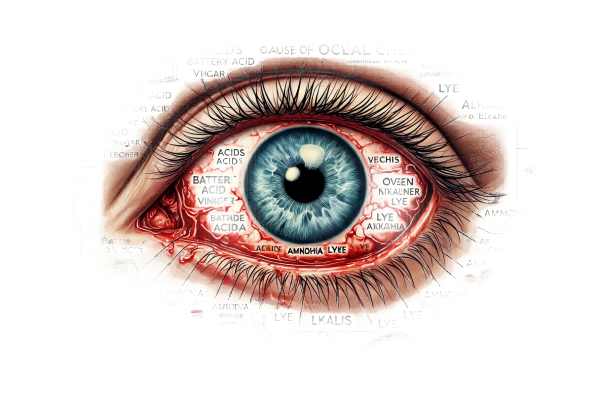
What is Ocular Chemical Burn?
Ocular chemical burns are serious injuries caused by exposing the eyes to acidic or alkaline substances. These burns can cause significant damage to the eye’s structures, resulting in pain, vision impairment, and even blindness if not treated quickly and properly. Chemical burns to the eye are considered medical emergencies and require immediate attention to prevent further damage and preserve vision. They can occur in a variety of settings, including workplaces, laboratories, and even the home, highlighting the importance of understanding their causes and consequences.
Inside Ocular Chemical Burns
Causes of Ocular Chemical Burns
Ocular chemical burns can result from exposure to a variety of substances, typically classified as acids or alkalis.
- Alkaline Burns: These are more common and typically more severe than acid burns. Alkalis like ammonia, lye (sodium hydroxide), lime (calcium hydroxide), and cement can penetrate the ocular tissues and cause extensive damage. The high pH of these substances causes saponification of cell membranes and collagen destruction, resulting in cell death and tissue injury.
- Acid Burns: Acids like sulfuric acid (found in car batteries), hydrochloric acid, and hydrofluoric acid cause coagulation necrosis, limiting deeper penetration into the eye but still causing significant surface damage. Acid burns typically result in immediate pain and redness.
Pathophysiology
The type of chemical, concentration, duration of contact, and extent of ocular penetration all influence the severity of an ocular chemical burn. When exposed, the chemical agent reacts with the ocular surface, causing immediate damage to the corneal epithelium and conjunctiva. The subsequent inflammatory response can cause additional complications.
- Initial Injury: The corneal epithelium suffers the most damage, resulting in cell death and loss of protective barrier function. This increases the likelihood of infection and subsequent damage.
- Inflammatory Response: After the initial injury, an inflammatory response occurs, which is characterized by the release of cytokines and other inflammatory mediators. In severe cases, this response can lead to corneal stromal damage, ulceration, and even perforation.
- Healing and Scarring: The healing process involves re-epithelialization, which can be hampered by persistent inflammation and infection. Fibroblasts and myofibroblasts help with wound healing, but they can also cause scarring, vascularization, and corneal opacity, resulting in long-term visual impairment.
Symptoms
The symptoms of an ocular chemical burn can vary depending on the severity of the injury, but generally include:
- Pain and Discomfort: Immediate and severe pain is common, with some describing it as a burning sensation. Patients may also experience a foreign body sensation in their eye.
- Redness and Swelling: The affected eye is frequently red and swollen due to inflammation and irritation of the conjunctiva and surrounding tissues.
- Tearing and Discharge: Increased tearing is a natural response to flush out the irritant, whereas discharge could indicate a secondary infection.
- Blurred Vision: The extent of corneal damage determines whether vision becomes blurred or hazy.
- Photophobia: Light sensitivity is common, as the damaged corneal surface is more susceptible to irritation from light exposure.
- Blepharospasm: The involuntary closing of the eyelids as a protective response to pain or irritation.
Complications
Ocular chemical burns can cause a variety of complications, especially if not treated promptly and appropriately.
- Corneal Ulceration and Perforation: Severe burns can cause deep corneal ulcers, which can progress to perforation, resulting in vision loss and the need for surgical intervention.
- Symblepharon Formation: Adhesions between the palpebral and bulbar conjunctiva may form, restricting eye movement and causing discomfort.
