symptoms, nodular episcleritis, like its simple counterpart, is usually self-limiting and does not cause significant ocular damage.
Causes and Risk Factors
The exact cause of episcleritis is frequently unknown, but it is thought to be linked to a variety of underlying conditions and environmental factors. This includes:
- Autoimmune Disorders: Episcleritis has been linked to systemic autoimmune diseases including rheumatoid arthritis, lupus, and inflammatory bowel disease. In these cases, the immune system mistakenly targets its own tissues, such as the episclera.
- Infections: Although rare, episcleritis can be caused by bacterial, viral, or fungal pathogens. Episcleritis can be caused by infections such as the herpes simplex virus or Lyme disease.
- Allergic Reactions: Environmental factors such as pollen, dust, or pet dander can trigger episcleritis.
- Stress and Hormonal Changes: Some evidence suggests that stress and hormonal fluctuations, particularly in women, may contribute to the development of episcleritis.
- Idiopathic: Episcleritis that occurs without a known cause is classified as idiopathic episcleritis. This type is usually mild and resolves on its own.
Symptoms
The symptoms of episcleritis vary according to the type and severity of the inflammation. Common symptoms include:
- Redness: The most common symptom of episcleritis is redness of the eye, which can be localized or diffuse.
- Mild Pain or Discomfort: Unlike scleritis, which can be excruciatingly painful, episcleritis usually causes only minor discomfort or tenderness.
- Irritation or Burning Sensation: Patients may notice a gritty or burning sensation in their affected eye.
- Light Sensitivity: Photophobia, or sensitivity to light, may occur but is usually mild.
- Watery Eyes: Increased tear production is common, but there is usually no discharge or mucus.
Differential Diagnosis
Differentiating episcleritis from other ocular conditions is critical for effective treatment. Conditions that may resemble episcleritis include:
- Scleritis: A more severe inflammation of the deeper scleral tissues that is frequently associated with significant pain and vision loss.
- Conjunctivitis: Also known as pink eye, conjunctivitis is an inflammation of the conjunctiva that is typically accompanied by discharge and itching.
- Keratitis: An inflammation of the cornea that can cause redness, pain, and vision changes.
Effects on Quality of Life
Although episcleritis is typically not sight-threatening, the symptoms can be bothersome and interfere with daily activities. The redness and discomfort may cause cosmetic issues and minor visual disturbances. Recurrent episodes can be especially frustrating for patients, causing anxiety and a lower quality of life.
Epidemiology
Episcleritis can develop at any age, but it is most common in young and middle-aged adults. Women are slightly more affected than men, perhaps due to hormonal influences. The condition is generally self-limiting, but the frequency and severity of episodes vary greatly between individuals.
Complications
Complications from episcleritis are uncommon, but they do occur, particularly if the underlying cause is a systemic disease. Possible complications include:
- Recurrent Episodes: Frequent recurrences can cause ongoing discomfort and frustration.
- Progression to Scleritis: Episcleritis can sometimes progress to scleritis, which is a more severe and potentially sight-threatening condition.
- Association with Systemic Disease: Episcleritis may be a sign of an underlying systemic condition that necessitates medical intervention.
Patient Education and Support
Educating patients about episcleritis is critical for effective treatment. Patients should be educated on the symptoms, potential triggers, and the importance of seeking medical attention if they have recurring or severe episodes. Support groups and resources can help patients deal with the emotional and practical aspects of living with episcleritis.
Episcleritis: Diagnostic Techniques
Episcleritis is diagnosed through a combination of clinical evaluation, patient history, and specific diagnostic tests that confirm the condition and rule out other causes of ocular redness and inflammation.
Clinical Examination
A thorough clinical examination by an ophthalmologist is required to diagnose episcleritis. This includes:
- Visual Inspection: The ophthalmologist will check the eye for redness, swelling, and visible nodules on the episclera.
- Slit-Lamp Examination: A slit-lamp microscope provides a detailed view of the eye’s anterior segment, allowing the ophthalmologist to determine the extent and location of inflammation. This examination helps to distinguish episcleritis from other conditions such as scleritis or conjunctivitis.
Patient History
Obtaining a complete patient history is critical for determining potential underlying causes and risk factors. The ophthalmologist will ask about:
- Duration and Onset of Symptoms: Understanding when symptoms first appeared and how they progressed can shed light on the nature of the condition.
- Previous Episodes: Knowing about previous cases of episcleritis can help determine whether the condition is recurring.
- Systemic Diseases: A history of autoimmune diseases, infections, or allergies may suggest a link to episcleritis.
- Medications: Because certain medications can cause or worsen inflammation, it is critical to have a thorough medical history.
Diagnostic Tests
Several diagnostic tests can be used to confirm episcleritis and rule out other conditions.
- Phenylephrine Test: Phenylephrine eye drops can be used to whiten the episcleral vessels. The redness in episcleritis usually goes away with phenylephrine, but not in scleritis. This test distinguishes between episcleritis and scleritis.
- Fluorescein Staining: Applying fluorescein dye to the eye can aid in determining any corneal involvement or defects that may indicate a different diagnosis.
- Ultrasound Biomicroscopy (UBM): High-frequency ultrasound is used to create detailed images of the eye’s anterior segment, which provides additional information about the depth and extent of inflammation.
