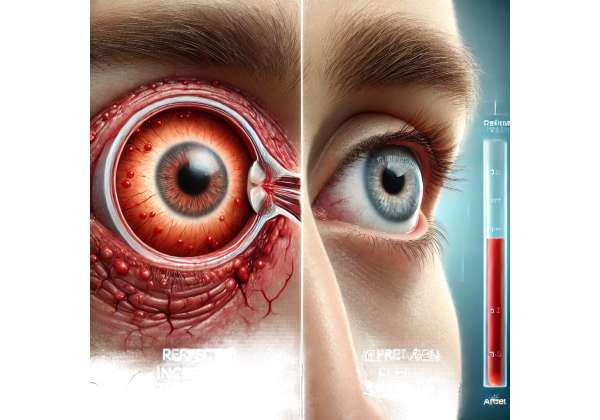
Scleritis is a severe inflammatory disease that affects the tough outer layer of the eye (the sclera), often leading to pain, redness, and, in advanced cases, permanent vision damage. When standard medications like corticosteroids or traditional immunosuppressants fail to control the condition, it is classified as “refractory” scleritis. For these challenging cases, infliximab—a tumor necrosis factor-alpha (TNF-α) inhibitor—has emerged as a promising therapy. While infliximab has been widely used to manage systemic autoimmune disorders such as rheumatoid arthritis, its role in modulating complex eye inflammation is a growing area of clinical interest.
Despite the potential severity of scleritis, many people remain unaware of alternative therapies beyond steroids and classic immunomodulatory drugs. Infliximab’s ability to target TNF-α, a key mediator in inflammatory pathways, offers new hope for individuals who have exhausted first-line treatments. Below, we explore how infliximab can help dampen ocular inflammation, reviewing its application protocols, current research, and what patients can expect regarding effectiveness, safety, and cost considerations.
Why Infliximab May Transform Scleritis Treatment
Scleritis encompasses a spectrum of conditions linked by scleral inflammation. At its most basic, it presents with eye pain, redness, and light sensitivity, but advanced stages may threaten vision if not managed aggressively. In some patients, scleritis aligns with systemic autoimmune disorders like rheumatoid arthritis, granulomatosis with polyangiitis, or inflammatory bowel diseases. In others, scleritis appears in isolation, complicating diagnosis and treatment approaches.
The Immunological Rationale
Infliximab specifically inhibits TNF-α, one of the most potent cytokines driving inflammation in autoimmune diseases. When the immune system misfires and attacks its own tissues, large amounts of TNF-α are released, causing symptoms that can include swelling, tissue destruction, and chronic pain. By binding to TNF-α molecules, infliximab prevents them from exerting their harmful effects on the sclera and surrounding ocular structures. This mechanism contrasts with broader immunosuppressants, which often exert an overarching dampening effect on the immune system. Infliximab’s targeted approach can, in certain scenarios, lead to better symptom control and fewer systemic side effects.
Refractory Scleritis and Beyond
When scleritis is refractory, it typically means high-dose corticosteroids or conventional immunosuppressants (e.g., methotrexate, mycophenolate mofetil) have not managed to keep inflammation at bay. Some patients cannot tolerate these medications long term due to adverse effects, such as bone loss, elevated intraocular pressure, liver toxicity, or uncontrolled blood sugar. Introducing infliximab can provide a dual benefit: potentially increasing therapeutic efficacy while possibly reducing the reliance on steroids. For individuals with concurrent systemic conditions, infliximab may also help manage joint pain or gastrointestinal issues, offering a more holistic approach to treating the underlying autoimmune process.
Other TNF-α Inhibitors and Choosing Infliximab
TNF-α inhibitors as a class include agents like adalimumab and etanercept. However, infliximab has garnered significant attention in ophthalmology, particularly in scleritis, uveitis, and other complex ocular conditions. Clinicians often weigh the following factors when opting for infliximab over other TNF-α inhibitors or immunosuppressants:
- Route of Administration: Infliximab is given intravenously, allowing precise dosing and close monitoring of the infusion process.
- Pharmacokinetics: Its half-life and binding characteristics may provide sustained control of ocular inflammation in specific patients.
- Evidence Base: Clinical reports and case series have documented infliximab’s capacity to induce remission in complex eye inflammation, particularly in those who have not responded to other biologics.
Given that each patient’s medical situation is unique, these decisions are often taken by a multidisciplinary team involving rheumatologists, ophthalmologists, and other specialists familiar with autoimmune pathology. This combined expertise ensures that the potential benefits of infliximab outweigh any associated risks.
Practical Guidelines for Infliximab Administration
For many, intravenous medication can sound intimidating. Understanding how infliximab is administered, monitored, and integrated into an overall treatment plan can ease concerns. Below is a closer look at how clinicians organize infliximab therapy to address scleritis.
Baseline Evaluation and Workup
Before initiating infliximab, doctors often perform a thorough evaluation. This may include:
- Complete Blood Tests: A full blood count, liver enzymes, kidney function tests, and screening for infections like tuberculosis or hepatitis.
- Imaging Studies: Chest X-rays or other scans to rule out latent infections.