- Limbal Stem Cell Deficiency: Damage to the limbal region may impair the eye’s ability to regenerate corneal epithelium, resulting in persistent epithelial defects and neovascularization.
- Glaucoma: Inflammation and scarring can cause elevated intraocular pressure, which can lead to optic nerve damage and vision loss.
- Cataracts: Chronic inflammation and steroid treatment can speed up the formation of cataracts.
- Infection: The compromised ocular surface is more vulnerable to bacterial, fungal, or viral infections, which can exacerbate healing and jeopardize vision.
Risk Factors
Certain factors may increase the risk of ocular chemical burns:
- Occupational Hazards: Workers in chemical-intensive industries, such as construction, manufacturing, and laboratory work, are at a higher risk.
- Household Chemicals: Common household cleaning agents, pesticides, and automotive fluids can be hazardous if not handled properly.
- Lack of Protective Gear: Failure to wear appropriate eye protection when handling chemicals significantly increases the risk of exposure and injury.
Prognosis
The prognosis for ocular chemical burns is dependent on the severity of the injury and the timing of treatment. Mild burns typically heal with minimal intervention and produce good visual outcomes. However, even with aggressive treatment, severe burns can cause significant scarring, vision loss, and long-term complications. Early and effective management is critical for improving the prognosis and limiting long-term damage.
Methods for Diagnosing Ocular Chemical Burns
Clinical Examination
A thorough clinical examination is required to diagnose ocular chemical burns. The key components of the examination are:
- Patient History: Gathering detailed information about the chemical involved, its concentration, duration of exposure, and any first aid measures taken is critical for determining the severity of the burn.
- Visual Acuity Test: Measuring visual acuity helps determine the effect of the burn on vision and guides treatment decisions.
- Slit-Lamp Examination: An ophthalmologist can use a slit-lamp microscope to closely examine the anterior segment of the eye, which includes the cornea, conjunctiva, and anterior chamber. This examination helps to determine the extent of epithelial damage, corneal stromal involvement, and the presence of foreign particles.
- pH Testing: Measuring the pH of the ocular surface with pH paper can help determine the residual alkalinity or acidity after initial irrigation, guiding future irrigation needs.
Staining Techniques
- Fluorescein Staining: A fluorescein dye is applied to the ocular surface to highlight epithelial damage. Under cobalt blue light, areas of corneal abrasion or ulceration will appear bright green, allowing for a more detailed assessment of the extent of injury.
- Lissamine Green Staining: Lissamine green can detect damage to conjunctival and corneal epithelial cells, providing additional information about the extent of surface damage.
Imaging Studies
- Ocular Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the cornea, allowing for precise measurements of stromal thickness and tissue damage.
- Ultrasound Biomicroscopy: This imaging technique assesses deeper ocular structures, such as the anterior chamber and lens, which may be damaged by severe burns.
Additional Diagnostic Tests
- Intraocular Pressure Measurement: Monitoring intraocular pressure is critical because chemical burns can lead to secondary glaucoma. To avoid optic nerve damage, elevated intraocular pressure must be treated promptly.
- Cultures and Sensitivity Testing: If there is a suspicion of secondary infection, ocular surface cultures can help identify the causative organism and guide appropriate antibiotic treatment.
Ocular Chemical Burn Treatment
Immediate First Aid
- Irrigation: The first and most important step in treating an ocular chemical burn is complete irrigation of the eye. To remove the chemical agent, do this immediately. Sterile saline or balanced salt solutions are preferred, but clean water can be used if they are not available. Irrigation should last at least 15-30 minutes, depending on the severity and type of chemical used. Evert the eyelids to ensure that no chemical remains.
Medical Treatment
- Topical Medication:
- Antibiotic Eye Drops/Ointments: Erythromycin or ciprofloxacin are common broad-spectrum antibiotic drops or ointments used to prevent infection.
- Cycloplegic Agents: Drugs such as atropine or cyclopentolate help to alleviate pain by relaxing the ciliary muscles and preventing painful muscle contractions.
- Steroid Eye Drops: Using corticosteroid drops for a short period of time can reduce inflammation and scarring. However, they should be used with caution to avoid delaying epithelial healing and increasing the risk of infection.
