What is fungal keratitis?
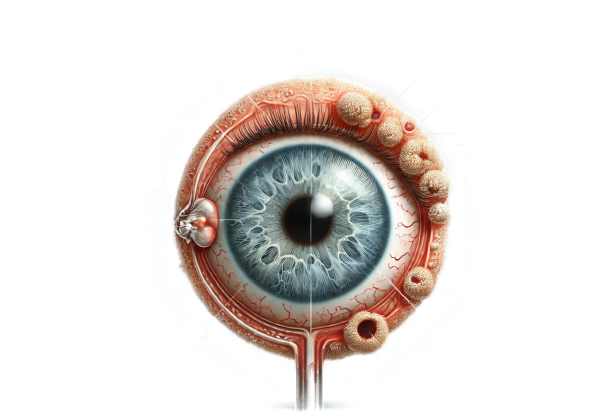
Fungal Keratitis is a severe and potentially sight-threatening cornea infection caused by fungal organisms. The cornea is a clear, dome-shaped surface that covers the front of the eye and is essential for focusing vision. Fungal infections of the cornea are uncommon, but they can occur after trauma, especially with organic matter like plant material, or in people with weakened immune systems. To avoid complications such as permanent vision loss, this condition must be diagnosed and treated as soon as possible.
Detailed Investigation of Fungal Keratitis
Fungal Keratitis is a complex ocular condition that is difficult to diagnose and manage. Understanding the etiology, risk factors, pathophysiology, clinical presentation, and complications is critical for successful treatment.
Etiology and causative organisms
Fungal Keratitis can be caused by a variety of fungi, which are broadly classified as filamentous fungi and yeasts.
- Filamentous Fungi: Fungal keratitis is most commonly caused by filamentous fungi in tropical and subtropical regions. Common species are:
- Aspergillus: Commonly found in soil and decaying vegetation.
- Fusarium: Commonly found in plant material and soil.
- Curvularia is another soil-borne fungus.
- Yeasts are more common in temperate climates and among immunocompromised patients. Common species are:
- candida: Commonly found on the skin and mucous membranes.
Pathophysiology
The pathogenesis of fungal keratitis begins with the introduction of fungal spores into the corneal tissue, which usually occurs after trauma or surgery. The fungi adhere to the corneal epithelium, invade the stroma, and produce enzymes that degrade corneal tissue, resulting in inflammation and necrosis. The immune response to the infection exacerbates tissue damage, leading to corneal ulcers.
Risk Factors
Several risk factors raise the chances of developing fungal keratitis:
- Trauma: Corneal injury, especially from organic matter like plant material, is a significant risk factor.
- Contact Lens Use: Poor hygiene, prolonged wear, and the use of contaminated solutions can all introduce fungi into the cornea.
- Ocular Surface Disease: Conditions that disrupt the integrity of the corneal epithelium, such as dry eye syndrome or chronic keratitis, make people susceptible to infection.
- Immunocompromised State: Patients with compromised immune systems, such as those with HIV/AIDS, diabetes, or receiving immunosuppressive therapy, are at a higher risk.
- Previous Ocular Surgery: Surgical procedures to the eye can introduce pathogens and jeopardize corneal integrity.
Clinical Presentation
Fungal keratitis causes a variety of symptoms, which vary in severity depending on the causative organism and the host’s immune response. Common symptoms include:
- Pain: Frequently severe and out of proportion to the clinical signs.
- Redness: Conjunctival injection causes redness in the eye.
- Discharge: A purulent or watery discharge may exist.
- Decreased Vision: Caused by corneal opacity and edema.
- Photophobia: sensitivity to light.
- Tearing refers to excessive tearing or lacrimation.
The clinical signs of fungal keratitis may include:
- Corneal Ulcer: A grayish-white infiltrate with feathery edges, more commonly found in filamentous fungi.
- Satellite Lesions: Smaller infiltrates around the primary lesion.
- Hypopyon is the accumulation of inflammatory cells in the anterior chamber.
- Corneal Thinning and Perforation: Severe cases may result in corneal thinning and perforation.
