What is Dermoid Cyst of the Orbit?
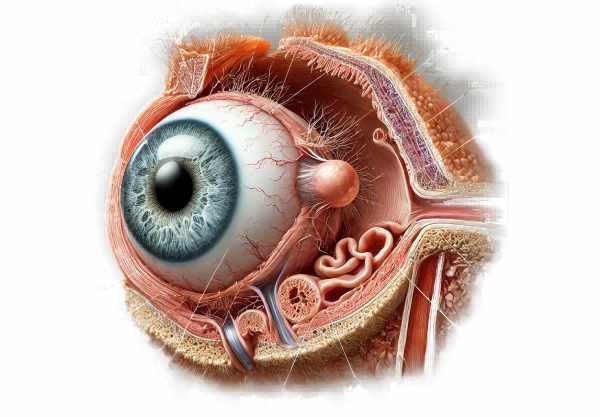
A dermoid cyst of the orbit is a benign, congenital lesion caused by ectodermal tissue trapped during embryonic development. These cysts are frequently found in the periorbital region, particularly near the lateral aspect of the brow. Dermoid cysts contain keratin, hair follicles, and sebaceous glands, and they can grow slowly over time. While they are usually present at birth, they may not be noticeable until later in childhood or even adulthood. Dermoid cysts, while benign, can cause cosmetic issues, discomfort, or visual impairment if they put pressure on ocular structures. Understanding the nature, causes, and implications of orbital dermoid cysts is critical for their successful management and treatment.
Dermoid Cyst of Orbit Detailed Insights
Dermoid cysts of the orbit are fascinating, yet complex congenital anomalies caused by the inclusion of ectodermal elements during embryogenesis. These cysts are lined with squamous epithelium and contain various ectodermal derivatives, including hair, sebaceous glands, and keratin. Their development is typically linked to the skull’s suture lines, specifically the frontozygomatic and frontoethmoidal sutures.
Pathophysiology
Dermoid cysts are thought to form when surface ectoderm is sequestered along embryonic fusion lines. As the craniofacial bones develop, remnants of ectodermal tissue may become trapped and differentiate into a cystic structure lined with epidermis-like cells. These cells continue to produce keratin and other skin components, gradually enlarging the cyst.
Epidemiology
Dermoid cysts of the orbit are relatively uncommon, accounting for only 3-9% of all orbital masses in children. They are typically diagnosed in early childhood, but some may go undetected until adulthood. There is no significant gender difference, and the condition can affect any race or ethnic group.
Clinical Manifestations
The appearance of a dermoid cyst varies according to its size, location, and rate of growth. Common clinical characteristics include:
- Palpable Mass: The most common sign is a painless, palpable mass near the outer edge of the brow or upper eyelid. The mass is usually mobile and non-tender.
- Cosmetic Concerns: Parents frequently seek medical advice for cosmetic reasons, as the cyst can cause visible swelling and asymmetry in the periocular region.
- Visual Impairment: Large cysts or those located deeper in the orbit can put pressure on ocular structures, potentially causing proptosis (forward displacement of the eye), astigmatism, or even amblyopia (lazy eye).
- Pain and Inflammation: While cysts are typically painless, they can become inflamed or infected, resulting in redness, tenderness, and swelling.
- Growth Over Time: Dermoid cysts grow slowly and can grow in size over many years. Growth spurts can be caused by trauma or hormonal changes during puberty.
Anatomical Variations
Dermoid cysts can be classified according to their anatomical location and size:
- Superficial Dermoid Cysts: These cysts are found near the skin’s surface and typically appear as a small, mobile lump. They are the most common type and are typically found near the outer brow.
- Deep Orbital Dermoid Cysts: These cysts extend deeper into the orbit and can cause more severe clinical symptoms because they are close to critical ocular structures. They are frequently discovered later in life due to their less obvious presentation.
- Complex Dermoid Cysts: These cysts can extend across multiple anatomical planes and affect both superficial and deep tissues. They can result in more severe deformities and complications.
Complications
While dermoid cysts are benign, they can cause a number of complications if not treated:
- Infection: The cyst may become infected, resulting in the formation of an abscess and the possibility of spreading to adjacent structures.
- Erosion and Rupture: The cyst may erode into nearby bones or rupture, resulting in inflammation and fibrosis in the surrounding tissues.
- Visual Disturbances: Pressure from the cyst can cause proptosis, strabismus (eye misalignment), and visual impairment.
- Cosmetic Deformity: Larger cysts can result in noticeable facial asymmetry and cosmetic concerns, affecting the patient’s self-esteem and quality of life.
Risk Factors
Certain factors may increase the likelihood of developing or exacerbating an orbital dermoid cyst.
- Congenital Factors: Because dermoid cysts are congenital, the main risk factor is the presence of ectodermal tissue remnants during embryonic development.
- Trauma: Trauma to the periocular region can occasionally cause inflammation or rapid growth of a previously undetected cyst.
- Hormonal Changes: Hormonal changes during puberty can promote cyst growth, making previously small and unseen cysts more visible.
Differential Diagnosis
When evaluating a patient with a suspected dermoid cyst, it is important to consider other possible diagnoses that can present with similar clinical features:
- Epidermoid Cysts: Similar to dermoid cysts, but without complex structures like hair and sebaceous glands.
- Lipoma: A benign fatty tissue tumor that appears as a soft, mobile mass.
- Lacrimal Gland Tumors: These appear as a mass in the superotemporal orbit and may require imaging to distinguish from dermoid cysts.
- Lymphangioma is a benign vascular tumor that can cause orbital swelling and proptosis.