- Pain management:
- Oral Analgesics: Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can alleviate pain and discomfort.
- Topical NSAIDs: These can be used to alleviate pain and inflammation, but their use should be carefully monitored to avoid corneal toxicity.
- Artificial tears and lubricants:
- Using preservative-free artificial tears on a regular basis can help keep the ocular surface moist and speed up the healing process.
Surgical Interventions
- Debridement: If there is significant necrotic tissue on the ocular surface, surgical debridement may be required to remove dead tissue and promote healing.
- Amniotic Membrane Transplantation: This novel treatment involves applying an amniotic membrane to the ocular surface to promote healing and reduce inflammation. The amniotic membrane has anti-inflammatory and anti-scarring properties, making it useful for treating severe chemical burns.
- Limbal Stem Cell Transplantation: For patients with limbal stem cell deficiency, transplanting healthy limbal stem cells from the patient’s other eye or from a donor can aid in the restoration of the ocular surface and epithelial healing.
- Corneal Transplantation: When the cornea is severely damaged and vision is significantly impaired, a corneal transplant (penetrating keratoplasty) may be required to restore vision.
Emerging and Innovative Therapeutics
- Growth Factors and Cytokine Therapy: Researchers are investigating the use of growth factors and cytokines to promote healing and reduce scarring. These biological agents can improve the regenerative capacity of the ocular surface.
- Gene Therapy: New research is looking into using gene therapy to increase the expression of protective and regenerative factors in the eye, potentially opening up new treatment options for severe chemical burns.
- Biomaterial Scaffolds: Advances in biomaterials are enabling the development of scaffolds that can aid in tissue regeneration and repair in the eye. These scaffolds serve as a framework for cellular growth and healing.
- Anti-Inflammatory and Anti-Scarring Agents: New pharmacological agents that target specific inflammatory and scarring pathways are being studied to improve outcomes in patients suffering from ocular chemical burns.
Effective Ways to Improve and Prevent Ocular Chemical Burns
- Use Protective Eyewear: Always wear safety goggles or face shields when working with chemicals, whether in a laboratory, workplace, or at home, to avoid accidental splashes into the eyes.
- Proper Chemical Storage: Keep chemicals in clearly labeled and secure containers. Keep hazardous substances out of children’s reach and store them according to safety guidelines.
- Immediate Access to Eyewash Stations: Make sure that eyewash stations are easily accessible and functional in workplaces and laboratories that use chemicals. Know where these stations are and how to use them properly.
- Education and Training: Regularly educate and train employees and family members on proper chemical handling, emergency procedures, and the importance of wearing protective equipment.
- Safe Handling Practices: Follow chemical safety protocols when handling and disposing of them. Do not mix chemicals unless specifically instructed to do so under controlled conditions.
- First Aid Preparedness: Be prepared to provide first aid in the event of chemical exposure. Know the first steps to take, such as irrigation, and keep emergency contact information readily available.
- Regular Safety Audits: Perform regular safety audits in workplaces and laboratories to identify potential hazards and ensure adherence to safety standards.
- Label and Read Instructions: Before using any chemical, always read and follow the instructions and warnings on the label. Make sure all containers are clearly labeled with their contents and hazard information.
- Personal Hygiene: After handling chemicals, wash your hands thoroughly, even if you were wearing gloves. When working with chemicals, avoid touching your face or eyes.
- Ventilation: Provide adequate ventilation in areas where chemicals are used to reduce the risk of inhalation and accidental splashes.
Trusted Resources
Books
- “Chemical Eye Injuries” by A. J. Bron and M. W. D. Ferguson
- “Emergency Care and Management of Ocular Trauma” by Thomas J. Wolf and M. Linda Workman
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
Online Resources
- American Academy of Ophthalmology: AAO.org
- National Eye Institute: NEI.nih.gov
- Mayo Clinic: MayoClinic.org
- All About Vision: AllAboutVision.com
- MedlinePlus: MedlinePlus.gov
- Centers for Disease Control and Prevention (CDC): CDC.gov
- PubMed: PubMed.gov
- World Health Organization (WHO): WHO.int