Differential Diagnosis
Fungal keratitis is distinct from other types of infectious keratitis, such as bacterial, viral, and acanthamoeba keratitis. This distinction is critical for effective treatment. Key differences include:
- Bacterial Keratitis: Typically has a faster onset and a central ulcer with a dense infiltrate.
- Viral Keratitis: This condition is frequently associated with dendritic lesions (in the case of herpes simplex virus) and a history of recurring episodes.
- Acanthamoeba Keratitis: Causes severe pain, ring infiltrates, and is frequently associated with contact lens wear.
Complications
If left untreated, fungal keratitis can cause serious complications, including:
- Corneal Scarring: Permanent scarring that may impair vision.
- Corneal Perforation: Full-thickness loss of corneal tissue, which may result in loss of vision.
- Endophthalmitis: Infection spreads to the interior of the eye, threatening vision and necessitating immediate treatment.
- Vision Loss: Significant and potentially permanent vision loss as a result of corneal and surrounding structural damage.
Epidemiology
Fungal keratitis is more common in tropical and subtropical regions due to increased risk of ocular trauma from plant material and fungi in the environment. It accounts for a large proportion of microbial keratitis cases in these areas. Fungal keratitis is less common in temperate climates, but it does occur, especially among contact lens wearers and immunocompromised patients.
Public Health Implications
Fungal keratitis is a major public health concern, particularly in developing countries where access to medical care and antifungal medications may be limited. Early diagnosis and treatment are critical for avoiding serious outcomes. Public health initiatives centered on education, prevention, and early intervention can help reduce the incidence and severity of fungal keratitis.
Recognizing the risk factors, clinical features, and potential complications of fungal keratitis is essential for understanding the condition. Early identification and differentiation from other types of keratitis are critical for initiating appropriate treatment and avoiding serious complications.
Diagnostic methods
Fungal keratitis must be diagnosed using a combination of clinical evaluation, laboratory testing, and imaging studies to confirm the presence of fungal infection and distinguish it from other types of keratitis.
Clinical Evaluation
- Patient History: A thorough history includes questions about recent trauma, particularly organic matter, contact lens use, previous ocular surgeries, and any underlying medical conditions that may predispose to fungal infections.
- Slit-Lamp Examination: A thorough examination with a slit lamp can reveal typical features of fungal keratitis, such as feathery-edged infiltrates, satellite lesions, and hypopyon.
Laboratory Testing
- Corneal Scraping and Culture: This is the most reliable method for diagnosing fungal keratitis. A corneal scraping is taken and cultured on specialized media to identify fungal organisms. Sabouraud dextrose agar is commonly used in fungal cultures.
- KOH Wet Mount: Using potassium hydroxide (KOH) to wet mount corneal scrapings can help identify fungal elements quickly. KOH dissolves the host cells, revealing the fungal hyphae or yeast cells under the microscope.
- Gram Stain and Giemsa Stain: These stains can aid in the detection of fungal organisms and other pathogens. Fungi are typically seen as branching hyphae in these preparations.
- PCR (Polymerase Chain Reaction): Molecular diagnostic techniques such as PCR can detect fungal DNA in corneal samples, providing a quick and accurate method for identifying specific fungal species.
Imaging Studies
- Confocal Microscopy: This non-invasive imaging technique produces high-resolution images of the cornea and can aid in identifying fungal hyphae within the corneal layers. It is especially useful when the diagnosis is unclear or when corneal scraping is not an option.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT can produce detailed cross-sectional images of the cornea, assisting in determining the depth and extent of the infection.
Additional Diagnostic Tools
- In Vivo Confocal Microscopy: This cutting-edge technique enables real-time imaging of the cornea, revealing detailed information about the presence and distribution of fungal elements.
- Serological Tests: Although not commonly used for initial diagnosis, serological tests can help identify systemic fungal infections that may be causing the keratitis.
Treatment
To avoid severe complications and preserve vision, fungal keratitis must be treated promptly and aggressively. The treatment usually consists of antifungal medications, but in some cases, surgical intervention is required.
