and Health Recommendations
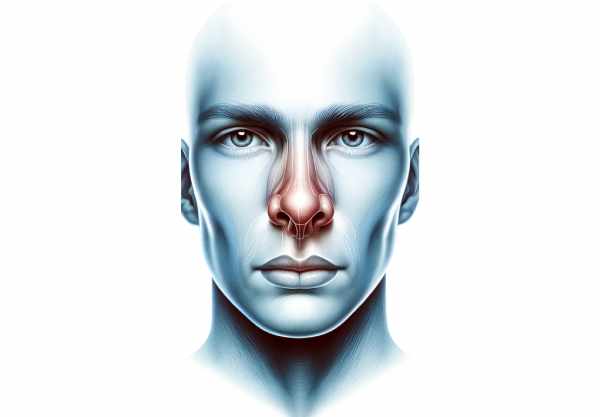
The nose is a vital organ that not only defines facial aesthetics but also plays a crucial role in breathing, olfaction, and overall health. It filters, warms, and humidifies incoming air, ensuring the respiratory system functions optimally. Additionally, the nose is central to our sense of smell, which influences taste and even memory. This comprehensive guide delves into the detailed anatomy of the nose, its diverse physiological functions, common disorders, advanced diagnostic methods, and a range of treatments and lifestyle practices designed to maintain and enhance nasal health.
Table of Contents
- Nasal Anatomy
- Physiological Functions
- Common Nasal Disorders
- Diagnostic Techniques
- Treatment Options
- Supplements for Nasal Health
- Lifestyle and Preventive Practices
- Trusted Resources
- Frequently Asked Questions
Nasal Anatomy
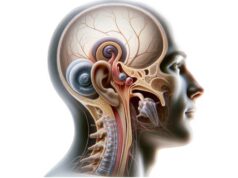
The anatomy of the nose is both complex and elegantly designed to support its numerous functions. Structurally, the nose is divided into two main parts: the external nose and the internal nasal cavity. Each compartment is composed of specialized tissues that work in harmony to facilitate breathing, olfaction, and air filtration.
External Nose
The external nose is the prominent, visible portion of the nose that defines much of our facial appearance. It comprises several key structures:
- Nasal Bones:
These two small, oblong bones form the bridge of the nose, providing structural support and contributing to the shape of the upper nose. - Cartilage:
Below the nasal bones, various cartilages—including the lateral, alar, and septal cartilages—give the lower part of the nose its shape and flexibility. The alar cartilages, for example, form the tip of the nose, while the septal cartilage supports the central portion. - Nasal Tip:
The nasal tip, composed primarily of alar cartilage, is the most anterior aspect of the nose. Its shape and projection significantly influence overall facial aesthetics. - Nostrils (Nares):
The nostrils are the external openings of the nasal cavity. They vary in shape and size between individuals and serve as the primary entry point for air into the respiratory system.
Internal Nasal Cavity
The internal nasal cavity is an intricate structure that serves multiple critical functions, including air filtration, humidification, and olfaction. It is divided by the nasal septum into two symmetrical halves.
- Nasal Septum:
The nasal septum is the wall that divides the nasal cavity into right and left sides. It is composed of both bone and cartilage, providing structural support while also directing airflow efficiently. A well-aligned septum is essential for balanced breathing. - Nasal Vestibule:
The anterior portion of the nasal cavity, known as the nasal vestibule, is lined with skin and hair follicles. These hairs (vibrissae) trap large particles and dust, preventing them from entering deeper into the respiratory tract. - Nasal Conchae (Turbinates):
The nasal cavity contains three pairs of bony projections—superior, middle, and inferior turbinates—that are covered by a mucous membrane. These structures increase the surface area of the nasal cavity, creating turbulence in the airflow. This turbulence enhances the warming, humidification, and filtering of inhaled air. - Nasal Mucosa:
Lining the entire nasal cavity is the nasal mucosa, which contains goblet cells that secrete mucus. This mucus traps particulate matter, pathogens, and allergens, while a rich network of blood vessels warms the air before it enters the lungs. - Olfactory Epithelium:
Located on the roof of the nasal cavity, the olfactory epithelium houses specialized olfactory receptor neurons. These receptors detect odor molecules dissolved in mucus and transmit signals to the brain via the olfactory nerve, enabling the sense of smell. - Paranasal Sinuses:
Surrounding the nasal cavity are the paranasal sinuses—air-filled cavities within the skull bones. The major sinuses include the maxillary, frontal, ethmoid, and sphenoid sinuses. They lighten the weight of the skull, contribute to voice resonance, and produce mucus that drains into the nasal cavity. - Nasopharynx:
The nasopharynx, located behind the nasal cavity, forms the upper part of the throat. It serves as an airway passage that connects the nasal cavity to the larynx and lungs, playing a critical role in breathing.