- Ophthalmic Assessment: Detailed eye exams using slit-lamp biomicroscopy to document the extent of scleral inflammation, presence of corneal involvement (keratitis), or signs of uveitis.
These evaluations serve two primary purposes. First, they ensure that the patient is a suitable candidate for infliximab, minimizing complications from undiagnosed infections. Second, they establish a baseline for measuring treatment outcomes, enabling clinicians to track improvements or any emerging side effects.
Dosing Schedules and Infusion Protocols
The standard protocol for infliximab involves an induction phase, typically at 0, 2, and 6 weeks, followed by maintenance infusions every 4 to 8 weeks thereafter. However, some ophthalmologists tweak these intervals based on clinical response and disease severity:
- Induction Phase: During the first two months, patients receive a series of infusions to quickly build therapeutic drug levels in the bloodstream.
- Maintenance Phase: Once remission or stable disease control is achieved, the frequency of infusions can be tapered or extended, ensuring ongoing control of scleral inflammation while aiming to limit the overall drug load.
Each infusion lasts about 2 hours or more, though some patients may need slower infusions if they are at higher risk for infusion reactions. Healthcare teams monitor for any signs of allergic or infusion-related events, which can include fever, chills, or changes in blood pressure.
Co-Administration with Other Immunosuppressants
In certain cases, infliximab may be combined with low-dose methotrexate or another immunomodulatory agent. This combination can augment effectiveness and decrease the risk of the body developing antibodies against infliximab. The synergy between infliximab and additional immunosuppressants often prolongs the drug’s effectiveness and helps maintain control of ocular inflammation.
Steroids may still play a role during the early stages of infliximab therapy, especially if a patient’s scleritis is aggressively flaring. However, if infliximab proves effective, many patients can gradually reduce and sometimes discontinue steroids, mitigating the long-term complications associated with high-dose corticosteroid use.
Monitoring Response and Adjusting Therapy
One crucial aspect of scleritis management with infliximab is evaluating clinical response over time. Eye specialists typically rely on a combination of patient-reported symptoms—like pain levels or visual disturbances—and objective measures such as scleral redness or presence of any active inflammatory nodules. Improvement or resolution of these signs usually indicates that infliximab is successfully controlling the condition.
If the patient does not show a substantial response or experiences partial improvements only, doctors may:
- Shorten the Infusion Interval: Administer infliximab more frequently.
- Increase the Dose: Raise the infliximab dose within safe limits.
- Switch to Alternative Biologics: Transition to another TNF-α inhibitor or a different class of biologics (e.g., IL-6 inhibitors), depending on the underlying cause of scleritis and systemic factors.
Regular communication between the patient and healthcare providers is paramount. Addressing mild flares swiftly can prevent severe progression, while vigilant monitoring helps detect side effects before they escalate into serious complications.
Emerging Clinical Evidence on Infliximab for Scleritis
Infliximab’s use in ophthalmology—especially for conditions like refractory scleritis—has steadily gained traction. While robust, large-scale randomized clinical trials are relatively limited in this specific domain, case reports, retrospective studies, and smaller prospective investigations collectively point toward infliximab’s notable efficacy and safety profile.
Key Findings from Peer-Reviewed Publications
Several papers published in reputable ophthalmology and rheumatology journals have shed light on the benefits of infliximab in managing stubborn scleritis:
- Response Rates: Many studies report that over half of patients with refractory scleritis achieve significant improvement in pain, redness, and scleral thickening after a course of infliximab.
- Steroid-Sparing Effects: A consistent observation is the possibility of reducing or discontinuing long-term steroids. For individuals who have experienced serious steroid-related side effects—such as glaucoma, cataracts, or adrenal suppression—this factor is particularly meaningful.
- Reduction in Flare Frequency: While flares can still occur, especially in the context of systemic diseases, infliximab often diminishes both the frequency and severity of these episodes.
In addition to scleritis, infliximab’s advantage extends to other ocular inflammatory conditions like uveitis and retinal vasculitis. Patients who exhibit signs of multi-layer inflammation in the eye may benefit from infliximab if they have a parallel indication for TNF-α inhibition systemically (for example, in Crohn’s disease, ankylosing spondylitis, or psoriatic arthritis).
Comparing Infliximab to Other Biologics
With the expanding palette of biologic therapies, clinicians strive to determine which agent suits a particular subtype of scleritis. Adalimumab, another TNF-α inhibitor, has FDA approval for certain inflammatory eye diseases (e.g., non-infectious uveitis) and is used off-label for scleritis. Some smaller studies suggest comparable efficacy between infliximab and adalimumab for refractory ocular inflammation, but individual patient factors—such as tolerance for subcutaneous injections (adalimumab) versus intravenous infusions (infliximab)—may guide selection.
In specific cases, non-TNF biologics (e.g., rituximab, tocilizumab) show potential efficacy for scleritis, especially when it is associated with anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitides or other complex autoimmune processes. However, infliximab remains an important choice for those needing a well-established and often rapid effect on scleral inflammation.
