What is posterior uveitis?
Posterior uveitis is an inflammatory condition that affects the choroid, retina, and optic nerve head. This condition is part of a larger group of diseases known as uveitis, which is defined by inflammation of the uveal layer of the eye. If not diagnosed and treated promptly, posterior uveitis can cause vision impairment or blindness. The condition is frequently associated with symptoms such as blurred vision, floaters, and, in severe cases, vision loss. Furthermore, it may cause eye pain, redness, and light sensitivity.
The causes of posterior uveitis are numerous, ranging from infectious agents such as viruses, bacteria, fungi, and parasites to autoimmune diseases like sarcoidosis, Behçet’s disease, and multiple sclerosis. Idiopathic cases, where the cause is unknown, are also prevalent. A comprehensive eye examination is required to diagnose posterior uveitis, which includes dilated fundus examination, optical coherence tomography (OCT), and fluorescein angiography. Laboratory tests and imaging studies may also be used to diagnose underlying systemic conditions.
Understanding the pathophysiology of posterior uveitis is critical to effective treatment. The inflammatory response can result in complications such as retinal detachment, macular edema, and optic neuropathy. Early detection and appropriate treatment are critical for preventing irreversible damage and preserving vision, so healthcare providers and patients must be well-informed about the condition.
Posterior Uveitis: Management and Treatment
The treatment of posterior uveitis necessitates a comprehensive approach that addresses the underlying cause of inflammation, manages symptoms, and avoids complications. Treatment plans frequently include a combination of medications, lifestyle changes, and, in some cases, surgical procedures.
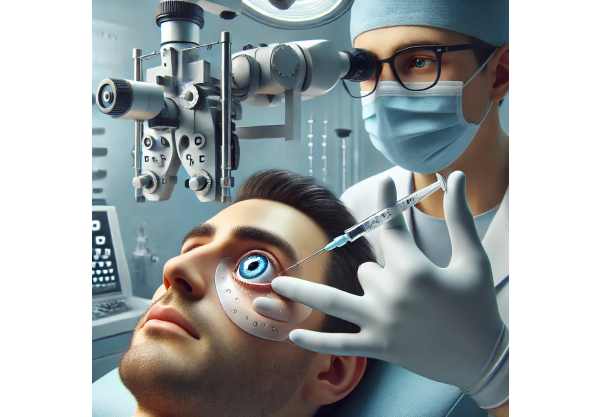
Corticosteroids are the primary treatment for posterior uveitis due to their potent anti-inflammatory properties. They are available in a variety of dosage forms, including oral tablets, periocular injections, and intravitreal injections. Oral prednisone is widely used for its systemic effects, but long-term use necessitates close monitoring due to potential side effects such as hypertension, diabetes, and osteoporosis. Periocular and intravitreal injections deliver steroids directly to the site of inflammation, reducing systemic side effects while providing targeted relief.
Immunosuppressive agents are frequently used when corticosteroids alone are insufficient or when chronic inflammation requires long-term treatment. Drugs like methotrexate, azathioprine, and mycophenolate mofetil aid in immune control and reduce the frequency of relapses. Biologic agents, such as tumor necrosis factor (TNF) inhibitors like infliximab and adalimumab, have also demonstrated efficacy in treating refractory posterior uveitis. These biologics target specific immune system pathways, allowing for more precise control of inflammation.
Antimicrobial therapy is required for all infectious causes of posterior uveitis. The pathogen’s identification influences the choice of antibiotics, antivirals, or antifungals. In cases of toxoplasmosis, for example, pyrimethamine, sulfadiazine, and folinic acid are frequently prescribed. Antiviral medications like ganciclovir and valganciclovir are used to treat viral infections such as cytomegalovirus (CMV) retinitis.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can help with symptom relief, especially in milder cases. They help reduce pain and inflammation and can be combined with other treatments to improve overall efficacy.
In severe cases, surgical intervention may be required to address complications such as retinal detachment, vitreous hemorrhage, or macular edema. Procedures such as vitrectomy, retinal detachment repair, and macular laser therapy can all help to restore and preserve vision.
Patients with posterior uveitis require regular follow-up and monitoring. Eye exams, imaging studies, and laboratory tests all help to determine the progression of the disease and the efficacy of treatment. Adjustments to the treatment plan may be required depending on the patient’s response and any side effects.
Innovative Posterior Uveitis Treatment Options
Recent advances in medical research and technology have transformed the treatment landscape for posterior uveitis. These advances have resulted in more effective and targeted therapies, thereby improving patient outcomes and lowering the burden of this difficult condition. Below, we look at some of the most innovative treatments and their impact on posterior uveitis management.
