What is uveitis?
Uveitis is a broad term for inflammation of the uveal tract of the eye, which includes the iris, ciliary body, and choroid. These structures work together to provide blood supply to the retina, control the amount of light entering the eye, and produce the aqueous humor, which helps to keep intraocular pressure stable. Uveitis can affect one or more parts of the uveal tract, and depending on the exact location and severity of the inflammation, it can cause a variety of symptoms, including vision loss if not treated.
Types of Uveitis
The location of the inflammation within the eye determines which type of uveitis it is:
- Anterior Uveitis: This is the most common type of uveitis, in which inflammation affects the eye’s anterior segment, including the iris and anterior chamber. It is also known as iritis or iridocyclitis when it affects the ciliary body. Anterior uveitis can strike unexpectedly, causing pain, redness, light sensitivity (photophobia), and blurred vision. It is frequently associated with autoimmune conditions such as ankylosing spondylitis, reactive arthritis, and juvenile idiopathic arthritis, but it can also occur independently or in conjunction with infections.
- Intermediate Uveitis: This type of uveitis causes inflammation primarily in the vitreous and peripheral retinas. It is also known as pars planitis when the inflammation only affects the pars plana region of the ciliary body. Intermediate uveitis is frequently associated with systemic conditions like multiple sclerosis, sarcoidosis, and Lyme disease. Symptoms of intermediate uveitis include floaters, blurred vision, and, less commonly, pain or redness.
- Posterior Uveitis: Posterior uveitis is an inflammation of the retina and choroid, the back part of the eye. This type of uveitis is less common but more serious because it directly affects the structures involved in vision. Symptoms of posterior uveitis include blurry vision, floaters, and visual field loss. It is frequently associated with infectious diseases like toxoplasmosis, tuberculosis, and syphilis, as well as systemic autoimmune disorders like Behçet’s disease and lupus.
- Panuveitis: Panuveitis is a severe type of uveitis that causes inflammation in all layers of the uvea, including the anterior, intermediate, and posterior segments. This type of uveitis can cause extensive eye damage and is frequently associated with systemic inflammatory diseases like Vogt-Koyanagi-Harada, sarcoidosis, and Behçet’s disease. Panuveitis symptoms may include pain, redness, blurred vision, floaters, and light sensitivity.
Causes and Risk Factors for Uveitis
Autoimmune diseases, infections, trauma, and environmental exposures are all potential causes of uveitis. In many cases, the exact cause of uveitis is unknown, so it is classified as idiopathic. Understanding the potential causes and risk factors is critical for successfully diagnosing and managing the condition.
- Autoimmune and Inflammatory Diseases: Autoimmune diseases are one of the leading causes of uveitis. In these cases, the immune system mistakenly attacks its own tissues, including the uveal tract, resulting in inflammation. Uveitis is commonly associated with the following autoimmune diseases:
- Ankylosing Spondylitis: Ankylosing spondylitis is a type of arthritis that primarily affects the spine and sacroiliac joints. It is strongly associated with anterior uveitis.
- Juvenile Idiopathic Arthritis: The most common form of arthritis in children, juvenile idiopathic arthritis can cause chronic anterior uveitis, especially in those with the oligoarticular subtype.
- Sarcoidosis: Sarcoidosis is a systemic inflammatory disease that can affect several organs, including the lungs and eyes. It is frequently associated with intermediate or posterior uveitis.
- Behçet’s Disease: A rare, chronic inflammatory disorder that causes blood vessel inflammation throughout the body, Behçet’s disease can result in panuveitis, which is characterized by recurrent episodes of inflammation affecting multiple parts of the eye.
- Systemic Lupus Erythematosus (SLE): SLE is an autoimmune disease that can affect nearly every organ system. It can also cause posterior uveitis, resulting in visual disturbances and potential vision loss.
- Infectious Causes: Several infectious agents can cause uveitis, particularly posterior uveitis. These infections may be bacterial, viral, fungal, or parasitic in nature.
Toxoplasmosis, caused by the parasite Toxoplasma gondii, is one of the most common causes of infectious posterior uveitis, resulting in retinal inflammation and scarring.
- Tuberculosis: Mycobacterium tuberculosis, the bacterium responsible for tuberculosis, can cause chronic uveitis, especially in endemic areas.
- Herpesviruses: Viruses like herpes simplex and herpes zoster can cause anterior uveitis, which is frequently associated with corneal involvement or other ocular complications.
