Sweat glands are specialized structures of the skin that play a crucial role in maintaining body temperature, excreting waste products, and contributing to the skin’s immune defense. These microscopic glands, found throughout the human body, are essential for thermoregulation and overall homeostasis. By producing sweat, they enable the body to cool itself through evaporation while also serving as a medium for eliminating metabolic byproducts. This guide will explore in depth the complex anatomy and diverse functions of sweat glands, the disorders that can affect them, modern diagnostic methods, and the range of treatments and lifestyle strategies available to ensure optimal sweat gland and skin health.
Table of Contents
- Anatomical Overview
- Eccrine Glands
- Apocrine Glands
- Modified Sweat Glands
- Innervation & Blood Supply
- Development & Aging
- Functional Roles
- Sweat Gland Disorders
- Diagnostic Techniques
- Treatment Strategies
- Supplemental & Nutritional Support
- Lifestyle and Preventive Practices
- Trusted Resources
- Frequently Asked Questions
- Disclaimer & Sharing
Anatomical Overview of Sweat Glands
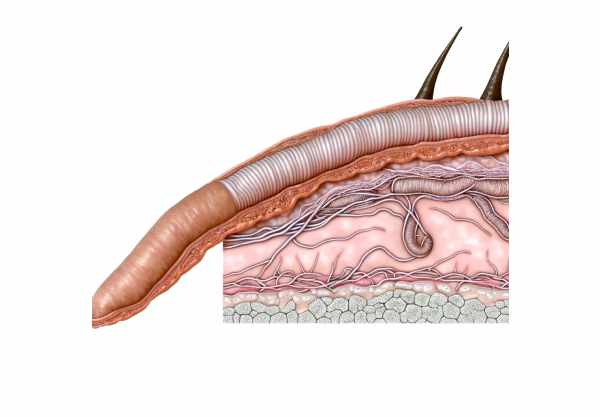
Sweat glands are vital components of the integumentary system, intricately embedded within the dermis of the skin. They are distributed across almost all body surfaces, with varying densities depending on the region. There are two main types of sweat glands—eccrine and apocrine—which differ in structure, location, and function. Eccrine glands are the most common and are responsible for regulating body temperature through the secretion of a watery sweat. In contrast, apocrine glands, which are concentrated in areas such as the armpits and groin, secrete a thicker fluid that plays roles in pheromone release and social signaling. Additionally, several modified sweat glands, including those found in the ear canal and near the eyes, contribute to specialized functions such as earwax production and tear film stability.
Eccrine Sweat Glands
Eccrine sweat glands are the most abundant type of sweat gland in the human body. They are distributed over nearly all skin surfaces and are essential for thermoregulation.
Structure and Location
Eccrine glands are simple, coiled tubular structures located deep in the dermis. Their secretory portions are responsible for producing sweat, while their ducts extend upward through the epidermis to open at the skin surface via tiny pores. They are especially concentrated on the palms, soles, and forehead, areas where effective temperature regulation is critical.
Cellular Composition
- Secretory Cells:
The secretory portion is lined with cells that contain abundant mitochondria and specialized transporters. These cells actively secrete a watery solution containing water, electrolytes, and small amounts of metabolic waste. - Myoepithelial Cells:
Surrounding the secretory portion are myoepithelial cells that contract to expel sweat from the gland. Their rhythmic contraction is crucial during heat stress.
Function
The primary role of eccrine sweat glands is thermoregulation. When the body’s internal temperature rises—due to exercise or high ambient temperatures—the hypothalamus signals these glands to produce sweat. The evaporation of sweat from the skin surface dissipates heat and cools the body. This mechanism is essential to prevent hyperthermia and maintain a stable internal environment.
Apocrine Sweat Glands
Apocrine sweat glands are less numerous than eccrine glands and are found primarily in specific regions such as the armpits, groin, and around the nipples. They differ from eccrine glands in both structure and function.
Structure and Location
Apocrine glands are larger and are located deeper in the dermis or subcutaneous tissue. Unlike eccrine glands, their ducts do not open directly onto the skin surface; instead, they open into hair follicles. This anatomical feature influences the characteristics of their secretions.