Biological Therapies
Biologic agents have transformed the treatment of posterior uveitis, especially for patients who do not respond well to standard therapies. These medications target specific components of the immune system, providing a more targeted approach to inflammation control. Tumor necrosis factor (TNF) inhibitors, including infliximab and adalimumab, have shown promise in treating refractory cases. These agents work by neutralizing TNF, a cytokine involved in systemic inflammation, which reduces ocular inflammation and protects tissues. Clinical trials have demonstrated their efficacy in achieving remission and reducing the frequency of relapses in patients with severe posterior uveitis.
Tocilizumab, an IL-6 receptor antagonist, is another well-known biologic therapy. Tocilizumab modulates the immune response by blocking the IL-6 pathway, and it has proven effective in treating autoimmune conditions associated with posterior uveitis. Biologics require careful patient selection and monitoring due to potential side effects, but their ability to provide long-term remission makes them an important addition to the therapeutic arsenal.
Advanced Imaging Techniques
Accurate diagnosis and monitoring of posterior uveitis are critical for successful treatment. Recent advances in imaging technology have greatly improved our ability to detect and assess the severity of inflammation. Enhanced depth imaging optical coherence tomography (EDI-OCT) enables detailed visualization of the posterior uvea and surrounding structures, facilitating early detection and precise monitoring of treatment response. EDI-OCT can detect subtle changes in tissue structure and inflammation, allowing for timely intervention and treatment adjustments.
Furthermore, ultra-widefield fundus imaging provides a comprehensive view of the retina and choroid, making it easier to detect complications like retinal detachment or choroidal effusion. The ability to capture high-resolution images of the entire posterior segment improves diagnostic accuracy and helps to assess treatment efficacy.
Minimal Invasive Drug Delivery Systems
Corticosteroids and immunosuppressive agents administered systemically have the potential to cause serious side effects. Minimally invasive drug delivery systems, such as intravitreal implants and sustained-release devices, provide targeted therapy while minimizing systemic exposure. Dexamethasone intravitreal implants, for example, provide localized anti-inflammatory effects while maintaining drug release, reducing the need for frequent injections and systemic side effects. These implants have been shown to effectively reduce inflammation and improve visual outcomes in patients with posterior uveitis.
Another exciting development is the use of biodegradable micro- and nanoparticles for drug delivery. These systems can encapsulate anti-inflammatory drugs and slowly release them at the site of inflammation, resulting in long-lasting therapeutic effects. Research into optimizing these delivery systems continues, with the goal of achieving even more precise and sustained drug release, which will improve patient compliance and outcomes.
Genetic Therapy
Gene therapy is a cutting-edge approach that has the potential to transform the treatment of posterior uveitis. Gene therapy, which targets the genetic and molecular pathways involved in inflammation, aims to provide long-term relief and potentially cure the disease. CRISPR-Cas9 gene editing and viral vector-mediated gene transfer are two techniques being investigated for modulating immune responses and reducing chronic inflammation.
Although still in the experimental stages, preliminary findings from preclinical studies are encouraging. Gene therapy has the potential to provide personalized treatment by targeting the underlying genetic factors that contribute to posterior uveitis. Ongoing research and clinical trials will be necessary to determine the safety, efficacy, and feasibility of this novel approach.
Artificial Intelligence, Machine Learning
AI and machine learning are transforming ophthalmology, including the treatment of posterior uveitis. AI algorithms can identify patterns and predict disease progression by analyzing large datasets containing imaging studies, clinical records, and genetic information. This capability enables early diagnosis, personalized treatment plans, and improved monitoring strategies.
Machine learning models can help distinguish posterior uveitis from other ocular conditions with similar presentations, reducing diagnostic time and improving treatment outcomes. Furthermore, AI-powered platforms can continually learn from new data, improving predictive accuracy and clinical decision-making over time.
Telemedicine & Remote Monitoring
The COVID-19 pandemic has accelerated the use of telemedicine, and its applications in treating posterior uveitis are becoming more apparent. Telemedicine platforms facilitate remote consultations, allowing patients to receive expert care without the need for frequent in-person visits. This approach is especially useful for patients who have mobility issues or live in remote areas.
Remote monitoring tools, such as smartphone apps and wearable devices, can track symptoms, medication adherence, and treatment outcomes in real time. These technologies allow for more timely interventions and therapy adjustments, which improves disease control and patient satisfaction.