- Syphilis: Caused by the bacterium Treponema pallidum, syphilis can result in posterior uveitis, chorioretinitis, and other serious ocular manifestations if not treated.
- Cytomegalovirus (CMV): CMV is a common cause of uveitis in immunocompromised people, including those living with HIV/AIDS. It usually manifests as a form of retinitis with severe vision loss.
- Trauma and Surgery: Ocular trauma or surgical procedures can damage the uveal tract, resulting in inflammation and subsequent uveitis. Traumatic uveitis is usually acute and can be treated effectively, but it can become chronic if not managed properly.
- Drug-Induced Uveitis: Some medications have been linked to uveitis, either through direct toxic effects or immune-mediated mechanisms. Bisphosphonates (used to treat osteoporosis), some antibiotics, and immune checkpoint inhibitors used in cancer treatment are all known to cause uveitis.
- Idiopathic Uveitis: In many cases, no identifiable cause of uveitis can be found, so the condition is classified as idiopathic. Idiopathic uveitis can be difficult to treat because there is no clear underlying cause, but treatment typically focuses on reducing inflammation and preventing complications.
Clinical presentation of uveitis
The symptoms of uveitis differ greatly depending on the type, severity, and duration of the inflammation. However, several common symptoms are frequently associated with uveitis, which can aid in clinical suspicion and diagnosis:
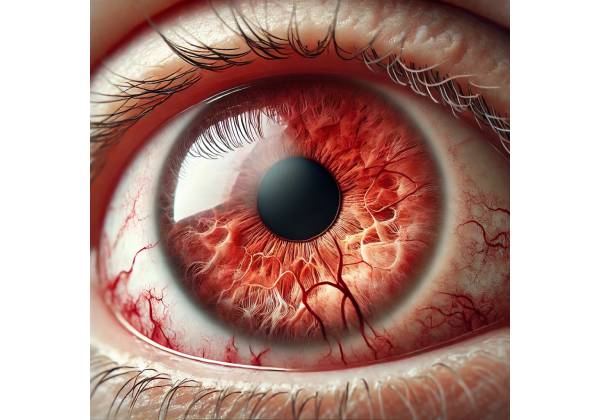
- Eye Redness: The dilation of blood vessels in the conjunctiva and episclera is a common cause of eye redness in anterior uveitis. The redness is usually most noticeable around the cornea (ciliary flush), and it may be painful.
- Pain: Eye pain is a common symptom of acute anterior uveitis, characterized as a deep, aching pain that worsens with eye movement or exposure to bright light. Although intermediate and posterior uveitis are less painful, they can still cause significant discomfort, especially if there is concurrent scleritis or other complications.
- Photophobia: Light sensitivity (photophobia) is common in uveitis, especially in anterior uveitis, where inflammation of the iris and ciliary body causes the eye to become more sensitive to bright light. Photophobia can be severe and debilitating in certain cases.
- Blurred Vision: Blurred or decreased vision is a common symptom of uveitis, especially when it affects the posterior segment of the eye. Macular edema, retinal inflammation, and the presence of inflammatory cells in the vitreous (vitritis) can all cause vision problems.
- Floaters: Patients with intermediate or posterior uveitis may notice small, dark spots or threads moving across their visual field. Inflammatory cells and debris in the vitreous humor cause floaters, which can be a sign of active inflammation.
- Visual Field Loss: In more severe cases of uveitis, particularly posterior uveitis, patients may develop visual field loss or scotomas (blind spots). This could be due to retinal inflammation, optic nerve involvement, or the presence of retinal lesions.
- Headache: Uveitis can cause headaches, especially in cases of anterior uveitis, which inflames the ciliary body and iris. The pain may spread to the forehead, temples, or around the eyes.
- Constricted Pupil: Anterior uveitis can cause the pupil to appear smaller than normal (miosis) due to iris muscle spasm. If there are posterior synechiae (adhesions between the iris and lens), the pupil may be irregular in shape.
Complications of Uveitis
If left untreated or inadequately managed, uveitis can cause a number of serious complications, including permanent vision loss:
- Cataract Formation: Chronic inflammation and long-term use of corticosteroids to treat uveitis can cause cataracts, particularly posterior subcapsular cataracts, which can severely impair vision.
- Glaucoma: Uveitis can progress to secondary glaucoma, which is characterized by high intraocular pressure (IOP) that damages the optic nerve. This can happen due to a variety of factors, including trabeculitis (inflammation of the trabecular meshwork), the formation of peripheral anterior synechiae (adhesions that block the drainage angle), or corticosteroid-induced IOP elevation. Glaucoma, if not treated properly, can cause progressive vision loss and eventually lead to blindness.