Blood Supply and Innervation
The nose is richly supplied with blood and nerve fibers to support its diverse functions:
- Blood Supply:
Multiple arteries, such as the anterior and posterior ethmoidal arteries (branches of the ophthalmic artery), the sphenopalatine artery (a branch of the maxillary artery), and branches of the facial artery, provide robust blood flow to the nasal tissues. This extensive vascular network ensures that the nasal mucosa remains warm and healthy. - Innervation:
Sensory innervation is primarily provided by branches of the trigeminal nerve (cranial nerve V). The ophthalmic division (V1) supplies the upper part of the nose, while the maxillary division (V2) innervates the lower part. The olfactory nerve (cranial nerve I) is responsible for transmitting smell signals from the olfactory epithelium to the brain.
Physiological Functions
The nose plays an indispensable role in several fundamental physiological processes, making it crucial to overall health and well-being. Its functions extend well beyond simple air passage.
Breathing and Airway Regulation
Breathing is the primary function of the nose, facilitating the movement of air into and out of the respiratory system.
- Airflow Management:
When air enters through the nostrils, it is channeled into the nasal cavity where the nasal septum and conchae regulate airflow. The turbulent flow created by the turbinates allows maximum contact with the nasal mucosa, optimizing the warming, humidification, and filtering of air before it reaches the lungs. - Temperature and Humidity Control:
The rich vascular supply of the nasal mucosa warms incoming air, while moisture from the mucus increases humidity. This is critical for protecting the delicate tissues of the lower respiratory tract and ensuring efficient gas exchange.
Olfaction (Sense of Smell)
The nose’s role in olfaction is complex and essential:
- Odor Detection:
The olfactory epithelium houses receptor neurons equipped with cilia that capture odor molecules dissolved in mucus. These receptors initiate a signal transduction cascade that sends electrical impulses via the olfactory nerve to the olfactory bulb. - Neural Processing:
The olfactory bulb processes these signals and relays them to various brain regions, including the olfactory cortex, hippocampus, and amygdala. This network not only enables the perception of different smells but also connects odors to memories and emotions.
Air Filtration and Defense
The nose acts as a first-line defense mechanism by filtering and trapping potentially harmful particles and pathogens.
- Nasal Hairs and Mucus:
The hairs in the nasal vestibule capture larger particles, while the mucus secreted by goblet cells ensnares smaller particles, bacteria, and viruses. - Mucociliary Clearance:
Cilia on the surface of the nasal epithelial cells beat in a coordinated manner, moving mucus and trapped particles toward the pharynx, where they are swallowed and neutralized by stomach acids. This process is critical in preventing respiratory infections.
Humidification and Moisturization
The nose ensures that the air we breathe is appropriately humidified before it reaches the delicate tissues of the lungs.
- Moisture Addition:
As air passes over the moist nasal mucosa, it absorbs water vapor, increasing its humidity. This not only protects the respiratory tract from drying out but also aids in the optimal functioning of the mucociliary clearance system.
Vocal Resonance and Sound Modification
The nasal cavity and sinuses significantly contribute to the quality of our voice.