- Encephalocele: A herniation of brain tissue through a skull defect, resulting in a pulsatile orbital mass.
Effects on Quality of Life
The presence of a dermoid cyst can have a significant impact on a patient’s quality of life, especially if it causes visible deformity or functional impairment. Parents may be concerned about their child’s appearance and potential for vision impairment. Early diagnosis and appropriate management are critical for mitigating these effects and ensuring the best possible outcomes for affected individuals.
Tips to Avoid Orbital Dermoid Cysts
The primary goal of preventing orbital dermoid cysts is to reduce risks and promote early detection. Here are some important precautions and risk reduction tips:
- Regular Pediatric Check-Ups: Schedule regular pediatric appointments to check for any signs of congenital anomalies, such as dermoid cysts.
- Early Intervention: If a swelling or lump appears near the eye or brow, seek medical attention immediately, even if it appears benign.
- Protective Eyewear: Encourage the use of protective eyewear during activities that may cause facial trauma to avoid triggering the growth or inflammation of existing cysts.
- Education on Signs and Symptoms: Inform parents and caregivers about the signs and symptoms of dermoid cysts in order to facilitate early detection and treatment.
- Avoid Unnecessary Trauma: Limit activities that pose a high risk of facial injury, particularly in children who have a known dermoid cyst.
- Monitor Hormonal Changes: Be aware that hormonal changes during puberty can influence the growth of dermoid cysts, and seek medical advice if any changes occur.
- Genetic Counseling: Families with a history of congenital anomalies should seek genetic counseling to better understand potential risks and early detection strategies.
- Prompt Treatment of Infections: Treat any eye or skin infections as soon as possible to reduce the risk of secondary complications related to the cyst.
- Follow Medical Advice: To avoid complications, follow your healthcare provider’s recommendations for monitoring and managing dermoid cysts.
- Maintain a Healthy Lifestyle: Promote a healthy lifestyle that includes proper nutrition and hydration to improve overall skin and tissue health.
Diagnostic methods
Orbital dermoid cysts are diagnosed using a combination of clinical and imaging studies. A detailed history and physical examination are usually part of the initial assessment. Clinicians look for distinctive signs, such as a painless, palpable mass in the orbital region, which is frequently located on the outer aspect of the brow. Proptosis, diplopia, or visual disturbances may require further investigation.
Ultrasonography is commonly used as the first-line imaging modality, particularly for superficial cysts. It helps to determine the cyst’s size, location, and content. Ultrasonography is advantageous because of its non-invasive nature, lack of radiation exposure, and ease of use, especially in pediatric patients.
Computed Tomography (CT) scans yield detailed images of the orbital anatomy, including bony structures. CT imaging is especially useful in determining the extent of bone involvement, such as remodeling or erosion caused by the expanding cyst. It aids in distinguishing dermoid cysts from other bony lesions and detecting any potential complications affecting nearby structures.
Magnetic Resonance Imaging (MRI) provides better soft tissue resolution than CT scans and is useful for determining the relationship between the cyst and the surrounding orbital tissues. MRI is especially useful for detecting deeper cysts or those with complex anatomical relationships to the optic nerve and extraocular muscles. MRI’s non-ionizing nature makes it a safer option for repeated imaging, particularly in children.
Advanced diagnostic techniques such as diffusion-weighted imaging (DWI) and spectroscopy can provide additional information about the cyst’s content and structure. DWI can help distinguish between dermoid cysts and other orbital masses based on differences in water diffusion properties. Spectroscopy can determine the chemical composition of the cyst, assisting in differential diagnosis.
In some cases, a fine-needle aspiration biopsy (FNAB) may be used to collect a sample of cyst content for histopathological analysis. This is usually reserved for atypical cases where non-invasive imaging is inconclusive and it is necessary to rule out malignancy or other cystic lesions.
Orbital Dermoid Cyst Therapies
Orbital dermoid cysts are treated primarily through surgical excision. The goal of surgery is to completely remove the cyst and its capsule in order to prevent recurrence. Surgical approaches vary according to the cyst’s location, size, and depth.
A simple excision of superficial cysts is typically performed through a small incision over the cyst. This method reduces scarring and allows for the complete removal of the cyst without causing significant damage to surrounding tissues. The procedure is frequently performed on an outpatient basis using local anesthesia, particularly in older children and adults.
Deep orbital cysts necessitate more complex surgical planning and may necessitate a multidisciplinary team that includes ophthalmologists and neurosurgeons. To access deep cysts, an anterior or lateral orbitotomy is often required, which provides adequate exposure to safely remove the cyst. When the cyst is close to critical structures like the optic nerve, precise dissection is required to avoid damage and maintain function.
Endoscopic approaches are emerging as less invasive treatments for specific orbital cysts. Endoscopic surgery uses small incisions and specialized instruments to access and remove the cyst. This technique shortens postoperative recovery time and addresses cosmetic concerns. However, endoscopic approaches are technically demanding and may not be appropriate in all cases.
Adjunctive treatments include corticosteroids to reduce inflammation and antibiotics for infection. In cases where complete excision is not possible due to the cyst’s location or the patient’s comorbidities, periodic imaging studies are recommended to assess cyst growth and plan future interventions.
Innovative therapies and research are exploring the use of minimally invasive techniques, such as sclerotherapy, which involves injecting sclerosing agents into the cyst to reduce its size. Advances in robotic surgery and image-guided navigation systems are also being studied to improve accuracy and safety during cyst excision.
Trusted Resources
Books
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright
- “Orbital Surgery: A Conceptual Approach” by Jack Rootman
- “Ocular and Orbital Tumors in Children and Adults” by Jerry A. Shields