Challenges and Ongoing Research
The main challenge in the field lies in conducting large-scale, randomized controlled trials to produce definitive guidelines on infliximab’s use for various scleritis subtypes. Several factors impede these studies:
- Rarity of Refractory Scleritis: Scleritis is already considered less common than other inflammatory eye diseases, and true refractory cases constitute an even smaller pool.
- Heterogeneity of Underlying Causes: From rheumatoid arthritis to Wegener’s granulomatosis (granulomatosis with polyangiitis), the spectrum of systemic diseases complicating scleritis is wide.
- Resource Constraints: Clinical trials for biologic agents are expensive, and pharmaceutical companies often prioritize broader indications with larger patient populations.
Nevertheless, smaller prospective studies continue to gather evidence, focusing on optimal dosing strategies and long-term remission rates. Investigations into the molecular mechanisms by which infliximab counteracts ocular autoimmune cascades are also ongoing, which can help refine patient selection criteria and optimize infusion schedules for maximum benefit.
Evaluating Efficacy and Safety Outcomes
Any patient considering infliximab, particularly for an inflammatory condition like scleritis, often wants clear, data-driven insights into how effective the therapy is and what potential risks might arise. Although each person’s experience varies, published data and clinical practice patterns provide a roadmap for setting realistic expectations.
Documented Efficacy in Reducing Pain and Inflammation
One of the hallmarks of scleritis is intense pain, often described as a deep, boring ache that worsens with eye movement. In published case series of patients on infliximab, a large proportion reported a significant decrease in ocular pain. In many scenarios, the sclera’s visible inflammation and redness subsided in tandem. While “remission” can be a loaded term, a considerable subset of patients achieves a stable disease state—no active inflammation—for extended periods when on a well-managed infliximab regimen.
A meaningful measure for ophthalmologists is improvement in best-corrected visual acuity (BCVA). Active scleritis can compromise different structures of the eye—cornea, uvea, retina—especially if inflammation continues unabated. By mitigating the underlying inflammatory process, infliximab helps prevent further tissue damage, preserving or occasionally improving vision.
Potential Risks and Strategies for Minimizing Them
As with any potent immunomodulator, infliximab is associated with a distinct risk profile. Some of the major concerns include:
- Infection Susceptibility: By curbing immune system activity, patients on infliximab can become more vulnerable to infections such as tuberculosis, fungal infections, or opportunistic pathogens. Pre-screening for latent TB is mandatory, and vigilance for new infections remains crucial throughout therapy.
- Infusion Reactions: During or shortly after an infusion, mild to severe reactions can occur. Symptoms include shortness of breath, chest pain, fever, or hives. Healthcare providers typically mitigate these risks by administering antihistamines or corticosteroids beforehand and closely monitoring the patient during the infusion.
- Autoimmune Phenomena: A rare potential effect of biologics is the induction of auto-antibody production, leading to lupus-like syndromes or demyelinating disorders. While uncommon, clinicians remain watchful for any unusual symptoms.
- Malignancy Risk: There has been debate around whether long-term TNF-α inhibitor use increases the risk of certain malignancies, such as lymphoma. Large patient registries for rheumatoid arthritis, inflammatory bowel disease, and psoriasis offer insights, suggesting that while any immunosuppression might carry a slight increased risk, absolute rates remain relatively low. Close collaboration with a rheumatologist and regular health check-ups are recommended.
Balancing Benefits Against Concerns
For a condition as severe as refractory scleritis, the possibility of preserving vision and preventing irreversible complications often outweighs the potential side effects. However, this balance is patient-specific. Individuals with uncontrolled comorbid conditions—like poorly managed diabetes, advanced cardiovascular disease, or an ongoing infection—need personalized consultations with their healthcare team to ascertain whether they can safely undergo infliximab therapy.
In clinical settings, close and continuous monitoring has become the norm. Patients receive regular check-ups, laboratory tests, and eye examinations to detect any warning signs early. By calibrating dosage schedules and staying vigilant about infections, clinicians often successfully navigate the risk-benefit equation, enabling patients to experience improved ocular health with minimal adverse events.
Understanding the Costs of Infliximab Therapy
The cost of infliximab can vary widely, influenced by insurance coverage, infusion center fees, and geographic location. In the United States, a single infusion may start at around \$1,000 to \$2,500 or more per dose for those without robust insurance. Some clinics provide package deals that encompass the drug itself, the infusion procedure, and routine blood tests, whereas others itemize each service. Patients seeking financial support can explore manufacturer assistance programs or philanthropic organizations that help offset costs for qualifying individuals.
Biologic therapies like infliximab represent a frontier of targeted treatment for individuals battling refractory scleritis. By honing in on TNF-α, infliximab can curb the intense inflammation at the heart of this vision-threatening condition. In clinical use, it has demonstrated the ability to reduce ocular pain, lessen reliance on steroids, and stabilize vision, offering hope to those who have not found relief in conventional treatments.
This article is intended for informational purposes only and does not substitute professional medical advice. Please consult a qualified ophthalmologist or rheumatologist to determine whether infliximab is suitable for your specific needs.
If you found this article helpful, we invite you to share it on Facebook, X (formerly Twitter), or your favorite social media platform. Your support can help others discover potentially life-changing information about managing complex inflammatory eye conditions.