- Resonance:
During speech, sound waves produced by the vocal cords resonate within the nasal cavity and paranasal sinuses. This resonance shapes the tone, timbre, and projection of the voice. Conditions that block or alter the nasal passages, such as congestion or sinusitis, can adversely affect vocal quality.
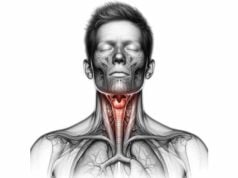
Pressure Regulation in the Ear
The nose also plays a subtle yet important role in regulating ear pressure.
- Eustachian Tube Function:
The nasopharynx connects to the middle ear via the Eustachian tube, which helps equalize air pressure on both sides of the eardrum. Proper functioning of this tube is essential for maintaining normal hearing and balance.
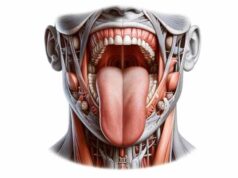
Integration of Taste and Smell
Though taste is primarily mediated by the tongue, the sense of smell is crucial for the full perception of flavor.
- Flavor Perception:
Olfactory receptors in the nose detect volatile compounds that contribute to the overall flavor of foods and beverages. This integration of smell and taste enriches our dining experiences and influences our dietary preferences.
Common Nasal Disorders
Due to its central role in respiration and olfaction, the nose is vulnerable to various disorders that can affect both its structure and function. Early recognition and proper management of these conditions are essential for maintaining overall nasal health.
Rhinitis
Rhinitis is an inflammation of the nasal mucosa that can result from allergic reactions, infections, or irritants.
Allergic Rhinitis
- Causes and Symptoms:
Triggered by allergens such as pollen, dust mites, mold, and pet dander, allergic rhinitis leads to sneezing, nasal congestion, itching, and watery eyes. It is the classic “hay fever” response. - Treatment:
Management includes antihistamines, decongestants, nasal corticosteroids, and allergen avoidance. Immunotherapy may be considered for long-term relief.
Non-Allergic Rhinitis
- Triggers and Characteristics:
Unlike allergic rhinitis, non-allergic rhinitis is not immune-mediated. It can be caused by irritants such as smoke, strong odors, or environmental changes. Symptoms mimic allergic rhinitis but without the allergen-specific immune response. - Management:
Avoiding triggers, using saline nasal sprays, and occasionally employing nasal corticosteroids help control symptoms.
Infectious Rhinitis
- Etiology and Manifestations:
Often caused by viruses (like rhinovirus) or bacteria, infectious rhinitis (the common cold) leads to a runny, congested nose, sore throat, and cough. - Treatment:
Supportive care, including hydration, rest, and over-the-counter medications, is typically recommended.
Sinusitis
Sinusitis is the inflammation or infection of the paranasal sinuses and can be acute, chronic, or recurrent.
Acute Sinusitis
- Presentation:
Typically follows a viral infection and lasts for a few weeks. Symptoms include facial pain or pressure, nasal congestion, purulent nasal discharge, and reduced sense of smell. - Management:
Treatment may involve decongestants, nasal corticosteroids, saline irrigation, and, in cases of bacterial infection, antibiotics.
Chronic Sinusitis
- Characteristics:
Lasting more than 12 weeks, chronic sinusitis is often linked to ongoing inflammation, structural abnormalities, or allergies. It presents with persistent nasal congestion, facial pain, and a diminished sense of smell. - Treatment:
A combination of medications (antibiotics, steroids, saline rinses) and, in refractory cases, surgical interventions such as Functional Endoscopic Sinus Surgery (FESS) may be necessary.
Nasal Polyps
Nasal polyps are benign, soft growths that develop on the lining of the nasal passages or sinuses due to chronic inflammation.
- Symptoms:
They may cause nasal obstruction, a reduced sense of smell, and recurring sinus infections. - Treatment:
Nasal corticosteroids, oral steroids, and in some cases, surgical removal are used to manage nasal polyps.
Deviated Septum
A deviated septum is a displacement of the nasal septum, which can result from congenital factors or trauma.
