Introduction to Epiphora
Epiphora, also known as excessive tearing, is a condition in which tears overflow onto the face. This happens when the tear drainage system becomes blocked or unable to function properly, or when there is an excess of tears. Epiphora can affect one or both eyes, reducing a person’s quality of life through discomfort, blurred vision, and social embarrassment. Understanding the underlying causes and mechanisms of epiphora is critical to accurate diagnosis and treatment.
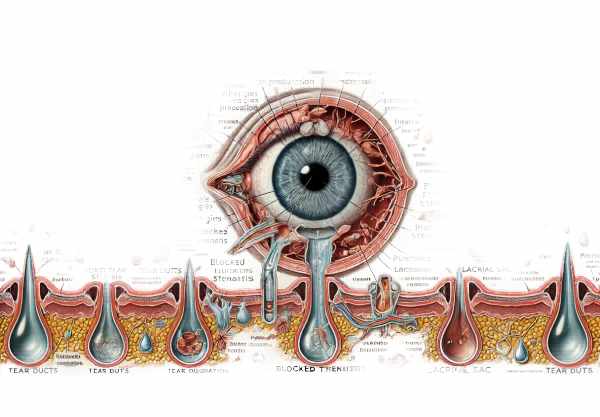
In-Depth Look at Epiphora
Epiphora can be caused by a variety of factors, which can be divided into two categories: excessive tear production and impaired tear drainage. Each category includes several distinct conditions and mechanisms that contribute to excessive tearing.
Increased Tear Production
Irritation or inflammation of the ocular surface can cause an increase in tear production by stimulating the lacrimal glands. Common causes of increased tear production are:
- Dry eye Syndrome
- Dry eye syndrome, paradoxically, can cause excessive tearing as the eye produces more tears to compensate for the dryness and irritation. This condition, referred to as reflex tearing, is frequently caused by insufficient lubrication and chronic ocular surface irritation.
- Allergies
- Allergic conjunctivitis, caused by allergens such as pollen, dust, or pet dander, can cause inflammation and itching in the eyes, resulting in an overproduction of tears.
- Infections
- Conjunctivitis (pink eye) and keratitis (corneal infection) are two common infections that cause redness, swelling, and increased tear production as part of the immune response.
- Foreign bodies
- Foreign bodies, such as dust, sand, or eyelashes, can irritate the ocular surface, causing excessive tearing as the eye tries to flush the irritants out.
- Corneal Abrasion
- Corneal scratches or injuries can cause significant discomfort and trigger reflex tearing as the eye attempts to heal the damaged tissue.
Impaired Tear Drainage
Impaired tear drainage occurs when there is an obstruction or malfunction in the lacrimal drainage system, preventing tears from draining properly through the nasolacrimal duct. Common causes of impaired tear drainage are:
- Nasolacrimal Duct Obstruction
- This condition is characterized by a blockage in the tear drainage system, typically at the level of the nasolacrimal duct, which can be congenital or acquired. Infections, inflammation, trauma, and tumors can all cause obstructions to form.
- Eyelid Malposition
- Ectropion (outward turning of the eyelid) and entropion (inward turning of the eyelid) can disrupt the puncta’s normal alignment, resulting in poor tear drainage and subsequent tear overflow.
- Punctual Stenosis
- Punctal stenosis is a narrowing or closure of the puncta that can be caused by chronic inflammation, infections, or aging. This condition prevents tears from passing through the tear drainage system efficiently.
- Dacryocystitis
- Inflammation or infection of the lacrimal sac (dacryocystitis) can obstruct tear drainage, causing tears to pool and overflow onto the face. This condition is frequently characterized by pain, redness, and swelling near the inner corner of the eye.
Symptoms and Signs
The primary symptom of epiphora is an excessive overflow of tears, which can be continuous or intermittent. Additional symptoms and signs could include:
- Blurry Vision: Excessive tearing can result in intermittent blurring of vision as tears pool on the ocular surface.
- Irritation and Redness: Prolonged tearing can cause skin irritation and redness near the eyes and cheeks.
- Discharge: Infection or dacryocystitis can cause mucopurulent discharge and excessive tearing.
- Pain and Discomfort: Obstructive causes of epiphora, such as dacryocystitis, can cause pain and discomfort, especially in the inner corner of the eye.
Risk Factors
Epiphora can be caused by a variety of factors, including:
- Age: Changes in the eyelids and tear drainage system can lead to the development of epiphora, especially in older adults.