Cellular Composition
- Secretory Cells:
The cells within apocrine glands produce a thicker, milky secretion that contains proteins, lipids, and steroids. Initially, this secretion is odorless, but when it interacts with skin bacteria, it can develop a characteristic body odor. - Myoepithelial Cells:
Similar to eccrine glands, apocrine glands are surrounded by myoepithelial cells that aid in the expulsion of secretions through their contractile action.
Function
Apocrine sweat glands are primarily involved in scent release and social communication. Their secretions contain pheromones—chemical signals that can influence social and sexual behavior. Although they play a less critical role in thermoregulation compared to eccrine glands, their activity increases during puberty under hormonal influence, contributing to individual body odor and aiding in interpersonal communication.
Modified Sweat Glands
In addition to the typical eccrine and apocrine glands, the human body features several modified sweat glands, each specialized for unique functions.
Ceruminous Glands
- Location:
Found in the external auditory canal. - Function:
Produce earwax (cerumen), which lubricates the ear canal, traps dust and debris, and provides antimicrobial protection.
Mammary Glands
- Location:
Located in the breasts. - Function:
Highly specialized modified apocrine glands that produce milk to nourish infants. Their activity is hormonally regulated, especially during pregnancy and lactation.
Ciliary Glands
- Location:
Situated near the eyelids. - Function:
Secrete a lipid-rich substance that contributes to the tear film, aiding in lubrication and protection of the eye surface.
Innervation & Blood Supply
Sweat glands are supported by an extensive network of nerves and blood vessels, which are critical for their function.
Neural Control
- Sympathetic Nervous System:
Sweat glands are primarily regulated by the sympathetic nervous system. Uniquely, eccrine glands are stimulated by cholinergic fibers that release acetylcholine, despite the majority of sympathetic nerves typically releasing norepinephrine. This cholinergic activation triggers sweat secretion. - Adrenergic and Cholinergic Fibers:
While eccrine glands are mainly influenced by cholinergic stimulation, apocrine glands receive both adrenergic and cholinergic signals, contributing to their distinct functional patterns.
Vascular Support
Sweat glands are richly vascularized. A dense capillary network surrounds them, providing a steady supply of nutrients and oxygen necessary for the production and transport of sweat. This robust blood supply also aids in the removal of metabolic waste products from the glandular cells.
Development & Aging of Sweat Glands
The formation and aging of sweat glands follow a well-defined developmental process, which has implications for their function throughout life.
Fetal Development
- Eccrine Glands:
Begin to form around the third month of fetal development and are usually fully functional by birth. Their early development is crucial for neonatal thermoregulation. - Apocrine Glands:
Develop later in fetal life and remain dormant until puberty, when hormonal changes activate them, leading to the development of characteristic body odor.
Postnatal Maturation and Aging
- Functional Maturation:
After birth, sweat glands continue to mature, with eccrine glands taking on their full thermoregulatory role. - Aging Effects:
As individuals age, the number and functionality of sweat glands tend to decline. This reduction can impact thermoregulation and the skin’s ability to excrete metabolic waste, making older adults more susceptible to heat stress and skin dryness.
Functional Roles of Sweat Glands
Sweat glands serve multiple critical functions that contribute to overall homeostasis and skin health.
Thermoregulation
- Heat Dissipation:
Eccrine sweat glands are primarily responsible for cooling the body. When core body temperature rises, the hypothalamus signals these glands to secrete sweat. As the water in the sweat evaporates from the skin’s surface, it absorbs heat, lowering the body temperature. - Evaporative Cooling:
The effectiveness of sweating depends on factors such as ambient temperature, humidity, and individual physiology. Rapid evaporation is essential for efficient heat loss.
Excretion of Metabolic Waste
- Removal of Solutes:
In addition to water, sweat contains electrolytes (sodium, chloride, potassium) and trace amounts of metabolic waste products such as urea and ammonia. This excretion helps maintain electrolyte balance and reduce the burden on the kidneys. - Detoxification:
The elimination of waste products through sweat contributes to overall detoxification, although the kidneys are the primary organs responsible for this function.
Skin Hydration and Protection
- Moisturizing the Skin:
Sweat helps maintain skin hydration by providing moisture. The slight acidity of sweat contributes to the formation of the acid mantle—a protective film that deters the growth of harmful bacteria and fungi. - Barrier Function:
By keeping the skin moist and maintaining an optimal pH, sweat supports the skin’s barrier function, preventing external irritants and pathogens from penetrating.