- Symptoms:
A deviated septum often causes nasal congestion, difficulty breathing, frequent nosebleeds, and snoring. - Treatment:
Management ranges from decongestants and nasal strips to surgical correction (septoplasty) for significant deviations.
Epistaxis (Nosebleeds)
Nosebleeds, or epistaxis, can range from mild to severe and are often caused by dryness, trauma, or underlying medical conditions.
- Types:
Anterior nosebleeds (from the front of the nasal septum) are common and usually minor, while posterior nosebleeds (from deeper within the nasal cavity) can be more serious. - Treatment:
Initial management includes applying pressure, using nasal packing, and, if necessary, cauterization. Underlying causes must also be addressed.
Olfactory Disorders
Disorders of smell can have a significant impact on quality of life and may be associated with nasal conditions or neurological diseases.
- Anosmia and Hyposmia:
Loss (anosmia) or reduction (hyposmia) in the sense of smell may result from nasal obstructions, infections, head injuries, or neurodegenerative diseases. - Parosmia:
A distortion of the sense of smell, often following infections or trauma. - Management:
Treatment focuses on addressing the underlying cause, which may involve medications, olfactory training, or surgical intervention if structural abnormalities are present.
Nasal Fractures
Due to its prominent position, the nose is prone to fractures resulting from trauma.
- Symptoms:
Pain, swelling, bruising, nasal deformity, and difficulty breathing. - Treatment:
Management includes pain relief, reduction (realignment) of the fracture, and, if necessary, surgical correction to restore function and appearance.
Tumors
Nasal tumors can be benign or malignant.
- Benign Tumors:
Such as papillomas and hemangiomas, which can cause obstruction and recurrent infections. - Malignant Tumors:
Although rare, cancers like squamous cell carcinoma and adenocarcinoma require aggressive treatment with surgery, radiation, and chemotherapy. - Management:
Early detection through imaging and biopsy is crucial for effective treatment.
Diagnostic Techniques for Nasal Conditions
Accurate diagnosis of nasal conditions is essential for effective treatment. A variety of diagnostic tools and methods are available, each offering unique insights into the structure and function of the nasal cavity.
Physical Examination
- Visual Inspection:
A comprehensive physical examination begins with inspecting the external nose for asymmetries, deformities, or signs of trauma. - Palpation:
Gently feeling the nasal structures helps detect tenderness, swelling, or masses. - Rhinoscopy:
A nasal speculum and light source allow clinicians to examine the nasal vestibule and anterior nasal septum for abnormalities such as polyps or excessive mucus.
Nasal Endoscopy
Nasal endoscopy provides a detailed view of the internal nasal cavity and nasopharynx.
- Procedure:
Using a flexible or rigid endoscope equipped with a camera and light, clinicians can visualize deeper regions, assess the condition of the mucosa, and identify obstructions or lesions. - Applications:
It is invaluable in diagnosing chronic sinusitis, nasal polyps, and structural abnormalities.
Imaging Studies
Imaging plays a critical role in assessing nasal and sinus anatomy.
- Computed Tomography (CT) Scan:
CT scans provide detailed cross-sectional images of the nasal cavity and paranasal sinuses. They are the gold standard for diagnosing sinusitis, structural abnormalities, and planning surgical interventions. - Magnetic Resonance Imaging (MRI):
MRI is used for soft tissue evaluation, particularly useful for assessing tumors, inflammatory conditions, and complications involving the orbit or intracranial structures. - X-rays:
Although less common now, plain X-rays can be useful for identifying nasal bone fractures or gross abnormalities.
Laboratory Tests
Laboratory assessments are useful for diagnosing infectious or allergic causes of nasal symptoms.
- Microbiological Cultures:
Swabs from nasal secretions can identify bacterial, viral, or fungal pathogens. - Allergy Testing:
Skin prick tests and serum IgE measurements help identify allergens responsible for allergic rhinitis. - Blood Tests:
These tests can assess inflammatory markers, immune function, and rule out systemic conditions affecting nasal health.
