What is neuromyelitis optica?
Neuromyelitis Optica (NMO), also known as Devic’s Disease, is a rare autoimmune disorder affecting primarily the optic nerves and spinal cord. This condition causes severe inflammation and demyelination, resulting in optic neuritis and transverse myelitis. These episodes can cause sudden vision loss and various levels of paralysis. Unlike multiple sclerosis (MS), which it is frequently confused with, NMO is distinguished by the presence of a specific antibody called aquaporin-4 (AQP4-IGG). Early diagnosis and treatment are critical for managing symptoms and avoiding relapses.
In-Depth Look at Neuromyelitis Optica
Neuromyelitis Optica is a severe and chronic disorder in which the immune system mistakenly attacks the body’s own central nervous system, particularly the optic nerves and spinal cord. The pathogenesis, clinical manifestations, associated complications, and underlying mechanisms provide a complete picture of this complex condition.
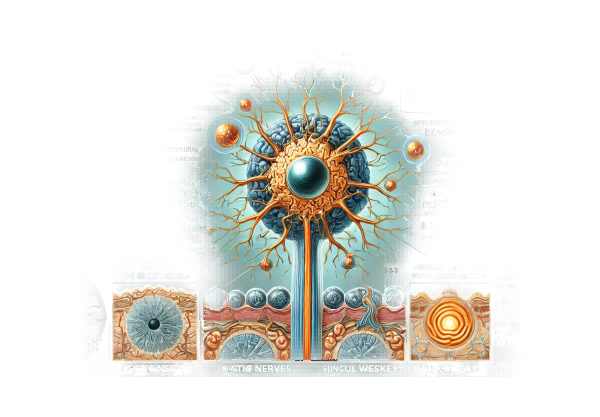
Pathophysiology
NMO’s main target is the water channel protein aquaporin-4 (AQP4), which is abundant in astrocytes, a type of glial cell in the central nervous system. Most patients have AQP4-IgG antibodies, indicating an autoimmune response to these channels. The binding of these antibodies to AQP4 triggers a series of inflammatory responses, resulting in the destruction of astrocytes and subsequent demyelination. This process disrupts nerve impulse transmission, resulting in the NMO-specific symptoms.
Clinical Features
Neuromyelitis Optica manifests as distinct clinical episodes primarily affecting the optic nerves and spinal cord.
Optic Neuritis.
Optic neuritis in NMO typically manifests as:
- Acute Vision Loss: Patients frequently report rapid vision loss in one or both eyes, which can be partial or complete.
- Eye Pain: Pain, especially during eye movement, is a common symptom.
- Visual Field Defects: Loss of vision can occur in certain areas of the visual field.
- Color Vision Impairment: Patients may experience a decrease in their ability to perceive colors accurately.
Transverse Myelitis
Transverse myelitis in NMO manifests as:
- Sudden Onset of Paraplegia or Quadriplegia: Depending on the degree of spinal cord involvement, patients may experience severe limb weakness or paralysis.
- Sensory Deficits: Loss of sensation, such as numbness and tingling, usually occurs below the level of spinal cord inflammation.
- Bladder and Bowel Dysfunction: Incontinence or difficulty urinating and passing stools is common.
- Lhermitte’s Sign: A sudden electric-shock-like sensation that runs down the spine after neck flexion.
Differential Diagnosis
Differentiating NMO from other neurological conditions, especially multiple sclerosis (MS), is critical but difficult. Key differences include:
- Lesion Location and Severity: NMO lesions are usually longitudinally extensive, affecting three or more vertebrae in the spinal cord, whereas MS lesions are shorter.
- Antibody Presence: AQP4-IgG antibodies are highly specific to NMO and do not appear in MS.
- Clinical Course: NMO is characterized by relapses and severe attacks, whereas MS can have a more variable clinical course, including progressive forms.