Pheromone Release
- Social Communication:
Apocrine sweat glands secrete pheromones that are involved in social and sexual communication. These chemical signals can influence interpersonal interactions and may play a role in attraction. - Odor Formation:
Although apocrine sweat is initially odorless, its interaction with skin bacteria produces characteristic body odors that can signal individual identity.
Immune Defense
- Antimicrobial Activity:
Sweat contains antimicrobial peptides, such as dermcidin and defensins, which help inhibit the growth of bacteria, viruses, and fungi on the skin. This function is vital for protecting the body from infections. - Enhancing Immune Surveillance:
By facilitating the constant flow of sweat over the skin, these peptides help maintain a sterile environment and prevent colonization by harmful microorganisms.
Sweat Gland Disorders
Sweat glands can be affected by various disorders, ranging from conditions that result in excessive sweating to those that impair sweat production. Understanding these conditions is essential for proper diagnosis and treatment.
Hyperhidrosis
Hyperhidrosis is characterized by excessive sweating beyond what is required for thermoregulation. It can be either focal (affecting specific areas like the palms, soles, or underarms) or generalized.
- Primary Hyperhidrosis:
Often develops during childhood or adolescence and is thought to result from overactivity of the sympathetic nervous system. - Secondary Hyperhidrosis:
Occurs as a result of underlying conditions such as hyperthyroidism, diabetes, infections, or as a side effect of medications.
Symptoms:
Excessive sweating that can interfere with daily activities, cause skin irritation, and lead to social and emotional distress.
Treatment:
Includes topical antiperspirants, oral anticholinergics, Botox injections, iontophoresis, and, in severe cases, surgical interventions such as sympathectomy.
Anhidrosis and Hypohidrosis
Anhidrosis is the absence of sweating, while hypohidrosis refers to reduced sweating. Both conditions impair the body’s ability to regulate temperature and can lead to heat intolerance.
- Causes:
Can result from skin damage (burns, infections), neurological disorders (autonomic neuropathy), genetic conditions, medications, or systemic diseases such as diabetes. - Symptoms:
Reduced or absent sweat production, heat intolerance, dizziness, and an increased risk of heatstroke.
Treatment:
Focuses on managing the underlying cause, staying cool with appropriate clothing and cooling devices, and ensuring adequate hydration.
Miliaria (Heat Rash)
Miliaria, commonly known as heat rash or prickly heat, occurs when sweat ducts become blocked, leading to sweat leakage into the skin.
- Types:
- Miliaria Crystallina: Characterized by clear, superficial blisters.
- Miliaria Rubra: Presents with red, itchy papules.
- Miliaria Profunda: Involves deeper, flesh-colored lesions.
- Symptoms:
Itching, prickling, and the formation of small bumps or blisters in areas of excessive sweating. - Treatment:
Involves cooling the skin, wearing loose clothing, and applying topical treatments such as calamine lotion or hydrocortisone.
Hidradenitis Suppurativa
Hidradenitis suppurativa (HS) is a chronic inflammatory condition affecting apocrine sweat glands, primarily in the armpits, groin, and under the breasts.
- Causes:
The exact cause is unclear but is believed to involve a combination of genetic, hormonal, and environmental factors. - Symptoms:
Painful, recurrent lumps, abscesses, and sinus tract formation that can lead to scarring and significant discomfort. - Treatment:
Options include antibiotics, hormonal therapies, immunosuppressants, biologics, and in severe cases, surgical removal of affected tissue.
Bromhidrosis
Bromhidrosis refers to unpleasant body odor resulting from the bacterial breakdown of sweat, particularly from the apocrine glands.
- Causes:
Poor hygiene, diet, infections, and certain medical conditions (e.g., metabolic disorders) can contribute to bromhidrosis. - Symptoms:
Noticeable and often distressing body odor that may affect personal and social interactions. - Treatment:
Emphasizes improved hygiene practices, antibacterial treatments, and lifestyle modifications to minimize odor.
Fox-Fordyce Disease
Fox-Fordyce disease is a rare, chronic skin disorder affecting apocrine sweat glands, primarily seen in post-pubertal women.
- Symptoms:
Itchy, small, skin-colored or red papules typically found in the underarms, groin, and around the nipples. - Treatment:
Options include topical retinoids, corticosteroids, and laser therapy to reduce symptoms and improve skin appearance.