Functional and Specialized Tests
- Olfactory Testing:
Standardized tests, such as the University of Pennsylvania Smell Identification Test (UPSIT) or Sniffin’ Sticks, evaluate the sense of smell and help diagnose olfactory disorders. - Peak Nasal Inspiratory Flow (PNIF):
This simple test measures the maximum airflow through the nose and is useful in quantifying nasal obstruction. - Acoustic Rhinometry:
By using sound waves to map the nasal cavity’s cross-sectional area, this technique provides quantitative data on nasal patency and can help assess the impact of treatments.
Biopsy
When suspicious lesions or tumors are identified, a biopsy may be performed.
- Procedure:
A small tissue sample is taken from the nasal mucosa or a lesion and examined histopathologically to diagnose malignancies or confirm inflammatory conditions. - Importance:
Biopsy is crucial for early detection of nasal cancers and other serious pathologies.
Treatment Options for Nasal Conditions
Treatment for nasal conditions depends on the underlying cause, severity, and patient-specific factors. Approaches range from conservative medical management to surgical interventions and innovative therapies.
Medical Management
Medications
- Decongestants:
Oral and topical decongestants (e.g., pseudoephedrine, phenylephrine) help reduce nasal congestion by constricting blood vessels. However, prolonged use of nasal sprays can lead to rebound congestion. - Antihistamines:
Agents like cetirizine, loratadine, and fexofenadine block histamine receptors and alleviate symptoms of allergic rhinitis such as sneezing, itching, and a runny nose. - Nasal Corticosteroids:
Intranasal corticosteroids (e.g., fluticasone, mometasone) are highly effective at reducing inflammation in allergic and non-allergic rhinitis, as well as in chronic sinusitis. - Antibiotics:
When bacterial infections are identified, appropriate antibiotics (e.g., amoxicillin-clavulanate, doxycycline) are prescribed. - Antifungals:
For fungal infections of the sinuses or nasal cavity, topical or systemic antifungal agents (such as itraconazole) may be used. - Saline Irrigation:
Regular use of isotonic or hypertonic saline nasal rinses helps clear mucus, allergens, and pathogens, improving nasal patency and comfort.
Immunotherapy
For patients with allergic rhinitis, allergen-specific immunotherapy (AIT) may be employed.
- Methods:
AIT is administered as subcutaneous injections (SCIT) or sublingual tablets/drops (SLIT) and involves gradually increasing exposure to allergens, thereby desensitizing the immune response.
Surgical Interventions
Surgery is indicated when structural abnormalities or persistent disease does not respond to medical management.
Functional Endoscopic Sinus Surgery (FESS)
- Procedure:
FESS uses an endoscope to visualize and remove obstructions such as nasal polyps or inflamed tissue from the sinus cavities. This surgery aims to restore normal sinus drainage and function. - Indications:
Chronic sinusitis, nasal polyposis, and certain cases of deviated septum may benefit from FESS.
Septoplasty
- Purpose:
Septoplasty corrects a deviated nasal septum to improve airflow and alleviate nasal obstruction. - Outcome:
Successful septoplasty can reduce symptoms of nasal congestion and associated complications like snoring and frequent nosebleeds.
Turbinate Reduction
- Technique:
Enlarged nasal turbinates can be reduced using methods such as radiofrequency ablation or submucosal resection. - Benefits:
Reducing turbinate size improves airflow, decreases nasal congestion, and enhances overall breathing.
Polypectomy
- Procedure:
Surgical removal of nasal polyps, usually performed endoscopically, can relieve obstruction and reduce the recurrence of sinus infections. - Follow-up:
Postoperative care often includes corticosteroid therapy to minimize inflammation and prevent polyp recurrence.
Rhinoplasty
- Scope:
Beyond cosmetic improvements, functional rhinoplasty addresses structural issues that affect nasal airflow. - Techniques:
Corrective procedures may involve reshaping the nasal bones and cartilages to enhance both appearance and function.