- Gender: Women are more likely to develop dry eye syndrome and punctal stenosis, which can cause excessive tearing.
- Environmental Factors: Smoke, wind, and chemicals can all cause ocular surface irritation and excessive tearing.
- Medical Conditions: Allergies, autoimmune diseases, and chronic sinus infections can all increase the risk of developing epiphora.
Complications
If left untreated, epiphora can lead to a number of complications, including:
- Chronic Discomfort: Persistent tearing can cause long-term discomfort and irritation, affecting daily activities and quality of life.
- Skin Maceration: Prolonged exposure to tears can cause skin maceration and breakdown around the eyes and cheeks, raising the risk of secondary infections.
- Visual Impairment: Chronic tearing can impair vision, especially while reading or driving, posing a safety risk.
- Infections: Obstructive causes of epiphora, such as nasolacrimal duct obstruction, can increase the likelihood of recurring infections and inflammation.
Epidemiology
Epiphora is a common condition that affects people of all ages, but it is more common in older adults due to changes in the tear drainage system. The prevalence of epiphora varies depending on the underlying cause and the population studied. For example, nasolacrimal duct obstruction is a common cause of epiphora in infants, whereas punctal stenosis and eyelid malpositions are more common in older people.
Patient Education and Support
Educating patients about epiphora is critical for early detection and treatment. Patients should be educated on the symptoms and risk factors, and encouraged to seek immediate medical attention if they experience persistent tearing or discomfort. Support groups and counseling can also help patients deal with the emotional and practical aspects of epiphora.
Methods for Epiphora Diagnosis
Epiphora is diagnosed through a comprehensive clinical evaluation, which may include specialized tests to determine the underlying cause and severity of the condition.
Clinical Examination
Epiphora is diagnosed first with a thorough clinical examination by an ophthalmologist. This includes:
- Patient History: The ophthalmologist will take a thorough history to determine the cause, duration, and pattern of tearing, as well as any associated symptoms or prior eye conditions.
- Visual Inspection: The doctor will check the eyelids, puncta, and surrounding areas for signs of malposition, inflammation, or obstruction.
- Slit-Lamp Examination: A slit-lamp microscope enables a thorough examination of the ocular surface, tear film, and tear drainage system. This aids in detecting signs of irritation, infection, and structural anomalies.
Diagnostic Tests
Several diagnostic tests are available to assess tear production, drainage, and the presence of any obstructions or abnormalities:
- Tear Breakup Time (TBUT)
- This test determines the stability of the tear film by applying a fluorescein dye to the eye and timing how long it takes for dry spots to appear on the cornea. A lower TBUT may indicate tear film instability and dry eye syndrome.
- Schirmer Test.
- The Schirmer test assesses tear production by placing a small strip of filter paper under the lower eyelid and measuring the amount of wetting over a given time period. This test aids in the diagnosis of conditions characterized by decreased tear production.
- Dye Disappearance Test.
- In this test, fluorescein dye is injected into the eye and the time it takes to drain through the nasolacrimal duct is measured. Delayed dye clearance may indicate a blockage in the tear drainage system.
- Lacrimal Syringes and Probing
- Lacrimal syringing is the process of flushing saline through the tear drainage system to check for blockages. Probing may be used to investigate the nasolacrimal duct and identify the source of the obstruction.
- Imagery Studies
- Imaging studies, such as dacryocystography (X-ray imaging of the tear drainage system) and dacryoscintigraphy (radioactive dye imaging), can provide detailed views of the lacrimal drainage anatomy and reveal obstructions or structural abnormalities.
Ancillary tests
Additional tests may be required to identify the underlying causes or associated conditions.
- Conjunctival Swab and Culture: In cases of suspected infection, a swab of the conjunctiva may be taken to identify the causative organism and guide treatment options.
- Allergy Testing: Allergy testing may be used to identify specific allergens that cause allergic conjunctivitis and increased tear production.
Epiphora: Standard and Emerging Treatments
The treatment of epiphora is determined by the underlying cause, the severity of the symptoms, and the presence of complications. Treatment options range from conservative to surgical interventions, with an emphasis on addressing the underlying cause of excessive tearing.
Standard Treatment Options
- Conservative management
- Lubricating Eye Drops and Ointments: These can alleviate symptoms by reducing irritation and improving tear film stability, particularly in cases of dry eye syndrome.
