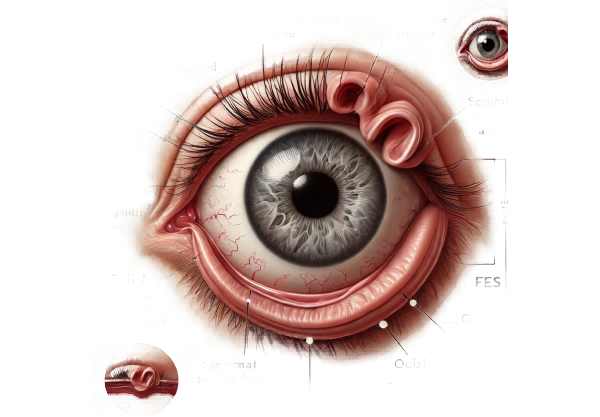
What is Floppy Eyelids Syndrome?
Floppy Eyelid Syndrome (FES) is an ocular condition characterized by upper eyelid laxity and floppiness, which allows them to be easily everted (turned inside out). This condition frequently causes chronic eye irritation, discomfort, and redness due to the constant exposure of the inner eyelid and ocular surface. FES is commonly found in obese middle-aged men and is frequently associated with obstructive sleep apnea (OSA). The exact cause is unknown, but it is thought to be due to mechanical and inflammatory factors affecting the eyelid tissues.
Clinical Presentation of Floppy Eyelid Syndrome
Floppy Eyelid Syndrome (FES) is a complex, multifactorial condition that affects the eyelids, causing significant discomfort and potentially damaging the ocular surface. This syndrome is frequently underdiagnosed due to its subtle and varied presentation.
Epidemiology and Demographics
FES is most common in obese, middle-aged men, but it can also affect women and children. The condition is frequently associated with obstructive sleep apnea (OSA), with studies indicating that up to 96% of FES patients have OSA. This strong association emphasizes the significance of identifying FES as a potential indicator of sleep-disordered breathing.
Pathophysiology
FES pathophysiology is complex, involving both mechanical and inflammatory factors. The upper eyelids become unusually lax and can be easily lifted with light pressure. This laxity is thought to be caused by the degeneration of elastic fibers and collagen in the eyelid tissues, which may be exacerbated by repetitive mechanical trauma during sleep, as patients frequently sleep with their faces pressed against a pillow.
Symptoms and Clinical Presentation
Patients with FES commonly present with a variety of ocular symptoms, including:
- Chronic Eye Irritation: Consistent discomfort and a gritty feeling in the eyes.
- Redness and Inflammation: Redness and inflammation of the conjunctiva caused by chronic exposure.
- Mucous Discharge: Increased mucous production causes a sticky discharge.
- Tearing: Excess tearing or epiphora caused by irritation.
Ptosis is the drooping of the upper eyelid. - Keratitis: Inflammation of the cornea, which can progress to more serious complications if left untreated.
Risk Factors
Several risk factors contribute to the development of FES, including:
- Obesity: A major risk factor due to increased mechanical pressure on the eyelids while sleeping.
- Obstructive Sleep Apnea: OSA and FES have a strong correlation, with many patients experiencing both conditions at the same time.
- Age and Gender: Middle-aged men are more susceptible, but the condition can affect people of any age and gender.
- Chronic Eye Rubbing: Repetitive eye rubbing can contribute to eyelid laxity and worsen symptoms.
Complications
If left untreated, FES can cause a number of complications that can impair vision and overall eye health:
- Chronic Keratoconjunctivitis: Prolonged inflammation of the cornea and conjunctiva, resulting in scarring and vision loss.
- Corneal Ulcers: Open sores on the cornea caused by chronic irritation and exposure, which can infect and impair vision.
- Scarring and Fibrosis: Chronic inflammation can cause scarring and fibrosis of the eyelids and ocular surface tissues.
- Ectropion: Outward turning of the eyelid margin, which increases exposure and irritation.