Epidemiology
Neuromyelitis Optica is a rare disorder, with an estimated incidence of 1-10 per 100,000 people. It affects women more than men, with a female-to-male ratio of around 9:1. The condition can occur at any age, but it usually appears in adults around the age of 40.
Etiology
The exact cause of NMO is unknown, but it is thought to be a combination of genetic susceptibility and environmental factors. Some identified risk factors and associations are:
- Genetic Factors: Certain HLA alleles increase the risk of developing NMO.
- Infections: Viral infections can trigger an autoimmune response.
- Other Autoimmune Disorders: Patients with NMO frequently have a history of other autoimmune diseases, such as systemic lupus erythematosus or Sjogren’s syndrome.
Complications
Neuromyelitis Optica can cause serious complications, affecting both physical and neurological functions.
- Permanent Vision Loss: Recurrent episodes of optic neuritis can permanently damage the optic nerves.
- Paralysis: Severe transverse myelitis can lead to permanent paralysis or quadriplegia.
- Chronic Pain: Neuropathic pain is a common and severe symptom in NMO patients.
- Respiratory Failure: Significant cervical spinal cord involvement can impair respiratory muscles, resulting in respiratory insufficiency.
- Psychosocial Impact: The chronic and severe nature of NMO can cause significant psychological distress, such as depression and anxiety.
Prognosis
The prognosis for NMO varies greatly among patients. Many patients can manage their symptoms and avoid severe disability by receiving an early diagnosis and appropriate treatment. However, due to the disease’s relapsing nature, ongoing medical care and monitoring are required to manage relapses and preserve quality of life.
Diagnosing Neuromyelitis Optica
Clinical evaluation, imaging studies, laboratory tests, and, in some cases, cerebrospinal fluid analysis are all required for an accurate diagnosis of Neuromyelitis Optica. Early and accurate diagnosis is critical for initiating appropriate treatment and avoiding relapses.
Clinical Evaluation
A thorough clinical evaluation consists of a detailed patient history and a neurological examination to identify symptoms consistent with NMO. Key aspects to assess include:
- Visual Acuity and Field Testing: Determines the degree of vision loss and specific visual field deficits.
- Neurological Examination: Assesses muscle strength, sensation, reflexes, and coordination to determine spinal cord involvement.
Imaging Studies 1. Magnetic Resonance Imaging (MRI): MRI is the primary method for diagnosing NMO. It can produce detailed images of the brain, optic nerves, and spinal cord. The key MRI findings in NMO are:
- Longitudinally Extensive Spinal Cord Lesions: Lesions that cover three or more vertebral segments.
- Optic Nerve Enhancements: Indicates inflammation and demyelination.
- Brain Lesions: Although uncommon, some NMO patients may develop brain lesions, particularly in the hypothalamus or brainstem.
Laboratory Tests 1. Serum Aquaporin-4 Antibody Test (AQP4-IgG): The presence of AQP4-IgG antibodies in the blood is highly specific for NMO and serves as a diagnostic marker. Testing for these antibodies distinguishes NMO from similar conditions like MS. Myelin Oligodendrocyte Glycoprotein Antibody (MOG-IgG): In some cases, testing for MOG-IgG antibodies may be beneficial, particularly in patients who are negative for AQP4-IgG but have clinical features suggestive of NMO.
Cerebral Spinal Fluid (CSF) Analysis
CSF analysis can provide useful diagnostic information:
- Pleocytosis: During acute attacks, the CSF contains an elevated number of white blood cells.
- Oligoclonal Bands: Unlike MS, NMO patients usually do not have oligoclonal bands in their CSF.
Neuromyelitis Optica Treatment
The treatment for Neuromyelitis Optica (NMO) focuses on managing acute attacks, preventing relapses, and addressing symptoms to improve quality of life. The approach is multifaceted, including immunosuppressive therapies, symptomatic treatments, and new experimental therapies.
Acute Attack Management
- High-Dose Corticosteroids: Intravenous methylprednisolone is commonly given at high doses for several days to reduce inflammation and treat acute cases of optic neuritis or transverse myelitis.