Eccrine Porocarcinoma
Eccrine porocarcinoma is a rare malignant tumor arising from the eccrine sweat glands.
- Causes:
The exact etiology is unknown; however, factors such as age, sun exposure, and immunosuppression may play a role. - Symptoms:
Slow-growing nodules that may ulcerate, bleed, or become painful. - Treatment:
Primarily involves surgical excision, with adjuvant radiation or chemotherapy considered depending on the tumor stage and spread.
Sweat Gland Cysts
Cysts in the sweat glands can develop due to blocked ducts or localized trauma.
- Symptoms:
Painless lumps or swellings that may become infected or inflamed. - Treatment:
Observation, drainage, or surgical removal if the cyst becomes symptomatic or recurrent.
Diagnostic Techniques for Sweat Gland Disorders
Accurate diagnosis of sweat gland disorders involves a combination of clinical evaluation, laboratory tests, and imaging studies. These methods help pinpoint the underlying cause and guide appropriate treatment.
Medical History and Physical Examination
- Medical History:
Detailed questioning regarding the onset, duration, and triggers of excessive or diminished sweating is essential. Family history and associated symptoms, such as skin lesions or systemic illness, are also evaluated. - Physical Examination:
A comprehensive skin examination is performed to assess the distribution and severity of sweating, detect signs of inflammation, and identify any associated skin changes or lesions.
Laboratory Tests
- Blood Tests:
Used to identify underlying systemic conditions such as hyperthyroidism or diabetes that may contribute to abnormal sweating patterns. - Sweat Tests:
- Quantitative Sudomotor Axon Reflex Test (QSART): Assesses the function of the autonomic nerves that control sweating by measuring sweat production in response to electrical stimulation.
- Microbiological Tests:
Skin swabs and cultures can identify bacterial or fungal infections that may influence sweat gland function.
Imaging Studies
- Ultrasound:
Non-invasive imaging used to visualize the structure of sweat glands and detect abnormalities such as cysts or tumors. - Magnetic Resonance Imaging (MRI):
Provides high-resolution images of soft tissue structures, useful for evaluating deep-seated sweat gland lesions. - Computed Tomography (CT) Scan:
Offers detailed cross-sectional images to help detect structural abnormalities, particularly in cases where sweat gland tumors are suspected. - Positron Emission Tomography (PET) Scan:
Used to identify areas of increased metabolic activity that may indicate malignancy.
Biopsy and Histopathology
- Skin Biopsy:
A small sample of tissue is removed for microscopic examination to confirm inflammatory conditions, neoplasms, or other pathologies affecting sweat glands. - Histopathological Analysis:
Provides definitive diagnosis by examining cellular architecture, inflammation, and other tissue changes.
Functional and Autonomic Tests
- Thermoregulatory Sweat Test (TST):
Assesses the distribution and functionality of sweat production by applying a powder that changes color when in contact with sweat, mapping areas of hyperhidrosis or anhidrosis. - Starch-Iodine Test:
Utilizes an iodine solution and starch powder to highlight areas of excessive or reduced sweating by a color change. - Evaporimetry:
Measures the rate of water vapor loss from the skin, offering a quantitative assessment of sweat production. - Autonomic Function Tests:
Include the tilt table test and heart rate variability (HRV) analysis to evaluate the overall function of the autonomic nervous system.
Genetic Testing
- Genetic Analysis:
In cases of congenital disorders affecting sweat gland function, genetic testing can identify mutations responsible for conditions like congenital anhidrosis.
Treatment Strategies and Management
The management of sweat gland disorders varies widely based on the condition, severity, and underlying causes. Treatment plans are often multidisciplinary, combining medical therapies with lifestyle modifications.
Medications
- Antiperspirants:
Aluminum chloride-based antiperspirants reduce excessive sweating by blocking sweat ducts. Both over-the-counter and prescription-strength formulas are available. - Anticholinergic Agents:
Oral medications such as glycopyrrolate and oxybutynin inhibit the neurotransmitter acetylcholine, reducing sweat production. They are particularly useful in treating generalized hyperhidrosis. - Topical Treatments:
Topical anticholinergics like glycopyrronium tosylate (Qbrexza) are applied directly to the skin to control underarm sweating. - Antibiotics and Anti-inflammatories:
For conditions like hidradenitis suppurativa, antibiotics (e.g., clindamycin, tetracycline) and corticosteroids reduce inflammation and control infection.