- Topical Antifungal Medications: – Natamycin is the primary treatment for filamentous fungi like Fusarium and Aspergillus. Natamycin 5% eye drops are initially applied frequently (every 1-2 hours) and then tapered according to clinical response.
• Voriconazole: Voriconazole, which is effective against both filamentous fungi and yeasts, can be used instead of or in addition to natamycin. It is available in both topical and systemic formulations.
- Amphotericin B: This antifungal is particularly effective against yeasts but can also be used to treat filamentous fungi. It is frequently reserved for cases that have not responded to other treatments.
- Oral Antifungal Medications: – Voriconazole: Oral voriconazole is commonly used in combination with topical therapy, especially in severe cases or deep stromal involvement.
- Itraconazole: Another systemic antifungal that can be used as an adjunctive treatment, especially in non-responding cases.
- Intrastromal Injections: – For deep or recalcitrant infections, intrastromal injections of antifungals like voriconazole can deliver high doses directly to the infection site.
- Surgical Interventions: – Debridement: Mechanically removing infected corneal tissue can improve topical antifungal penetration and reduce fungal growth.
- Therapeutic Penetrating Keratoplasty (PKP): In severe or unresponsive cases, corneal transplantation may be required to remove infected tissue and restore vision. This entails replacing the damaged cornea with a donor cornea.
- Lamellar Keratoplasty: A partial thickness corneal transplant can be used to remove infected layers while keeping healthy corneal tissue.
Innovative and Emerging Therapies
- Combination Therapy: – Combining different antifungal agents can improve efficacy and reduce resistance. For example, combining natamycin with voriconazole or amphotericin B can result in broader coverage and more effective treatment.
- Photodynamic Therapy (PDT): Uses light-sensitive compounds activated by specific wavelengths to kill fungal cells. PDT is being investigated as an adjunctive treatment to improve the efficacy of antifungal medications.
- Nanotechnology-Based Drug Delivery: Developing nanocarriers for antifungal drugs can improve drug delivery to the cornea, enhance penetration, and provide sustained release, resulting in increased treatment effectiveness.
- Gene Therapy: Gene therapy research aims to enhance the immune system’s ability to fight fungal infections and reduce inflammation.
- Immune Modulation: – Modifying the immune response to fungal infections could lead to new therapeutic options, especially for cases where the immune system exacerbates tissue damage.
Combining standard treatments with these novel approaches may result in more effective management of fungal keratitis, potentially reducing disease severity and improving patient outcome.
Best Practices for Avoiding Fungal Keratitis
- Protective Eyewear: – Use protective eyewear for activities that could cause eye injury, such as gardening, farming, or handling plant material.
- Maintain proper contact lens hygiene by cleaning and disinfecting regularly, avoiding overnight wear unless prescribed, and using sterile solutions.
- Seek immediate medical attention for eye injuries, particularly those involving plant material or soil, to prevent infection.
- Avoid Contaminated Water: – Avoid swimming or bathing in contaminated water while wearing contact lenses to prevent fungi from entering the eyes.
- Schedule regular eye examinations to detect and treat early signs of infection or ocular conditions.
- Awareness of Symptoms: – Be aware of the symptoms of fungal keratitis, which include severe eye pain, redness, blurred vision, discharge, and photophobia, and seek immediate medical attention if they appear.
- Managing Ocular Surface Diseases: – Address underlying conditions like dry eye syndrome or chronic keratitis to prevent secondary infections.
- Immunocompromised Precautions: – People with compromised immune systems should take extra precautions to avoid fungal infections.
Individuals who follow these preventive measures can significantly reduce their risk of developing fungal keratitis while also maintaining good ocular health.
Trusted Resources
Books
- “Keratitis: Diagnosis and Treatment” by Thomas Reinhard and Frank Larkin
- “Ocular Infection: Investigation and Treatment in Practice” by Edward Holland and Mark J. Mannis
Online Resources
- American Academy of Ophthalmology: AAO
- National Eye Institute: NEI
- Mayo Clinic: Mayo Clinic
- Centers for Disease Control and Prevention: CDC










