Introduction
Cranial Nerve IV Palsy, also known as trochlear nerve palsy, is a neurological disorder that affects the fourth cranial nerve, which controls the superior oblique muscle of the eye. This muscle is essential for eye movement, particularly downward and inward movements. Damage to the trochlear nerve can cause vertical or torsional diplopia (double vision), difficulty reading or descending stairs, and a distinct head tilt to compensate for misalignment. Understanding the causes, clinical characteristics, and impact of Cranial Nerve IV Palsy is critical for accurate diagnosis and treatment.
Cranial Nerve IV Palsy Insight
Cranial Nerve IV Palsy is a condition that impairs the function of the superior oblique muscle, causing significant visual disturbances and reducing the patient’s quality of life. This palsy can be congenital or acquired, with different etiologies and clinical manifestations.
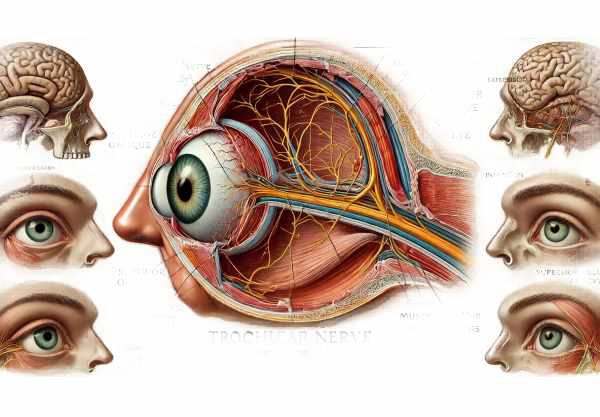
Anatomy and Function
The trochlear nerve is the fourth cranial nerve and is distinctive in several ways. It is the only cranial nerve that exits the brainstem dorsally and only innervates one muscle: the superior oblique. This muscle controls downward and inward eye movements, which are especially important when looking down or reading. The superior oblique also aids in intorsion, which is an inward rotation of the eye.
Cranial Nerve IV Palsy can be congenital or acquired, with a variety of causes.
Congenital Cranial Nerve IV Palsy.
Congenital disorders are frequently the result of developmental abnormalities. These patients usually adapt over time, resulting in subtle or compensated symptoms that may become apparent later in life when exacerbated by trauma or other factors.
Acquired Cranial Nerve IV Palsy
Acquired cases can result from several etiologies, including:
- Trauma: Head trauma is the leading cause of Cranial Nerve IV Palsy. The long course of the trochlear nerve makes it especially vulnerable to injury during head impacts.
- Microvascular Ischemia: Diabetes and hypertension can cause ischemia of the trochlear nerve, resulting in palsy, especially in older adults.
- Tumors: Neoplasms in the brainstem or along the path of the trochlear nerve can compress the nerve and cause dysfunction.
- Inflammatory and Infectious Diseases: Conditions such as multiple sclerosis, meningitis, and vasculitis can affect the trochlear nerve, resulting in palsy.
- Aneurysms: Rarely, aneurysms, particularly those near the Willis circle, can compress the trochlear nerve.
- Idiopathic: When no clear cause can be identified, the condition is referred to as idiopathic.
Clinical Manifestations
Patients with Cranial Nerve IV Palsy typically present with the following symptoms and signs associated with superior oblique muscle dysfunction:
- Vertical Diplopia: Double vision, especially when looking down or reading, is a common symptom. The images are frequently vertically misaligned, with one being tilted.
- Torsional Diplopia: Some patients have torsional diplopia, which occurs when the images are rotated relative to one another.
- Head Tilt: To compensate for diplopia, patients frequently tilt their heads toward the opposite shoulder. This compensatory mechanism uses the position of the unaffected eye to align the images.
- Difficulty Reading and Descending Stairs: Tasks that require downward gaze, such as reading or descending stairs, become difficult due to eye misalignment.
- Eye Misalignment: An examination of the affected eye may reveal hypertropia (upward deviation) when looking inward and downward.
Risk Factors
Several factors raise the risk of developing Cranial Nerve IV Palsy:
- Age: The risk of microvascular diseases like diabetes and hypertension rises with age, making older people more vulnerable.
- Trauma: Activities or situations involving a high risk of head injury can predispose people to traumatic Cranial Nerve IV Palsy.
- Medical Conditions: Preexisting conditions such as diabetes, hypertension, multiple sclerosis, and inflammatory diseases raise the risk.
- Genetic Factors: Congenital cases may have a genetic component, but specific genetic causes are not well defined.
Impact on Daily Life
Cranial Nerve IV Palsy has a significant impact on daily activities because of visual disturbances and compensatory head postures. Constant double vision can cause headaches, eye strain, and difficulty completing tasks that require precise vision. The head tilt can cause neck pain and discomfort in the long term. These symptoms reduce overall quality of life, necessitating effective management strategies.
Psychological and Social Implications
Living with Cranial Nerve IV Palsy can have a significant psychological and social impact. Visible eye misalignment, as well as compensatory head tilt, can have an impact on self-esteem and social interactions. Patients may experience anxiety and depression as a result of the chronic nature of their condition and its impact on daily life. Social activities and occupational performance may suffer, potentially resulting in isolation or embarrassment.
Prevention Tips
- Manage underlying health conditions. Control diabetes, hypertension, and other vascular risk factors with medication, diet, and lifestyle changes to lower the risk of microvascular cranial nerve damage.
- Use Protective Gear: Wear helmets and protective gear when participating in activities that pose a high risk of head injury, such as cycling, contact sports, and certain occupational tasks.
- Regular Medical Checkups: Routine health screenings can aid in the detection and management of conditions such as hypertension and diabetes, both of which are risk factors for Cranial Nerve IV Palsy.