- Macular Edema: Macular edema is one of the most common and vision-threatening complications of uveitis, especially in the intermediate and posterior regions. It is characterized by fluid accumulation in the macula, the central part of the retina responsible for sharp, detailed vision. Macular edema can cause significant visual impairment and is difficult to treat, necessitating a combination of anti-inflammatory and anti-VEGF treatments.
- Retinal Detachment: In severe cases of posterior uveitis, chronic inflammation can cause scar tissue and traction on the retina, resulting in retinal detachment. This is an ophthalmic emergency that requires immediate surgical intervention to avoid permanent vision loss.
- Optic Neuritis: Uveitis can occasionally spread to involve the optic nerve, resulting in optic neuritis. This condition is characterized by inflammation of the optic nerve, which causes pain, vision loss, and color vision changes. Optic neuritis can be associated with systemic conditions like multiple sclerosis, necessitating immediate treatment to avoid irreversible damage.
- Band Keratopathy: Chronic anterior uveitis can cause calcium deposition in the corneal epithelium and Bowman’s layer, which results in band keratopathy. This condition manifests as a horizontal, grayish-white opacity on the cornea, causing visual disturbances and discomfort. To remove calcium deposits, treatment may include chelation therapy or corneal scraping.
- Synechiae Formation: Uveitis, especially anterior uveitis, can cause the formation of synechiae, which are adhesions between the iris and other ocular structures. Posterior synechiae exist between the iris and the lens, whereas peripheral anterior synechiae connect the iris to the trabecular meshwork. Synechiae can cause irregular pupil shape, pupillary blockage, and secondary angle-closure glaucoma.
- Cystoid Macular Edema (CME): CME is a type of macular edema in which fluid-filled cysts develop in the macula, causing visual distortion and blurring. CME is especially common in cases of chronic uveitis and can be resistant to treatment, necessitating a combination of corticosteroids, NSAIDs, and intravitreal injections.
- Hypotony: Chronic uveitis can cause hypotony, which is characterized by an abnormally low IOP. Damage to the ciliary body can cause this, as it reduces aqueous humor production. Further complications from hypotony include choroidal detachment, maculopathy, and eye atrophy.
- Epiretinal Membrane (ERM): Chronic inflammation in uveitis can cause the formation of an epiretinal membrane, which is a layer of fibrous tissue on the surface of the retina. ERM can cause visual distortion and blurring, and in severe cases, surgery may be required.
- Choroidal Neovascularization (CNV): Inflammatory processes in posterior uveitis can promote the development of abnormal blood vessels beneath the retina, resulting in CNV. These vessels may leak fluid or bleed, resulting in severe vision loss. Anti-VEGF injections, laser therapy, and surgery are all common treatments for CNV.
- Persistent Vision Loss: Untreated uveitis can cause chronic damage to the ocular structures, resulting in irreversible vision loss. This emphasizes the importance of early detection and aggressive treatment for the condition.
Diagnostic methods
Uveitis diagnosis necessitates a thorough evaluation that includes a detailed patient history, clinical examination, and a variety of diagnostic tests. The goal is to identify the underlying cause of the inflammation, the extent of ocular involvement, and any associated systemic conditions. Accurate diagnosis is critical for determining appropriate treatment and avoiding complications.
Clinical Examination
- Patient History: A thorough patient history is required to diagnose uveitis. The ophthalmologist will inquire about the symptoms’ onset, duration, and nature, which may include pain, redness, photophobia, and visual disturbances. Furthermore, the patient’s medical history, including any known autoimmune diseases, infections, or recent trauma, is examined. A history of systemic symptoms such as joint pain, skin rashes, or neurological symptoms may indicate an underlying systemic condition associated with uveitis.
- Slit-Lamp Examination: Slit-lamp biomicroscopy is an important tool in the diagnosis of uveitis. This examination enables the ophthalmologist to thoroughly examine the anterior segment of the eye, which includes the cornea, anterior chamber, iris, and lens. Keratic precipitates (inflammatory deposits on the corneal endothelium), anterior chamber cells, flare (evidence of active inflammation), and posterior synechiae are all common findings in anterior uveitis. In cases of intermediate or posterior uveitis, the slit-lamp examination can be combined with a fundus lens to look for signs of inflammation in the vitreous and retina, such as vitritis, retinal vasculitis, or chorioretinitis.