- Plasma Exchange (Plasmapheresis): Plasma exchange can help patients who do not respond to corticosteroids. This procedure consists of removing the patient’s blood plasma, which contains the harmful antibodies, and replacing it with donor plasma or a plasma substitute.
Long-Term Immunosuppressive Treatment
- Azathioprine: This immunosuppressant is commonly used to reduce the number of relapses. It works by inhibiting the proliferation of immune cells that cause inflammation.
- Mycophenolate Mofetil: Mycophenolate mofetil, another immunosuppressive agent, helps to prevent relapses by targeting the immune cells that cause the autoimmune response.
- Rituximab: A monoclonal antibody that eliminates B cells that are involved in the production of AQP4-IgG antibodies. Rituximab is effective in lowering relapse rates and improving patient outcomes in NMO.
- Methotrexate: An alternative immunosuppressive drug for patients who cannot tolerate other medications.
Symptomatic Treatment
- Pain Management: Neuropathic pain is prevalent in NMO patients. Gabapentin, pregabalin, and duloxetine are common pain relievers.
- Physical Therapy: Rehabilitation and physical therapy are critical for restoring mobility, strength, and overall function, particularly following an acute attack.
- Bladder and Bowel Management: Medication and behavioral strategies are used to treat bladder and bowel dysfunction caused by spinal cord involvement.
Emerging Therapies
- Eculizumab is a monoclonal antibody that targets the complement system, which contributes to the inflammatory response in NMO. Clinical trials have shown that eculizumab is effective in reducing relapses.
- Satralizumab is an interleukin-6 receptor inhibitor that has shown promise in lowering relapse rates in NMO patients. It works by modulating the disease’s inflammatory pathways.
- Inebilizumab: A monoclonal antibody that targets CD19 on B cells and causes their depletion. Clinical trials have shown that inebilizumab is effective at preventing relapses.
- Stem Cell Therapy: Experimental research is looking into the use of autologous hematopoietic stem cell transplantation to reset the immune system and potentially provide long-term remission in NMO patients.
Supportive Care 1. Psychological Support: Counseling and psychological support are crucial for addressing emotional and mental health challenges associated with a chronic condition like NMO. 2. Occupational Therapy: Assists patients in maintaining independence despite physical limitations caused by the disease.
Effective Ways to Improve and Prevent Neuromyelitis Optica
Preventing and managing Neuromyelitis Optica requires proactive strategies and early intervention to reduce symptoms and complications. Here are a few effective methods:
- Regular Monitoring: Schedule regular medical check-ups and imaging studies to track the progression of NMO and identify complications early.
- Medication Adherence: Take immunosuppressive medications as prescribed to reduce the risk of relapse and effectively manage symptoms.
- Healthy Lifestyle: Eat a well-balanced diet, exercise regularly, and avoid smoking to improve overall health and lower the risk of complications from NMO.
- Manage Infections Promptly: Treat infections as soon as possible because they can cause relapses. Stay up to date on vaccinations to avoid common infections.
- Stress Management: Use stress-reduction techniques like yoga, meditation, or mindfulness to help manage the emotional and psychological effects of NMO.
- Symptom Monitoring: Keep track of any new or worsening symptoms and report them to your healthcare provider right away to ensure prompt treatment.
- Support Networks: Connect with support groups and communities where people with NMO can share their experiences, access information, and receive emotional support.
- Physical Activity: Perform regular physical activity that is appropriate for your abilities in order to maintain strength, flexibility, and overall well-being.
Trusted Resources
Books
- “Neuromyelitis Optica Spectrum Disorders” by Dean Wingerchuk
- “Mayo Clinic Guide to Living with a Spinal Cord Injury” by Mayo Clinic
- “Multiple Sclerosis and Related Disorders: Clinical Guide to Diagnosis, Medical Management, and Rehabilitation” by Alexander D. Rae-Grant