Innovative and Minimally Invasive Therapies
Biological Therapies
- Biologics:
Monoclonal antibodies, such as dupilumab (targeting the IL-4 receptor), have shown promise in treating chronic rhinosinusitis with nasal polyps by reducing inflammation and polyp size. - Impact:
These agents offer targeted treatment with potentially fewer side effects than conventional systemic medications.
Balloon Sinuplasty
- Description:
Balloon sinuplasty is a minimally invasive technique that involves the insertion of a small balloon catheter into the sinus ostia, which is then inflated to dilate the openings. - Advantages:
This procedure can improve sinus drainage without the need for extensive tissue removal, leading to a faster recovery.
Cryotherapy and Phototherapy
- Cryotherapy:
Cryoablation uses cold temperatures to reduce inflammation and treat chronic rhinitis by targeting specific nerves that contribute to congestion. - Phototherapy:
Intranasal phototherapy devices emit specific wavelengths of light that reduce mucosal inflammation and alleviate symptoms of allergic rhinitis.
Supplements for Nasal Health
Nutritional and herbal supplements can support nasal health by enhancing immune function, reducing inflammation, and protecting mucosal integrity.
Vitamins and Minerals
- Vitamin C:
Known for its immune-boosting and antioxidant properties, vitamin C helps protect the nasal mucosa from oxidative damage and reduces the severity of respiratory infections. - Vitamin D:
Adequate vitamin D levels are associated with a reduced risk of respiratory infections and may help alleviate chronic rhinitis and sinusitis. - Vitamin A:
Essential for maintaining the integrity of mucosal surfaces, vitamin A supports the nasal epithelium in trapping pathogens and allergens. - Zinc:
Zinc is crucial for cellular repair and immune function. A deficiency in zinc can impair nasal mucosal health and increase susceptibility to infections.
Herbal Supplements
- Echinacea:
Widely used for its immune-enhancing properties, echinacea may reduce the frequency and severity of colds, thereby protecting nasal passages. - Butterbur:
Butterbur exhibits anti-inflammatory effects that can help alleviate symptoms of allergic rhinitis, reducing nasal congestion and sneezing. - Quercetin:
A natural flavonoid with antihistamine and anti-inflammatory effects, quercetin helps stabilize mast cells and lower histamine release, alleviating allergic symptoms.
Enzymes
- Bromelain:
Derived from pineapples, bromelain has potent anti-inflammatory properties and can help reduce nasal congestion and mucus viscosity, facilitating easier breathing.
Hormonal and Miscellaneous Supplements
- Melatonin:
Beyond its role in sleep regulation, melatonin’s antioxidant properties may protect nasal tissues from oxidative stress and enhance overall immune function. - Omega-3 Fatty Acids:
These essential fatty acids, found in fish oil and flaxseed, have anti-inflammatory properties that can help manage chronic nasal inflammation and allergic rhinitis. - N-acetylcysteine (NAC):
NAC helps thin mucus and reduce inflammation in the nasal passages, making it a useful supplement for chronic sinusitis and rhinitis.
Probiotics
Probiotics contribute to a balanced microbiome throughout the body, including the nasal passages. A healthy balance of bacteria supports immune defenses and may lower the risk of respiratory infections.
Lifestyle and Preventive Practices
Maintaining nasal health requires a proactive approach that integrates good hygiene, environmental awareness, and healthy living practices.
