Introduction to the Epiretinal Membrane
An epiretinal membrane (ERM), also known as macular pucker or cellophane maculopathy, is a condition in which a thin, fibrous layer forms on the retina’s surface, particularly over the macula. The macula is the central part of the retina that allows for sharp central vision and fine detail. When an ERM develops, it can cause vision distortion, blurriness, and sometimes double vision. This condition is more common in older adults and has a significant impact on quality of life, making early detection and understanding critical.
Understanding Epiretinal Membrane Mechanisms
The formation of an epiretinal membrane is characterized by complex changes within the eye, which are frequently associated with aging or other ocular conditions. Understanding the development, causes, symptoms, and risk factors of ERM can help you understand how it affects your vision and overall eye health.
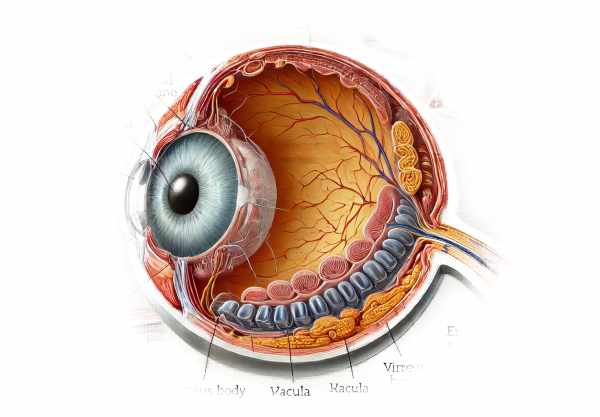
Pathophysiology
The retina is a delicate, multilayered tissue in the back of the eye that captures light and transmits visual information to the brain. The macula, which is located in the center of the retina, is essential for central vision. An epiretinal membrane forms when cells proliferate on the retina’s surface, resulting in a semi-transparent layer. This membrane can contract, causing the retinal layers beneath it to wrinkle or pucker. The distortion of the retinal surface causes visual disturbances.
Causes and Risk Factors
Several factors can lead to the formation of an epiretinal membrane:
- Age: Age-related changes are the most common cause of ERM. As the eye ages, the vitreous gel within it can shrink and pull away from the retina, a condition known as posterior vitreous detachment (PVD). This can cause microscopic damage to the retinal surface, which promotes the formation of an ERM.
- Retinal Tears or Detachments: Any injury to the retina, such as tears or detachments, can stimulate the formation of an ERM as part of the recovery process.
- Inflammation: Conditions that cause inflammation in the eye, such as uveitis, can increase the risk of developing ERM.
- Diabetic Retinopathy: Patients with diabetic retinopathy have a higher risk of ERM due to retinal damage and microvascular changes caused by diabetes.
- Ocular Surgeries: Previous eye surgeries, such as cataract removal or retinal procedures, can raise the risk of an ERM forming.
- Trauma: Direct injury to the eye can also cause the formation of an ERM.
Symptoms
The symptoms of an epiretinal membrane vary according to its severity and location. Common symptoms include:
- Blurry Vision: The wrinkling of the macula can cause general blurriness of vision.
- Visual Distortion: Patients may experience metamorphopsia, which makes straight lines appear wavy or bent.
- Double Vision: In some cases, particularly when the membrane affects one eye more than the other, double vision (diplopia) may occur.
- Difficulty Reading: The central vision impairment makes reading or any activity that requires fine detail difficult.
- Reduced Visual Acuity: The overall clarity of vision can deteriorate, affecting daily activities.
Effects on Quality of Life
ERM-related symptoms can have a significant impact on one’s quality of life. Reading, driving, and other activities that require clear vision can become challenging. The visual distortion can be especially bothersome, resulting in frustration and decreased functional ability. Early detection and appropriate management are critical to mitigating these effects.
Epidemiology
Epiretinal membrane is fairly common, especially in older adults. According to studies, its prevalence rises with age, affecting up to 7% of those over the age of 60. The condition can be unilateral or bilateral, but it most commonly affects one eye. The progression of ERM is variable; some membranes remain stable, while others progress and cause increasing visual symptoms over time.
Complications
If left untreated, an epiretinal membrane can cause a variety of complications, including:
- Severe Visual Impairment: Progressive wrinkling of the macula can result in significant vision loss.
- Macular Edema: Fluid accumulation in the macula can worsen vision.
- Retinal Detachment: In severe cases, the membrane’s traction can cause retinal detachment, which is a sight-threatening condition.
Patient Education and Support
Educating patients about the symptoms and progression of epiretinal membrane disease is critical. Patients should be encouraged to schedule regular eye exams, especially if they notice changes in their vision. Support groups and counseling can assist patients in coping with visual disturbances and their impact on daily life.
Methods for Epiretinal Membrane Diagnosis
An epiretinal membrane is diagnosed using a combination of clinical evaluation, imaging techniques, and functional tests to determine the extent and severity of the condition.
Clinical Examination
A comprehensive clinical examination by an ophthalmologist is the first step in diagnosing ERM. This includes:
- Visual Acuity Test: Measuring a patient’s ability to see at different distances helps determine the severity of visual impairment.
- Dilated Fundus Examination: Using drops to dilate the pupils allows the ophthalmologist to examine the retina and macula more closely. An ERM is commonly identified as a shiny or wrinkled area on the retinal surface.