- Fundoscopy: A fundoscopy (or ophthalmoscopy) examines the posterior segment of the eye, which includes the retina, choroid, and optic nerve head. An ophthalmologist looks for signs of inflammation, such as optic disc swelling, retinal infiltrates, retinal hemorrhages, and macular edema. Fundoscopy is particularly useful for diagnosing posterior uveitis and determining the severity of ocular involvement.
- Tonometry: Tonometry is essential for measuring intraocular pressure (IOP), especially when uveitis is associated with secondary glaucoma. Elevated IOP indicates the presence of trabeculitis or angle closure mechanisms, whereas low IOP may indicate ciliary body dysfunction and hypotonia.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It is especially effective for detecting macular edema, cystoid macular edema, and epiretinal membranes in uveitis patients. OCT is also useful for monitoring treatment efficacy and detecting recurrent inflammation.
- Fluorescein Angiography (FA): An intravenous injection of fluorescein dye highlights the retinal blood vessels. This imaging technique is useful for diagnosing retinal vasculitis, identifying capillary non-perfusion, and detecting choroidal neovascularization. FA can also aid in the diagnosis of posterior uveitis and the evaluation of treatment efficacy.
- Indocyanine Green Angiography (ICGA): ICGA is similar to FA but uses indocyanine green dye to provide a better view of the choroidal vasculature. ICGA is especially useful in assessing choroidal inflammation, detecting subclinical choroiditis, and diagnosing conditions such as Vogt-Koyanagi-Harada disease or birdshot chorioretinopathy.
- Ultrasound Biomicroscopy (UBM): This technique uses high-frequency ultrasound to visualize the anterior segment of the eye, which includes the ciliary body and peripheral retina. It is especially useful in cases of intermediate uveitis or when examining the anterior segment for synechiae, angle closure, or ciliary body detachments.
Lab Tests
- Blood Tests and Serology: Laboratory tests are required to identify systemic conditions associated with uveitis. To assess systemic inflammation, blood tests may include a complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). Serological tests for specific autoimmune markers such as antinuclear antibodies (ANA), rheumatoid factor (RF), and HLA-B27 can aid in the diagnosis of autoimmune diseases. Infectious causes of uveitis, such as syphilis, tuberculosis, and toxoplasmosis, may necessitate specific serological testing or polymerase chain reaction (PCR).
- Aqueous and Vitreous Sampling: If the underlying cause of uveitis is unknown or an infectious etiology is suspected, sampling of the aqueous humor (from the anterior chamber) or vitreous humor (from the posterior segment) may be performed. These samples are examined for the presence of pathogens, inflammatory cells, or abnormal proteins in order to determine the exact cause of the uveitis.
- Systemic Imaging: Depending on the suspected underlying condition, imaging studies like chest X-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI) may be required. For example, chest X-rays can detect sarcoidosis, whereas MRI can assess neurological involvement in conditions such as multiple sclerosis.
Effective Management of Uveitis
Managing uveitis necessitates a personalized approach that addresses both the underlying cause of inflammation and the disease’s specific manifestations in the eye. The primary treatment goals are to reduce inflammation, preserve vision, avoid complications, and manage any underlying systemic conditions. Treatment options differ depending on the type and severity of the uveitis, as well as the patient’s overall health and response to therapy.
Medical Management
- Corticosteroids: Corticosteroids are the cornerstone of uveitis treatment due to their potent anti-inflammatory properties. They can be administered in a variety of ways, depending on the location and severity of the inflammation.
- Topical Corticosteroids: These are common treatments for anterior uveitis. Prednisolone acetate eye drops are effective at reducing inflammation in the eye’s anterior segment. The frequency of administration is typically high at first (e.g., every hour) and gradually decreases as the inflammation resolves.
- Systemic Corticosteroids: Prednisone, an oral corticosteroid, is used to treat more severe or widespread uveitis, particularly intermediate, posterior, or panuveitis. Systemic steroids are effective at controlling inflammation throughout the body, including the eyes, but long-term use is associated with serious side effects such as weight gain, osteoporosis, hypertension, and an increased risk of infections.
- Periocular and Intravitreal Corticosteroids: Corticosteroid injections into or around the eye (periocular or intravitreal injections) are used when inflammation is limited to the posterior segment or topical and systemic steroids are insufficient. Triamcinolone acetonide is a popular intravitreal corticosteroid that offers targeted treatment with minimal systemic side effects. However, multiple injections may be required, and there is a risk of complications such as increased intraocular pressure (IOP) and cataract formation.