- Practice Good Hygiene:
Regular handwashing and avoiding touching the face can help prevent the spread of pathogens that cause nasal infections. - Stay Hydrated:
Drinking plenty of water keeps the mucous membranes moist and supports the natural clearance of mucus and debris. - Use a Humidifier:
Especially in dry climates or during winter months, a humidifier can maintain optimal moisture levels in the air, preventing dryness and irritation in the nasal passages. - Perform Nasal Irrigation:
Saline nasal rinses help remove allergens, irritants, and excess mucus, reducing inflammation and improving breathing. - Avoid Irritants:
Minimize exposure to pollutants, cigarette smoke, strong odors, and other environmental irritants that can trigger or exacerbate nasal inflammation. - Maintain a Balanced Diet:
A nutrient-rich diet supports immune function and overall health. Foods high in vitamins, antioxidants, and anti-inflammatory compounds contribute to the health of nasal tissues. - Manage Allergies:
Identify and avoid allergens through proper testing, and follow a tailored treatment plan which may include antihistamines, nasal corticosteroids, or immunotherapy. - Exercise Regularly:
Regular physical activity boosts circulation and strengthens the immune system, indirectly promoting nasal health. - Quit Smoking:
Smoking damages the nasal mucosa, impairs mucociliary clearance, and increases the risk of chronic rhinitis and sinusitis. - Keep Up with Vaccinations:
Staying current with immunizations, such as the seasonal flu shot, helps prevent respiratory infections that can compromise nasal health. - Reduce Stress:
Stress management techniques like meditation, yoga, and deep breathing exercises can reduce the frequency of stress-induced nasal symptoms, such as non-allergic rhinitis.
Trusted Resources
For those seeking more information on nasal health, numerous reliable resources are available across various platforms.
Recommended Books
- “Rhinology and Endoscopic Skull Base Surgery: Clinical Reference Guide” by Raj Sindwani, MD:
An in-depth resource covering the anatomy, physiology, and surgical management of nasal and sinus conditions. - “Nasal Physiology and Pathophysiology of Nasal Disorders” by Özlem Önerci, MD:
This book offers comprehensive insights into nasal functions and common disorders, blending clinical practice with research findings. - “Nose and Paranasal Sinuses: A Practical Guide” by Paolo Castelnuovo, MD, and Daniele Marchioni, MD:
A practical manual that outlines diagnostic techniques, medical and surgical treatments, and advancements in managing nasal and sinus conditions.
Academic Journals
- The American Journal of Rhinology & Allergy:
This peer-reviewed journal publishes clinical and basic research articles focused on nasal and sinus conditions, including innovative treatment methods. - International Forum of Allergy & Rhinology:
Featuring the latest research on rhinology and allergy, this journal provides valuable insights into diagnostic methods and therapeutic advances.
Mobile Applications
- Rhinology Toolbox:
An app for healthcare professionals offering tools, calculators, guidelines, and reference materials to assist in diagnosing and managing nasal conditions. - Allergy Tracker:
This app helps individuals monitor allergy symptoms, access real-time pollen counts, and manage medications to mitigate allergic rhinitis. - Nasal Health Guide:
A resource offering practical tips on nasal hygiene, advice on nasal irrigation, and strategies for managing common nasal conditions.
Frequently Asked Questions
What are the primary functions of the nose?
The nose is essential for breathing by filtering, warming, and humidifying air. It also plays a crucial role in olfaction (smell), contributes to vocal resonance, and helps defend against pathogens through mucociliary clearance.
How does the nasal cavity filter and humidify air?
As air passes through the nasal cavity, the nasal hairs and mucosa trap particles and allergens. The rich blood supply warms the air, while mucus and moisture add humidity, ensuring that the air reaching the lungs is properly conditioned.
What are common causes of allergic rhinitis?
Allergic rhinitis is primarily caused by exposure to allergens such as pollen, dust mites, pet dander, and mold. The immune response to these allergens triggers histamine release, leading to symptoms like congestion, sneezing, and itching.
When is surgical intervention necessary for nasal conditions?
Surgical treatments, such as FESS, septoplasty, or turbinate reduction, are considered when medical management fails to relieve symptoms, when structural abnormalities impede nasal function, or when complications such as chronic sinusitis or severe nasal obstruction occur.
How can I improve nasal health through lifestyle changes?
Maintaining good nasal hygiene, staying hydrated, using saline irrigation, avoiding irritants, managing allergies, and ensuring a balanced diet rich in vitamins and antioxidants are all effective ways to support nasal health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider regarding any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to maintain optimal nasal health.