Introduction to Central Retinal Vein Occlusion
Central Retinal Vein Occlusion (CRVO) is a serious ocular condition caused by a blockage of the central retinal vein, which drains blood from the retina. This obstruction causes increased pressure within the retinal veins, resulting in hemorrhages, swelling, and impaired vision. CRVO is a leading cause of vision loss, particularly in older adults, and can occur suddenly or gradually. Understanding the risk factors, pathophysiology, and impact of CRVO is critical for successful prevention and treatment. This article provides a thorough overview of CRVO, emphasizing its underlying mechanisms, associated risk factors, and potential preventive measures.
Central Retinal Vein Occlusion: Detailed Overview
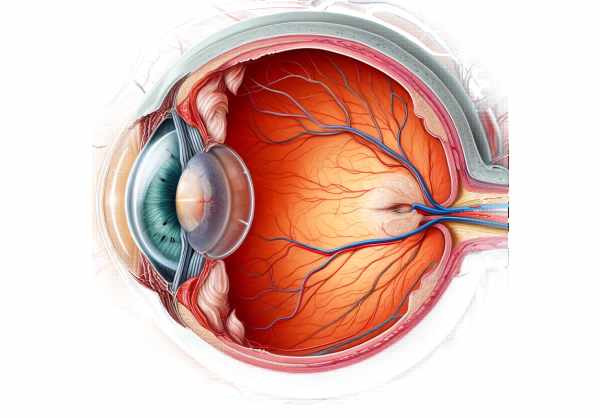
Central Retinal Vein Occlusion happens when the central retinal vein, which transports deoxygenated blood away from the retina, becomes clogged. The retina is a light-sensitive layer in the back of the eye that captures and transmits visual information to the brain. The central retinal vein and artery share a common adventitial sheath as they pass through the optic nerve, making the vein especially vulnerable to compression and occlusion caused by adjacent arterial abnormalities.
Pathophysiology
The pathophysiology of CRVO includes several interrelated processes:
- Venous Compression and Thrombosis: A thickened central retinal artery, possibly due to atherosclerosis, can compress the central retinal vein. This compression reduces venous outflow, resulting in turbulent blood flow, endothelial damage, and thrombus formation within the vein. The thrombus that forms further obstructs blood flow, resulting in a blood backlog and increased intravascular pressure.
- Retinal Ischemia and Edema: When venous outflow is blocked, capillary pressure increases, causing capillary walls to rupture and blood and fluid to leak into the retinal tissue. This results in retinal hemorrhages and macular edema, which severely impair visual function. Ischemia (lack of oxygen) also causes the release of vascular endothelial growth factor (VEGF), which promotes additional vascular leakage and neovascularization.
- Inflammation: Venous occlusion causes ischemic and hypoxic conditions in the retina, resulting in an inflammatory response. Inflammatory cytokines promote increased vascular permeability and tissue damage, exacerbating retinal swelling and hemorrhage.
Risk factors
Several risk factors contribute to the development of CRVO:
- Age: CRVO primarily affects older adults, with rates rising significantly after the age of 50. Age-related vascular health changes, such as increased arterial stiffness and atherosclerosis, raise the risk.
- Hypertension: High blood pressure is a major risk factor for CRVO because it causes arterial wall thickening and subsequently compresses the central retinal vein.
- Diabetes Mellitus: Diabetes causes vascular endothelial dysfunction and increased blood viscosity, which increases the risk of retinal vein thrombosis.
- Hyperlipidemia: High levels of cholesterol and triglycerides promote atherosclerosis, increasing the risk of venous compression by an atherosclerotic central retinal artery.
- Cardiovascular Disease: Conditions such as coronary artery disease, atrial fibrillation, and heart failure have been linked to an increased risk of CRVO due to their impact on overall vascular health and the possibility of thromboembolic events.
- Glaucoma: Elevated intraocular pressure in glaucoma can compress the central retinal vein, making people more likely to develop CRVO.
- Smoking: Tobacco use has been linked to increased vascular inflammation, endothelial damage, and atherosclerosis, all of which raise the risk of venous occlusion.
- Hypercoagulable States: Conditions that increase the risk of blood clotting, such as factor V Leiden mutation, antiphospholipid syndrome, and high homocysteine levels, can predispose people to CRVO.
Clinical Presentation.
CRVO is typically characterized by a sudden, painless loss of vision in one eye. The degree of vision loss varies according to the severity and location of the occlusion. In some cases, patients may experience blurred or distorted vision, which is known as metamorphopsia. Visual symptoms are frequently associated with the extent of retinal hemorrhage and macular edema.