- Immunosuppressive Therapy: Immunosuppressive agents may be required for patients with chronic uveitis or when corticosteroids are ineffective or have significant side effects. This includes:
- Antimetabolites: Drugs like methotrexate, azathioprine, and mycophenolate mofetil suppress immune system activity, lowering the frequency and severity of uveitis flare-ups. They are frequently used in conjunction with low-dose corticosteroids to improve chronic inflammation management.
- T-Cell Inhibitors: Drugs such as cyclosporine and tacrolimus specifically inhibit T-cell function, which is essential in autoimmune responses. These medications are effective in treating systemic autoimmune diseases-related uveitis.
- Biologic Agents: TNF-α inhibitors (e.g., adalimumab and infliximab) target specific inflammatory molecules. These medications are especially effective in treating non-infectious uveitis associated with autoimmune conditions such as Behçet’s disease and rheumatoid arthritis.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, both systemic and topical, are used in conjunction with corticosteroids to treat mild to moderate uveitis. They reduce inflammation and pain, but are less effective than corticosteroids and are typically used in conjunction with other treatments.
- Antimicrobial Therapy: When an infectious agent causes uveitis, proper antimicrobial treatment is required. Treatment options vary depending on the pathogen:
- Antibiotics: Bacterial infections such as tuberculosis or syphilis are treated with antibiotics such as rifampin, isoniazid, and penicillin.
- Antivirals: Acyclovir, valacyclovir, or ganciclovir are used to treat viral uveitis caused by herpes simplex or cytomegalovirus.
- Antifungals: Fungal uveitis, which can occur in immunocompromised patients, is treated with antifungal medications such as voriconazole or amphotericin B.
- Antiparasitic Agents: Toxoplasmosis-induced uveitis is treated with antiparasitic medications such as pyrimethamine and sulfadiazine.
Surgical Management
In some cases, surgical intervention may be required to manage uveitis complications or to treat refractory cases that do not respond to medical therapy.
- Vitrectomy: Pars plana vitrectomy is a surgical procedure that removes the vitreous gel from the eye. It is used in cases of persistent vitritis, vitreous hemorrhage, or retinal detachment caused by uveitis. Vitrectomy can also be used to clear inflammatory debris or treat complications like epiretinal membranes or macular edema.
- Cataract Surgery: Cataract formation is a common side effect of chronic uveitis and prolonged corticosteroid use. Cataract surgery may be required to restore vision in patients with significant cataracts. However, careful perioperative management is required to control inflammation and prevent the uveitis from worsening.
- Glaucoma Surgery: For patients with uveitic glaucoma who do not respond to medical therapy, surgical options such as trabeculectomy or the implantation of glaucoma drainage devices may be required to control IOP and protect the optic nerve.
- Laser Therapy: In some cases of posterior uveitis, laser photocoagulation can be used to treat choroidal neovascularization or prevent retinal detachment. Laser therapy is also used to treat peripheral retinal lesions that are likely to cause tractional detachments.
Monitoring and Follow-up
Given the chronic and recurring nature of uveitis, regular monitoring and follow-up are essential for management. Patients usually require regular eye exams to assess visual acuity, monitor IOP, and look for signs of active inflammation. OCT and fluorescein angiography are examples of imaging studies that can be repeated on a regular basis to assess treatment response and detect complications early. Adjustments to therapy may be required based on disease activity and patient response. Long-term management frequently requires a multidisciplinary approach, with collaboration among ophthalmologists, rheumatologists, infectious disease specialists, and other healthcare providers to address both the ocular and systemic aspects of the disease.
Trusted Resources and Support
Books
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup: This comprehensive textbook covers all aspects of uveitis, from basic science to clinical management. It is a valuable resource for both clinicians and researchers involved in the care of patients with ocular inflammation.
- “Ocular Inflammatory Disease and Uveitis Manual” by Andrew Dick and Peter J. McCluskey: This book provides practical guidance on the diagnosis and management of uveitis and other inflammatory eye diseases. It includes case studies and clinical pearls that are useful for practicing ophthalmologists.
Organizations
- American Uveitis Society (AUS): The AUS is a professional organization dedicated to advancing the understanding and treatment of uveitis. They offer resources for both healthcare professionals and patients, including access to the latest research, clinical guidelines, and educational materials.
- The Ocular Immunology and Uveitis Foundation (OIUF): OIUF provides support and education for patients with uveitis and related ocular conditions. They offer information on treatment options, coping strategies, and access to support groups, helping patients manage the challenges of living with uveitis.