Differential Diagnosis FES must be distinguished from other conditions with similar symptoms, including:
- Blepharitis: Inflammation of the eyelid margins, frequently caused by bacterial infection or skin conditions such as rosacea.
- Conjunctivochalasis: Excess conjunctival tissue that can cause FES symptoms.
- Ectropion: Eyelid laxity caused by aging or previous trauma/surgery.
- Dry Eye Syndrome is a condition characterized by insufficient tear production or poor tear quality, which causes chronic irritation.
Pathologic Findings
Histopathological analysis of eyelid tissue in FES patients reveals significant changes, including:
- Elastin Degradation: The breakdown of elastic fibers within the tarsal plate of the eyelid.
- Collagen Abnormalities: Changes to collagen structure and composition, resulting in decreased tensile strength and increased laxity.
- Chronic Inflammation: The presence of chronic inflammatory cells in the eyelid tissues, which contribute to ongoing irritation and degradation.
Associated Conditions
The strong association between FES and obstructive sleep apnea (OSA) emphasizes the importance of a multidisciplinary approach to diagnosis and treatment. OSA is a condition characterized by repeated episodes of partial or complete upper airway obstruction during sleep, which causes sleep disruption and a variety of systemic complications such as cardiovascular disease and metabolic syndrome. Addressing OSA in FES patients can greatly improve their ocular symptoms and overall health.
Effects on Quality of Life
FES has a significant impact on a patient’s quality of life, causing chronic discomfort, visual disturbances, and cosmetic concerns. The constant irritation and need for frequent eye care can be taxing, affecting daily activities and sleep quality. In addition, the aesthetic changes caused by ptosis and mucous discharge can have an impact on self-esteem and social interactions.
Diagnostic Tools for Floppy Eyelid Syndrome
Floppy Eyelid Syndrome is diagnosed through a combination of clinical evaluation, patient history, and specialized tests that confirm the presence of eyelid laxity and associated ocular surface changes.
Clinical Examination
A thorough clinical examination by an ophthalmologist is required to diagnose FES. Key aspects of the exam include:
- Eyelid Eversion Test: Gently evert the upper eyelid to determine its laxity and ease of turning inside out. With FES, the eyelid can be easily everted with little pressure.
- Slit-Lamp Examination: A thorough examination of the ocular surface with a slit lamp to detect signs of conjunctival inflammation, keratitis, or mucous discharge.
- Assessment of Ptosis: determining the extent of upper eyelid drooping and its impact on vision.
Imaging Techniques
Advanced imaging techniques can provide more information about the structural changes in the eyelids and ocular surface.
- Anterior Segment Optical Coherence Tomography (OCT): High-resolution imaging of the eyelid and conjunctival structures, aiding in the assessment of elastin and collagen degradation.
- Meibography: Imaging of the meibomian glands to assess function and detect any abnormalities related to FES.
Sleep Studies
Given the strong link between FES and obstructive sleep apnea, a full sleep study (polysomnography) may be recommended to screen for OSA. Identifying and treating OSA can greatly improve FES symptoms and overall health.
Differential Diagnosis
Differentiating FES from other conditions with similar symptoms is critical for proper diagnosis and treatment. This may involve:
- Schirmer’s Test: Determines tear production to rule out dry eye syndrome.
- Eyelid Biopsy: In rare cases, a biopsy of the eyelid tissue may be performed to detect underlying pathological changes.
Managing Floppy Eyelid Syndrome
Treatment for Floppy Eyelid Syndrome (FES) focuses on symptom relief, preventing complications, and addressing any underlying conditions, such as obstructive sleep apnea. Here are the conventional and emerging treatment options:
- Lubricating Eye Drops and Ointments: These are frequently used as the first line of treatment to alleviate dryness and irritation. Using lubricating eye drops during the day and ointments at night can help to protect the eye surface.
- Eyelid Taping or Shields: Patients may be advised to tape their eyelids shut or wear eye shields while sleeping to keep them from turning inside out. This reduces exposure and irritation to the conjunctiva and cornea.