Types of CRVOs
CRVO is divided into two types based on the extent of retinal ischemia:
- Non-ischemic CRVO: This type is distinguished by a partial blockage of the central retinal vein, which causes milder retinal hemorrhage and less severe visual impairment. Non-ischemic CRVO has a better prognosis and is less likely to cause complications than ischemic CRVO.
- Ischemic CRVO: In this more severe form, the central retinal vein is completely blocked, resulting in extensive retinal ischemia, significant hemorrhage, and profound vision loss. Ischemic CRVO is linked to an increased risk of complications, including neovascularization and neovascular glaucoma, both of which can result in further vision loss.
Complications
CRVO can cause a variety of complications that worsen vision:
- Macular Edema: The accumulation of fluid in the macula, the central part of the retina responsible for detailed vision, is a common side effect. Macular edema is a leading cause of vision loss in CRVO and must be treated promptly to avoid permanent damage.
- Neovascularization: The ischemic retina produces VEGF, which promotes the development of new, abnormal blood vessels. These vessels are delicate and prone to bleeding, resulting in vitreous hemorrhage and tractional retinal detachment.
- Neovascular Glaucoma: New blood vessels can form on the iris and angle of the eye, obstructing the outflow of aqueous humor and causing a significant rise in intraocular pressure. This condition, known as neovascular glaucoma, is difficult to treat and can cause severe vision loss.
Prognosis
The prognosis of CRVO varies with the type and severity of the occlusion. Non-ischemic CRVO has a better visual outcome, with many patients achieving some degree of recovery. In contrast, ischemic CRVO frequently results in a poor visual prognosis due to extensive retinal damage and the possibility of complications. Early diagnosis and treatment are critical for improving outcomes and maintaining vision.
Psychosocial impact
The sudden vision loss caused by CRVO can have a significant psychosocial impact on patients. It can cause difficulties with daily tasks, loss of independence, and emotional distress. Patients may experience anxiety, depression, and a lower quality of life. Comprehensive care, including psychological support and rehabilitation services, is critical for patients dealing with the challenges of living with CRVO.
Essential Preventive Tips
- Regular Eye Examination
- Get regular eye exams, especially if you have risk factors like hypertension, diabetes, or a family history of CRVO. Early detection and management of risk factors can help prevent the onset of CRVO.
- Control your blood pressure
- Maintain optimal blood pressure levels by making lifestyle changes and taking medications as directed by your healthcare provider. Proper blood pressure control lowers the risk of venous compression and thrombosis.
- Manage Diabetes
- Maintain blood sugar levels under control through proper dietary measures, medications, and frequent monitoring. Proper diabetes management prevents vascular complications, such as CRVO.
- Monitor and manage cholesterol levels
- Maintain healthy cholesterol and triglyceride levels by eating a balanced diet, exercising regularly, and taking medications as needed. Reducing hyperlipidemia reduces the likelihood of atherosclerosis and venous compression.
- Quit smoking
- Avoid using tobacco to reduce your risk of vascular inflammation, endothelial damage, and atherosclerosis. Seek help and resources for quitting smoking if needed.
- Exercise regularly
- Exercise regularly to improve cardiovascular health and lower the risk of CRVO-related conditions. Aim to complete at least 150 minutes of moderate-intensity exercise per week.
- Healthy diet
- Eat a heart-healthy diet high in fruits, vegetables, whole grains, and lean proteins to improve overall vascular health and lower your risk of occlusive events.
- Managed Glaucoma
- If you have glaucoma, strictly adhere to your treatment plan to keep your intraocular pressure under control. Regular monitoring and treatment can reduce the risk of CRVO caused by high eye pressure.
- Be aware of symptoms
- Recognize the symptoms of CRVO, such as sudden, painless vision loss or blurred vision, and seek emergency medical attention if they occur. Early intervention can improve outcomes while preserving vision.
Diagnostic methods
A thorough eye examination, as well as advanced imaging techniques, are required to diagnose Central Retinal Vein Occlusion (CRVO). Standard diagnostic techniques include:
Fundoscopy
A thorough examination of the retina with a slit-lamp biomicroscope and a fundus lens allows the ophthalmologist to detect characteristic signs of CRVO. These symptoms include retinal hemorrhages, dilated and tortuous retinal veins, cotton wool spots, and macular edema. The presence of a “blood and thunder” appearance in the retina is indicative of CRVO.
Fluorescein Angiogram
In fluorescein angiography, a fluorescent dye is injected into the bloodstream and photographed as it travels through the retinal vessels. This method aids in detecting areas of capillary non-perfusion, leakage, and neovascularization. It generates a detailed map of the retinal circulation, which is critical for determining the severity of ischemia and guiding treatment.