Imaging Techniques
Advanced imaging techniques are essential for diagnosing and monitoring epiretinal membranes.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique that uses light waves to create cross-sectional images of the retina. It provides detailed images of the retinal layers, allowing you to visualize the ERM and assess its thickness and effect on the macula. OCT can detect even subtle changes in the retina, making it a valuable tool for diagnosing ERM.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and photographing the retina while the dye circulates. It aids in detecting abnormalities in the retinal blood vessels and can reveal areas of leakage or abnormal growth associated with ERM.
- Fundus Photography: Standard fundus photography captures a wide-angle view of the retina, allowing for long-term documentation and comparison. It is useful for monitoring changes in the appearance of the ERM.
Functional Tests
Functional tests assess the impact of ERM on vision and assist in determining the necessity and urgency of treatment.
- Amsler Grid Test: This simple test detects visual distortions by drawing a grid of horizontal and vertical lines. Patients with ERM may notice wavy or missing lines, indicating metamorphopsia.
- Contrast Sensitivity Test: This test assesses the ability to distinguish between different shades of grey, which is influenced by ERM. Reduced contrast sensitivity can have an impact on daily activities like driving and reading.
Ancillary tests
Additional tests may be performed to rule out other conditions and provide a complete understanding of the patient’s ocular health.
- Electroretinography (ERG): ERG assesses the retina’s electrical responses to light stimulation. It can aid in distinguishing ERM from other retinal conditions that may exhibit similar symptoms.
- Visual Field Testing: This test evaluates peripheral vision and can help identify any areas of vision loss caused by ERM.
Epiretinal Membrane: Standard and Emerging Treatments
Treatment for epiretinal membrane (ERM) is determined by the severity of the symptoms and their impact on vision. In many cases, if the symptoms are mild and do not significantly impair vision, close monitoring and regular eye exams may suffice. However, for patients who have significant visual impairment or discomfort, surgical intervention may be required.
Standard Treatment Options
- Observation and Monitoring: Ophthalmologists may recommend regular monitoring for mild cases with minimal symptoms. Periodic eye exams and OCT scans are used to monitor membrane progression and vision changes.
- Vitrectomy – Pars plana vitrectomy is the primary surgical procedure for treating symptomatic ERM. In this procedure, a vitreoretinal surgeon removes the vitreous gel from the eye in order to access the retina. The epiretinal membrane is gently peeled away from the retinal surface. This surgery is done under local or general anesthesia and usually results in a significant improvement in vision. The recovery period varies, but patients usually notice gradual visual improvement over several weeks or months.
- Pharmaceutical interventions Although less common, pharmacological treatments such as injecting anti-inflammatory or anti-fibrotic agents into the eye are being investigated. The goal of these injections is to reduce inflammation and prevent membrane progression.
Innovative and Emerging Therapies
- Microincision Vitrectomy Surgery (MIVS) Microincision vitrectomy surgery, which uses smaller incisions and less invasive methods, was developed as a result of advancements in surgical technique. MIVS provides faster recovery times, lower surgical risks, and better patient outcomes than traditional vitrectomy.
- Enzyme Therapy – Research is underway to use enzyme therapy to dissolve the epiretinal membrane without surgery. Enzymes like ocriplasmin have shown promise in breaking down fibrous tissue, suggesting a less invasive treatment option.
- Gene Therapy – Gene therapy is being studied as a treatment option for ERM, especially in cases with genetic predispositions. This approach seeks to correct the underlying genetic causes while also preventing membrane formation or recurrence.
- Stem Cell Therapy – Stem cell research aims to regenerate damaged retinal cells and restore normal function. Stem cell therapy, which is still in the experimental stages, has the potential to revolutionize the treatment of ERM and other retinal conditions.
- Nanotechnology for Drug Delivery Nanotechnology is being used to create advanced drug delivery systems that can target specific cells in the retina. These systems aim to deliver medications more effectively while reducing side effects, potentially improving ERM treatment outcomes.
Patients and healthcare providers can make informed decisions about the best treatment options for managing epiretinal membrane by staying up to date on emerging therapies and surgical advancements.
Best Ways to Avoid Epiretinal Membrane
- Schedule regular eye exams, particularly if you are over 50 or have a history of eye conditions. Early detection can help manage potential problems before they worsen.
- Protect Your Eyes from Injury – Wear protective eyewear when participating in activities that may cause eye injury, such as sports, home improvement projects, or working with hazardous materials.
- Manage systemic conditions such as diabetes and hypertension, which can lead to retinal problems. Regular checkups and appropriate treatment can help to avoid complications.
- Avoid Eye Rubbing: Excessive rubbing can damage the retina and increase the risk of ERM formation.
- Monitor PVD Symptoms: If you notice flashes of light or floaters, seek medical attention right away to avoid complications.
- Maintain Eye Health: Practice good hygiene, use lubricating drops as needed, and wear sunglasses to protect your eyes from UV light.
- Be Aware of Medication Side Effects – Certain medications may impact eye health. Discuss any concerns with your healthcare provider, and follow their recommendations for regular eye exams.
- Maintain a healthy diet with antioxidants and omega-3 fatty acids to promote eye health. Avoid smoking and excessive alcohol consumption, as both can raise the risk of developing eye conditions.
- Stay Informed: Stay up-to-date on eye health research and advancements. Awareness and education can help you take proactive steps to avoid ERM and other ocular conditions.
- Seek prompt treatment for eye infections to avoid complications such as epiretinal membrane formation.
Trusted Resources
Books
- “Retina” by Stephen J. Ryan
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Vitreoretinal Surgery: Strategies and Tactics” by Carl D. Regillo and Allen C. Ho