- Topical Steroids and Antibiotics: In cases of severe inflammation or infection, short-term use of topical steroids or antibiotics may be prescribed to reduce inflammation and treat secondary infections.
- CPAP Therapy for OSA: Because FES is frequently associated with OSA, continuous positive airway pressure (CPAP) therapy can alleviate both sleep apnea and FES symptoms by reducing mechanical stress on the eyelids while sleeping.
- Eyelid Surgery: Surgical intervention is recommended in severe cases or when conservative treatments fail. Various surgical techniques can be used:
- Lateral Tarsal Strip Procedure: Tightening the lateral canthal tendon to help support the eyelid.
- Eyelid Tightening Procedures: These include medial or lateral plications to reduce eyelid laxity.
- Blepharoplasty: The removal of excess skin and tissue from the eyelids to improve function and appearance.
Innovative and Emerging Therapies
- Biologic Agents: Researchers are investigating the use of biologic agents to target specific inflammatory pathways involved in FES. These agents could provide a more targeted approach to reducing inflammation and promoting tissue repair.
- Gene Therapy: New research on gene therapy seeks to address the underlying genetic components of FES by repairing or replacing defective genes. Although still in the experimental stages, this approach shows promise for future treatments.
- Tissue Engineering: Advances in tissue engineering and regenerative medicine are being studied to create new eyelid tissues capable of replacing damaged or lax eyelid structures.
- Minimally Invasive Procedures: Novel minimally invasive surgical techniques are being developed to shorten recovery time and improve outcomes. These include laser-based methods and advanced suturing techniques for improving eyelid stability and function.
- Neuroprotective Therapies: Investigating neuroprotective treatments to improve the health of the ocular surface and eyelid tissues, with the goal of reducing the effects of chronic inflammation and mechanical stress.
By combining traditional treatment methods with innovative approaches, FES management is becoming more comprehensive and effective, giving patients hope for a better quality of life.
Risk Reduction for Floppy Eyelid Syndrome
While Floppy Eyelid Syndrome (FES) is primarily caused by mechanical and genetic factors, there are several best practices that can help reduce the risk and manage symptoms.
- Keep a Healthy Weight: Obesity is a major risk factor for FES and OSA. Maintaining a healthy weight through diet and exercise can help lower the risk.
- Use Proper Sleep Posture: Avoid sleeping on your face or side, as this can cause pressure on your eyelids. Sleeping on your back with your head elevated may aid in reducing eyelid laxity.
- Regular Eye Exams: Early detection and treatment of FES can help prevent complications. Regular visits to an ophthalmologist are required, especially for those at higher risk.
- Treat Underlying Conditions: Using CPAP therapy to manage associated conditions such as OSA can help improve FES symptoms and prevent the condition from worsening.
- Avoid Rubbing Your Eyes: Prolonged eye rubbing can worsen eyelid laxity. Be gentle with your eyes and avoid excessive touching or rubbing.
- Use Protective Eyewear: Wearing protective eyewear while engaging in activities that may cause eye trauma can help prevent injuries that contribute to eyelid laxity.
- Maintain a Skincare Routine: Proper eyelid hygiene and skincare can reduce inflammation and irritation, thereby improving overall eyelid health.
- Stay Hydrated: Adequate hydration promotes tissue health and helps to maintain eyelid elasticity.
- Protect Against Allergens: Effectively manage allergies to prevent rubbing and irritation of the eyes, which can exacerbate FES symptoms.
Individuals who follow these practices can reduce their risk of developing FES and alleviate current symptoms.
Trusted Resources
Books
- “Eyelid Disorders: Diagnosis and Management” by Frank A. Bucci Jr.
- “Diseases and Disorders of the Orbit and Ocular Adnexa” by Aaron Fay and Peter J. Dolman
Online Resources
- American Academy of Ophthalmology: AAO
- National Eye Institute: NEI
- Mayo Clinic: Mayo Clinic
- American Sleep Apnea Association: ASAA