Optical coherence tomography (OCT)
OCT is a non-invasive imaging technique for creating high-resolution cross-sectional images of the retina. It is especially useful for determining the extent of macular edema, a common complication of CRVO. OCT can measure retinal thickness and visualize intraretinal and subretinal fluid, which is useful for diagnosis and monitoring treatment response.
OCTA (Optical Coherence Tomography Angiography)
OCTA is a novel imaging modality that produces detailed images of the retinal and choroidal vasculature without the use of dye injection. It visualizes blood flow and detects microvascular abnormalities such as capillary non-perfusion and neovascularization. OCTA is particularly effective for tracking disease progression and treatment efficacy.
Color Doppler Imaging (CDI)
CDI uses ultrasound to measure blood flow in the central retinal vein and other ocular vessels. It can help determine the presence and severity of blood flow abnormalities, which is critical for diagnosing CRVO and assessing the possibility of collateral circulation.
Electroretinography (ERG).
ERG measures the retina’s electrical response to light stimulation. In CRVO, the b-wave amplitude is frequently reduced, indicating impaired function of the inner retinal layers. The ERG can help determine the severity of retinal ischemia and guide treatment decisions.
These diagnostic methods, which range from traditional fundoscopy to advanced imaging techniques such as OCT and OCTA, provide a thorough assessment of CRVO, allowing for accurate diagnosis and effective management.
Effective Treatments for Central Retinal Vein Occlusion
The treatment of Central Retinal Vein Occlusion (CRVO) is intended to reduce macular edema, manage complications, and improve visual outcomes. Standard treatments and emerging therapies include the following:
Anti-VEGF Therapies
Anti-VEGF (vascular endothelial growth factor) injections are the primary treatment for macular edema associated with CRVO. VEGF inhibitors such as ranibizumab, bevacizumab, and aflibercept reduce vascular permeability and edema. Regular intravitreal injections are necessary to maintain therapeutic effects and improve vision.
Steroid injections
Intravitreal corticosteroids, such as triamcinolone acetonide and dexamethasone implants, are used to treat CRVO inflammation and edema. Steroid injections can help reduce macular thickness and improve visual acuity. However, there is a risk of side effects such as increased intraocular pressure and cataract formation.
Laser photocoagulation
Panretinal photocoagulation (PRP) is a treatment for neovascularization that also prevents complications like neovascular glaucoma. PRP entails applying laser burns to the peripheral retina to reduce VEGF release and discourage the formation of abnormal blood vessels. Focal laser photocoagulation can also be used to treat small areas of macular edema.
Hyperbaric oxygen therapy (HBOT)
HBOT involves breathing pure oxygen in a pressurized chamber to increase oxygen delivery to the retina. This therapy may help reduce ischemia and promote retinal healing in CRVO. While not widely used, HBOT is being investigated as a possible treatment for retinal vascular occlusions.
Ischemic management
The goal of ischemic CRVO management is to prevent complications and improve retinal perfusion. This may include the use of anticoagulants or antiplatelet agents to reduce the risk of future thrombotic events. Monitoring for neovascularization and prompt treatment with anti-VEGF therapy or laser photocoagulation are critical.
Emerging Therapies
The search for new treatments for CRVO is ongoing. Potential treatments include:
- Gene Therapy: Gene therapy techniques seek to alter the expression of genes involved in retinal ischemia and inflammation. This approach has the potential to provide long-term benefits by targeting the underlying pathophysiology of CRVO.
- Stem Cell Therapy: Stem cell transplantation is being studied for its potential to regenerate damaged retinal tissue and restore function. While still in the experimental stages, this therapy provides hope to patients suffering from severe retinal ischemia.
- Neuroprotective Agents: Neuroprotective drugs are intended to protect retinal neurons from ischemic damage. These agents may aid in the preservation of vision in CRVO patients by reducing oxidative stress and apoptosis.
- New Anti-VEGF Agents: Research into new anti-VEGF drugs with longer durations of action and fewer side effects is underway. These agents have the potential to provide more long-term control of macular edema while also reducing injection frequency.
In summary, CRVO is treated with a combination of anti-VEGF therapy, steroids, laser photocoagulation, and novel approaches such as HBOT and emerging therapies. Early intervention and regular monitoring are critical for improving visual outcomes and reducing complications.
Trusted Resources
Books
- “Retinal Vascular Disease” by A.M. Joussen, T.W. Gardner, B. Kirchhof, S.J. Ryan
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Retina” by Stephen J. Ryan, SriniVas R. Sadda