Botulinum Toxin Injections
- Mechanism:
Botulinum toxin (Botox) injections temporarily block the release of acetylcholine, significantly reducing sweat production in the treated area. - Procedure:
The toxin is injected into the skin (commonly the underarms, palms, or soles), with effects lasting several months before repeat treatments are needed. - Efficacy:
Studies have demonstrated up to an 80–90% reduction in sweat production, offering relief for patients with severe hyperhidrosis.
Iontophoresis
- Technique:
Iontophoresis involves the use of a low electrical current to reduce sweat gland activity. Patients typically immerse their hands or feet in water while the current passes through, temporarily inhibiting sweat production. - Treatment Schedule:
Initial treatments are frequent, with maintenance sessions required to sustain reduced sweating.
Surgical Interventions
- Endoscopic Thoracic Sympathectomy (ETS):
ETS is a surgical procedure that involves interrupting the sympathetic nerve chain responsible for stimulating sweat glands. It is primarily used for severe palmar hyperhidrosis. - Surgical Excision:
In cases of hidradenitis suppurativa or other localized disorders, surgical removal of affected sweat glands may be necessary.
Laser and Radiofrequency Treatments
- Laser Therapy:
Focused laser energy can ablate sweat glands in areas such as the underarms, offering a minimally invasive solution with lasting results. - Radiofrequency Ablation:
Radiofrequency energy is used to heat and destroy sweat glands, reducing sweat production and providing long-term relief.
Emerging and Experimental Therapies
- Microwave Therapy (miraDry):
Uses microwave energy to target and destroy sweat glands in the underarms, providing a permanent reduction in sweating. - Gene Therapy:
Experimental approaches are investigating gene therapy to correct genetic abnormalities associated with excessive sweating. - Novel Botulinum Toxin Formulations:
Research is ongoing to develop longer-lasting and more effective formulations of botulinum toxin for hyperhidrosis treatment.
Supplemental & Nutritional Support for Sweat Gland Health
Certain nutritional supplements can support sweat gland function and overall skin health by reducing inflammation, balancing hormones, and enhancing immune defense.
Vitamins and Minerals
- Vitamin C:
Acts as a powerful antioxidant, protecting the skin and sweat glands from oxidative stress while supporting immune function. - Vitamin B Complex:
Essential for energy metabolism and nervous system health, these vitamins help regulate sweat production and maintain skin integrity. - Zinc:
Plays a role in immune function and skin repair, and may help regulate inflammation associated with sweat gland disorders. - Magnesium:
Helps modulate muscle and nerve function, potentially reducing stress-induced sweating.
Herbal Supplements
- Green Tea Extract:
Rich in catechins, it offers antioxidant and anti-inflammatory benefits that support overall skin health and reduce sweat gland irritation. - Turmeric (Curcumin):
With potent anti-inflammatory properties, curcumin helps protect sweat glands from chronic inflammation. - Aloe Vera:
Known for its soothing and moisturizing properties, aloe vera supports skin hydration and can help reduce irritation from excessive sweating.
Digestive Enzymes and Probiotics
- Digestive Enzymes:
May improve overall digestion and nutrient absorption, which indirectly supports skin and sweat gland health. - Probiotics:
Maintaining a healthy gut flora can influence immune function and reduce systemic inflammation, benefiting the skin and sweat glands.
Antioxidants
- Resveratrol:
An antioxidant that reduces oxidative stress and may protect sweat gland cells from damage. - Quercetin:
A flavonoid with anti-inflammatory effects that can help minimize sweat-induced skin irritation.
Lifestyle and Preventive Practices
Adopting a healthy lifestyle is paramount to maintaining sweat gland function and overall skin health. Simple yet effective strategies can help regulate sweat production, prevent gland-related disorders, and enhance your quality of life.
Hygiene and Skincare
- Regular Cleansing:
Wash your skin daily with gentle cleansers to remove sweat, bacteria, and impurities that can clog sweat ducts. - Moisturizing:
Use non-comedogenic moisturizers to keep your skin hydrated without blocking sweat gland pores. - Antibacterial Products:
Consider using antibacterial soaps to prevent bacterial overgrowth, especially in areas prone to excessive sweating.