- Warm Compresses: Using warm compresses can help with mild eyelid inflammation or meibomian gland dysfunction by improving tear quality and reducing irritation.
- Eyelid Hygiene: Maintaining proper eyelid hygiene through gentle cleaning can help manage conditions such as blepharitis, which contribute to epiphora.
- Medications
- Antibiotics: To treat bacterial infections that cause conjunctivitis or dacryocystitis, topical or oral antibiotics may be prescribed.
- Anti-inflammatory Agents: Steroid eye drops or nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation in allergic conjunctivitis and other inflammatory conditions.
- Antihistamines: For allergic causes of excessive tear production, antihistamine eye drops or oral medications can help relieve symptoms.
- Punctal plugs
- Punctal plugs can be used to partially or completely block the puncta, which are the openings of the tear drainage system, in cases of excessive tears. This can help keep tears on the ocular surface, providing relief to patients with dry eye syndrome.
Surgical Interventions
- Dilation and probing
- To remove blockages, the tear drainage ducts are widened and probed. It is commonly used in cases of congenital nasolacrimal duct obstruction in infants and can be performed under local anesthesia in adults.
- Dacryocystorhinostomy (DCR)
- DCR is a surgical procedure that creates a new drainage pathway between the lacrimal sac and the nasal cavity, avoiding any obstructions in the nasolacrimal duct. This procedure, which can be performed externally or endoscopically, is highly effective in treating epiphora caused by nasolacrimal duct obstruction.
- Punctoplasty
- Punctoplasty entails expanding the punctal openings to improve tear drainage. This procedure is commonly used to treat punctal stenosis and can significantly alleviate epiphora symptoms.
- Eyelid surgery
- In cases of eyelid malposition, such as entropion or ectropion, surgical correction of the eyelid position can restore normal tear drainage and reduce excessive tear production.
Innovative and Emerging Therapies
- Minimally Invasive Procedures.
- Advances in minimally invasive techniques, such as balloon dacryoplasty and laser-assisted procedures, provide less invasive alternatives with shorter recovery times and a lower risk of complications.
- Botulinum toxin Injections
- Functional epiphora can be treated with botulinum toxin (Botox) injections, which temporarily paralyze the muscles responsible for tear drainage dysfunction. This approach offers temporary relief and can be repeated as needed.
- Genetic Therapy
- Gene therapy research aims to correct genetic defects that contribute to conditions such as congenital nasolacrimal duct obstruction, which could provide a long-term solution.
- stem cell therapy
- Stem cell therapy is being investigated for its ability to regenerate damaged lacrimal gland tissue and restore normal tear production and drainage functions.
These novel therapies, combined with advances in surgical techniques, offer hope for more effective and less invasive epiphora treatments in the future.
Best Practices for Epiphora Prevention
- Regular Eye Exam
- Schedule regular eye exams to detect early signs of tear drainage issues and to monitor your eyes’ overall health.
- Maintain eyelid hygiene
- To avoid infections and inflammation, keep your eyelids and lashes clean on a regular basis.
- Avoid Environmental Irritators
- Keep your eyes away from smoke, wind, and chemicals, which can irritate the ocular surface and cause excessive tear production.
- Wear Protective Eyewear
- Wear protective eyewear when participating in activities that could result in eye injury, such as sports or work with hazardous materials.
- Manage Allergies
To reduce the risk of allergic conjunctivitis and excessive tearing, use antihistamines effectively and avoid known allergens. - Stay hydrated
- Stay hydrated to promote overall eye health and avoid dryness, which can lead to reflex tearing.
- Avoid eye rubbing
- Avoid rubbing your eyes vigorously, as this can aggravate irritation and increase tear production.
- Use Lubricating Eye Drops.
- Use lubricating eye drops to keep the tear film stable and avoid dryness and irritation.
- Monitor Medication Side Effects
- Be aware of medications that may cause dry eyes or increased tear production, and discuss any concerns with your doctor.
- Seek Early Treatment for Eye Infections.
- Treat any eye infections immediately to avoid complications and lower the risk of chronic tearing.
Trusted Resources
Books
- “Lacrimal Drainage Surgery” by David G. Tse
- “Ophthalmology” by Myron Yanoff and Jay S. Duker
- “The Lacrimal System: Diagnosis, Management, and Surgery” by Adam J. Cohen and Michael Mercandetti