Lab Tests
When an underlying systemic condition is suspected, laboratory tests may be required.
- Blood Tests: Tests for inflammation markers (e.g., ESR, CRP) and specific autoimmune markers (e.g., ANA, RF) can aid in the diagnosis of associated systemic diseases.
- Infectious Disease Screening: If an infectious cause is suspected, tests for specific pathogens (such as Lyme disease or herpes simplex virus) may be performed.
Imaging Studies
Advanced imaging techniques can provide additional insights into the condition.
- Optical Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the eye, which are useful for detecting structural changes in the episclera and sclera.
- MRI or CT Scans: In rare cases, imaging studies may be required to determine the extent of inflammation and rule out other serious eye conditions.
Episcleritis Treatment Options
Episcleritis treatment aims to alleviate symptoms while also addressing any underlying conditions. Most cases of episcleritis are self-limiting and resolve without treatment, but medications and supportive care can hasten recovery and alleviate discomfort.
Standard Treatment Options
- Topical Steroid
- Mild topical corticosteroids may be prescribed to alleviate inflammation and discomfort. Prednisolone acetate and fluorometholone are two commonly used steroids. These drops are typically administered several times per day, with the dose decreasing as symptoms improve.
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- NSAIDs, whether topical or oral, can help relieve pain and inflammation. Diclofenac and ketorolac are frequently used as eye drops. Oral NSAIDs, such as ibuprofen or naproxen, may also be prescribed for severe discomfort.
- Artificial tears
- Lubricating eye drops or artificial tears can help relieve the irritation and dryness caused by episcleritis. These are sold over the counter and can be used as needed.
- Cold compresses
- Using cold compresses on the affected eye can help reduce redness and swelling. This simple home remedy brings relief and can be combined with other treatments.
Treatment of Underlying Conditions
If episcleritis is linked to an underlying systemic condition like rheumatoid arthritis or lupus, treating the primary disease is critical. This may involve:
- Agents that suppress immunity
- Medications like methotrexate, azathioprine, or biologics may be prescribed to treat autoimmune diseases that cause episcleritis.
- Antibiotics and antivirals
- If an infection is the source, appropriate antibiotics or antivirals will be required to combat the underlying pathogen.
Innovative and Emerging Therapies
- Biological Treatments
- Biologic drugs that target specific immune system components are being studied for their ability to treat autoimmune-related episcleritis. These include TNF inhibitors and other monoclonal antibodies that regulate immune responses.
- Advanced Topical Agents
- New anti-inflammatory formulations are being developed to provide more effective and long-lasting relief. These could include novel steroid-sparing agents that reduce inflammation without the side effects that come with long-term steroid use.
- targeted immunotherapy
- The goal of targeted immunotherapy research is to develop treatments that specifically target the immune mechanisms that cause episcleritis. This approach has the potential to provide more precise and effective management of the condition, particularly for those who experience chronic or recurring episodes.
Supportive Care
Providing supportive care is critical for managing symptoms and increasing patient comfort. This includes:
- Patient education
- Educating patients about the condition, its benign nature, and the importance of follow-up can help to reduce anxiety and ensure treatment adherence.
- Regular monitoring
- Regular follow-up visits to monitor the condition and adjust treatments as needed are essential, particularly for patients with underlying systemic diseases.
By combining these standard treatments with emerging therapies and supportive care, healthcare providers can provide comprehensive management strategies that are tailored to each patient.
Best Practices for Avoiding Episcleritis
- Keep Good Eye Hygiene
- Clean your eyelids and eyelashes on a regular basis to remove debris and lower the risk of infection or irritation.
- Manage stress
- Stress can trigger the onset of episcleritis. Exercise, meditation, or hobbies can all help reduce stress.
- Protect your eyes
- Wear protective eyewear when doing activities that may expose your eyes to dust, debris, or chemical irritants.
- Control Systemic Conditions
- If you have an autoimmune disease or other chronic conditions, stick to your treatment plan and schedule regular check-ups to avoid flare-ups that can lead to episcleritis.
- Avoid allergens
- Identify and avoid allergens that can cause episcleritis, such as pollen, dust, or pet dander.
- Use Artificial Tears.
- Keep your eyes lubricated with artificial tears, especially in dry or windy weather, to reduce irritation and inflammation.
- Avoid eye rubbing
- Avoid rubbing your eyes, as this can worsen inflammation and increase the risk of episcleritis.
- A Healthy Diet and Hydration
- Eat a well-balanced diet rich in antioxidants and omega-3 fatty acids, and stay hydrated to promote overall eye health.
- Quit smoking
- Smoking can increase inflammation and harm eye health. Quitting smoking can lower the risk of episcleritis and other ocular problems.
- Regular Eye Exam
- Schedule regular eye exams to catch any early signs of episcleritis and treat them promptly.
Trusted Resources
Books
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Adam T. Gerstenblith and Laura J. Wayne
- “Ocular Disease: Mechanisms and Management” by Leonard A. Levin, James Ver Hoeve, Samuel Wu, Paul L. Kaufman, and Albert Alm
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
Online Resources
- American Academy of Ophthalmology
- National Eye Institute
- Mayo Clinic – Episcleritis
- WebMD – Episcleritis