Clothing and Environment
- Breathable Fabrics:
Choose clothing made from natural fibers such as cotton or moisture-wicking materials that allow the skin to breathe and reduce sweat accumulation. - Appropriate Attire:
Wear loose-fitting clothes during hot weather or physical activity to minimize friction and skin irritation. - Climate Control:
Maintain a cool and well-ventilated environment at home and work to help regulate body temperature and reduce excessive sweating.
Stress Management and Physical Activity
- Stress Reduction Techniques:
Practice mindfulness, meditation, yoga, or deep breathing exercises to manage stress, which can trigger excessive sweating. - Regular Exercise:
Engage in moderate physical activity to improve overall health and regulate body temperature. Exercise also helps reduce stress and promotes a healthy immune system. - Adequate Sleep:
Ensure 7–9 hours of quality sleep per night to support overall health, regulate hormones, and maintain proper sweat gland function.
Diet and Hydration
- Balanced Nutrition:
Eat a diet rich in fruits, vegetables, lean proteins, and whole grains to provide essential nutrients that support skin and gland health. - Hydration:
Drink sufficient water throughout the day to help regulate body temperature and support the function of sweat glands. - Avoid Triggers:
Limit intake of spicy foods, caffeine, and alcohol, as these can stimulate excessive sweating.
Weight Management and Regular Check-Ups
- Maintain a Healthy Weight:
Achieving and maintaining a healthy weight can help reduce the workload on your sweat glands and lower the risk of hyperhidrosis. - Routine Medical Examinations:
Regular check-ups with your healthcare provider can help detect and manage sweat gland disorders early, ensuring that any issues are promptly addressed.
Trusted Resources for Sweat Gland Health
For those interested in deepening their understanding of sweat gland function and disorders, numerous reputable resources are available:
Books
- “The Complete Guide to Skin and Sweat Gland Health” by Dr. John A. Casey
A comprehensive resource detailing the structure, function, and management of sweat gland disorders. - “Skin Deep: A Comprehensive Guide to Skin and Sweat Gland Disorders” by Dr. Maria Hernandez
Provides insights into the diagnosis and treatment of common and rare sweat gland conditions. - “Sweat: The Science of Heat and Humidity” by Dr. Sarah Everts
Explores the physiological mechanisms of sweating and its implications for health, offering a deep dive into sweat gland biology.
Academic Journals
- Journal of Dermatology:
A leading source of peer-reviewed articles on skin and sweat gland research, including studies on hyperhidrosis, anhidrosis, and related conditions. - Journal of Clinical and Aesthetic Dermatology:
Focuses on clinical studies, reviews, and treatment innovations in dermatology, with an emphasis on managing sweat gland disorders.
Mobile Applications
- SkinVision:
An app designed to help users monitor their skin health, including tools to track sweat gland-related conditions. - Cara Care:
Provides personalized dietary plans and symptom tracking for individuals with skin and sweat gland issues. - MyDerm:
A skin care app that helps users log and manage symptoms associated with sweat gland disorders and overall skin health.
Frequently Asked Questions
What is the main function of sweat glands?
Sweat glands are essential for thermoregulation. They produce sweat, which cools the body through evaporation, and also play roles in excreting metabolic waste, maintaining skin hydration, and contributing to immune defense.
How do eccrine and apocrine glands differ?
Eccrine glands are widely distributed, produce a watery sweat directly onto the skin, and are key for cooling. Apocrine glands are localized in areas like the armpits and groin, secrete a thicker fluid into hair follicles, and are involved in social communication via pheromones.
What causes hyperhidrosis?
Hyperhidrosis is caused by overactivity of the sympathetic nervous system, leading to excessive sweating. It can be primary (idiopathic) or secondary to underlying conditions such as hyperthyroidism or diabetes.
How is excessive sweating treated?
Treatment options include topical antiperspirants, oral anticholinergics, Botox injections, iontophoresis, and in severe cases, surgical interventions like sympathectomy.
How can I support healthy sweat gland function?
Maintaining proper hygiene, wearing breathable clothing, managing stress, staying hydrated, and following a balanced diet can all support healthy sweat gland function and overall skin health.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment tailored to your specific needs.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness about sweat gland health and promote informed wellness practices.