- Avoid Inflammatory and Infectious Risks: Prevent infections like meningitis and reduce your exposure to inflammatory conditions by practicing good hygiene, getting vaccinations, and managing autoimmune disorders.
- Healthy Lifestyle Choices: To improve overall vascular health, maintain a healthy lifestyle that includes regular exercise, a balanced diet, and abstaining from smoking and drinking excessively.
- Eye Safety: Protect your eyes from trauma by taking appropriate precautions during activities that may result in eye injury.
- Monitor for Early Symptoms: Early detection of symptoms such as double vision or head tilt can result in timely medical evaluation and intervention, potentially preventing the condition from worsening.
Diagnostic Methods
Cranial Nerve IV Palsy is diagnosed through a comprehensive evaluation that includes a clinical examination, imaging studies, and, in some cases, specialized tests to determine the underlying cause and severity of the condition.
Clinical Examination
The diagnostic process starts with a thorough clinical examination by an ophthalmologist or neurologist. Key aspects of this exam include:
- Patient History: A detailed history is taken to determine the onset and progression of symptoms, as well as any recent trauma, medical conditions, and family history.
- Ocular Alignment Tests: Cover tests are used to assess eye alignment and detect hypertropia, as well as the head tilt that patients may use to compensate for diplopia.
- Eye Movement Evaluation: Examining the eyes’ range of motion, particularly for limitations in downward and inward gaze, which are indicative of superior oblique muscle dysfunction.
- Diplopia Charting: Documenting the nature and pattern of double vision to determine its extent and impact on daily activities.
Imaging Studies
Imaging is essential in determining the underlying cause of Cranial Nerve IV Palsy, especially in acquired cases.
- Magnetic Resonance Imaging (MRI): MRI is the preferred imaging modality because it provides detailed images of the brain and cranial nerves. It can detect structural abnormalities, tumors, inflammation, and demyelination.
- Magnetic Resonance Angiography (MRA): MRA is used to assess blood vessels and identify aneurysms or vascular malformations that may compress the trochlear nerve.
- Computed Tomography (CT) Scan: CT scans are commonly used in emergency situations to quickly assess for fractures, hemorrhages, or large masses. CT angiography can be especially useful in determining vascular causes.
- High-Resolution Orbital Imaging: This allows for detailed images of the orbits and extraocular muscles, which is useful when trauma or localized orbital pathology is suspected.
Specialized Tests
In some cases, additional tests are performed in order to better understand the functional impact of the palsy and plan treatment.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): These tests measure the electrical activity of the superior oblique muscle and the conduction of the trochlear nerve, which helps determine the extent of nerve damage.
- Vestibular Testing: Because the vestibular system is closely linked to eye movements and balance, vestibular tests can help rule out other conditions that may mimic or exacerbate symptoms of Cranial Nerve IV Palsy.
Emerging Diagnostic Techniques
Diagnostic technology advancements improve the accuracy and depth of evaluations for Cranial Nerve IV Palsy.
- Diffusion Tensor Imaging (DTI): This advanced type of MRI maps the brain’s white matter tracts, providing detailed information about the integrity of the trochlear nerve pathways.
- Functional MRI (fMRI): fMRI measures blood flow changes in the brain to determine how the palsy affects the visual and motor areas.
- Artificial Intelligence (AI) in Imaging: AI algorithms are being developed to more precisely analyze imaging data, potentially identifying subtle abnormalities that would otherwise go undetected by humans.
Treatment for Cranial Nerve IV Palsy aims to alleviate symptoms, correct eye misalignment, and address underlying causes. The type of treatment is determined by whether the palsy is congenital or acquired, as well as the severity and impact on daily activities.
Standard treatment options include non-surgical management.
- Observation: In cases of microvascular ischemic palsy, particularly in patients with diabetes or hypertension, observation is frequently recommended because these usually resolve spontaneously within three to six months.
- Prism Glasses: These special glasses help correct double vision by realigning the images, providing immediate relief to patients suffering from diplopia.
- Eye Patching: Covering one eye temporarily eliminates double vision, relieving symptoms and preventing compensatory head postures.
Surgical Interventions
When non-surgical treatments fail, or when the palsy is caused by structural issues such as trauma or tumors, surgery may be required.
- Strabismus Surgery: Surgical procedures that realign the eyes by adjusting the muscles surrounding them, particularly the superior oblique and its antagonist muscles. To improve alignment, techniques include weakening overacting muscles and tightening underacting ones.
- Superior Oblique Tendon Tuck: A procedure that tightens the superior oblique tendon to improve its function; commonly used in congenital cases.
Innovative and Emerging Therapies
Neurostimulation and Neuroplasticity.
Neurostimulation techniques such as transcranial magnetic stimulation (TMS) and direct current stimulation (tDCS) are being investigated for their potential to improve neural plasticity and aid in nerve function recovery.
Pharmaceutical Advances
New pharmacological treatments are being tested to alleviate symptoms and promote nerve healing. These include neuroprotective agents, which are designed to reduce damage and promote nerve fiber regeneration.
Genetic Therapy
New research in gene therapy is looking into ways to treat congenital forms of Cranial Nerve IV Palsy by correcting the underlying genetic abnormalities that cause developmental issues.
Personalized Medicine
Personalized approaches based on genetic and molecular profiling are being developed to tailor treatments to individual patients’ specific needs and conditions, thereby increasing the efficacy and outcomes of therapeutic interventions.
Trusted Resources
Books
- “Neuro-Ophthalmology Illustrated” by Valerie Biousse and Nancy J. Newman
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakrabarti
- “Cranial Nerves: Functional Anatomy” by Stanley Monkhouse






