What is Ocular Circatricial Pemphigoid?
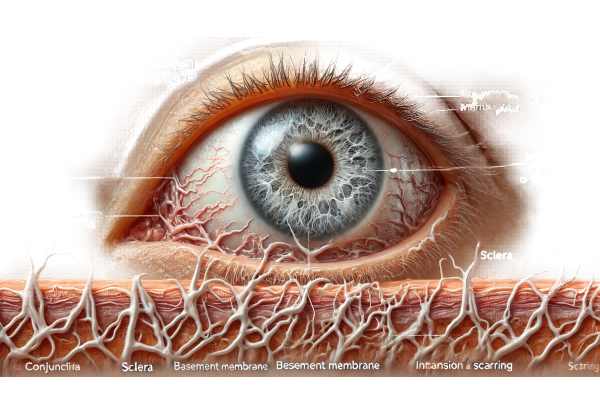
Ocular cicatricial pemphigoid (OCP) is a rare, chronic autoimmune disease that affects the mucous membranes, primarily the conjunctiva of the eyes. This condition causes progressive scarring and fibrosis, which may result in severe vision impairment or blindness. It is a type of mucous membrane pemphigoid (MMP) in which the immune system mistakenly attacks the conjunctiva’s basement membrane. OCP primarily affects older adults and, if not properly managed, can have a significant impact on their quality of life.
Detailed Study of Ocular Cicatricial Pemphigoid
Pathophysiology
Ocular cicatricial pemphigoid is an autoimmune condition in which the immune system attacks and damages the conjunctiva’s basement membrane. This immune attack causes chronic inflammation, which eventually scars (cicatrizes). The conjunctiva is a thin, transparent membrane that covers the white part of the eye (sclera) and lines the inside of the eyelids, helping to keep the ocular surface healthy and functioning properly.
Immune Mechanisms
- Autoantibodies: The pathogenesis of OCP is characterized by the production of autoantibodies against specific proteins in the basement membrane zone, including BP180 (type XVII collagen) and BP230. These autoantibodies cause a cascade of inflammatory responses.
- Complement Activation: The binding of autoantibodies activates the complement system, a component of the immune response that improves the ability to remove microbes and damaged cells. This activation leads to the recruitment of inflammatory cells to the conjunctiva, including neutrophils and macrophages.
- Cytokine Release: Inflammatory cells produce cytokines, which are signaling molecules that promote inflammation. This chronic inflammation causes tissue damage and fibrosis over time.
Stages of Disease
OCP progresses through several stages, each with increasing severity of symptoms and damage to the ocular surface.
- Early Stage: Non-specific symptoms of OCP include redness, irritation, and mild discomfort. Conjunctival inflammation is common, but it does not always result in visible scarring.
- Intermediate Stage: As the disease progresses, patients may experience more severe symptoms such as chronic conjunctivitis, conjunctival thickening, and symblepharon formation.
- Advanced Stage: In the advanced stages, extensive scarring causes forniceal shortening (a reduction in the depth of the conjunctival sac), entropion (inward turning of the eyelids), trichiasis (eyelashes rubbing against the cornea), and conjunctival keratinization. These changes can result in severe discomfort and visual impairment.
Symptoms
The symptoms of OCP differ depending on the stage of the disease, but commonly include:
- Redness and Irritation: Persistent redness and irritation of the eyes are common early signs of OCP.
- Dry Eyes: Scarring and inflammation can disrupt the normal function of the tear glands, causing chronic dry eye symptoms.
- Discharge: Patients may have mucous or purulent discharge from their eyes.
- Pain and Discomfort: As the disease progresses, pain and discomfort worsen, particularly with the appearance of symblepharon and trichiasis.
- Blurred Vision: Keratinization, scarring, and corneal damage can all have an impact on visual acuity.
- Light Sensitivity: Photophobia, or sensitivity to light, is common in the advanced stages of corneal involvement.
Risk Factors
Several factors can raise the risk of developing OCP, including:
- Age: OCP primarily affects older adults, usually over the age of 60.
- Gender: Some studies indicate a higher prevalence in females than males.
- Genetic Predisposition: Genetic factors may play a role, but the specific genetic markers are not well defined.
- Autoimmune Disorders: People with other autoimmune conditions may be more likely to develop OCP.
Complications
If not managed properly, OCP can cause a number of serious complications:
- Corneal Ulceration and Perforation: Chronic inflammation and mechanical trauma from trichiasis can cause corneal ulcers, which can progress to perforation if not treated.
- Blindness: Extensive scarring and corneal damage can cause significant vision loss, including blindness.
- Secondary Infections: Infections are more likely to occur on the disrupted ocular surface, complicating the disease and its treatment.
- Symblepharon Formation: Adhesions between the eyelid and the eyeball can limit eye movement and be uncomfortable.
Effects on Quality of Life
OCP can significantly impact a patient’s quality of life. Because of the disease’s chronic nature and progressive symptoms, it can cause significant physical and emotional distress. Patients may have difficulty performing daily tasks like reading, driving, and working. Persistent discomfort and visual impairment can lead to social isolation and depression.
Diagnostics
OCP is diagnosed using a combination of clinical, histopathological, and immunological tests. In the absence of other causes, the characteristic signs of chronic conjunctivitis with progressive scarring frequently raise the possibility of OCP. A conjunctival biopsy is typically required to confirm the presence of subepithelial fibrosis as well as linear immunoglobulin and complement component deposition along the basement membrane.
Diagnostic Techniques for Ocular Cicatricial Pemphigoid
Clinical Examination
- Patient History: A detailed patient history is required, with emphasis on symptoms, duration, and any previous episodes of conjunctivitis or other autoimmune conditions. Detailed questioning can help identify patterns that are consistent with OCP.
- Slit-Lamp Examination: A slit-lamp examination provides detailed views of the conjunctiva, cornea, and eyelids. This exam may reveal signs of inflammation, scarring, symblepharon, forniceal shortening, and corneal changes.
- Eyelid Eversion: Eversion of the eyelids aids in detecting early symblepharon formation and determining the extent of conjunctival involvement.
Histopathologic Examination
- Conjunctival Biopsy: A biopsy of the conjunctiva is required to diagnose OCP. The tissue sample is examined under a microscope to detect subepithelial fibrosis, chronic inflammation, and other histopathological characteristics.
- Direct Immunofluorescence (DIF): DIF analysis of the biopsy sample can detect the presence of immunoglobulins (IgG, IgA, and IgM) and complement components (C3) along the basement membrane zone. This linear deposition pattern indicates an autoimmune process.
Immunological Tests
- Serological Tests: Blood tests can detect autoantibodies associated with OCP. Antibodies to BP180 and BP230 are commonly detected using enzyme-linked immunosorbent assays (ELISA) and indirect immunofluorescence (IIF).
- T-Cell Studies: Advanced immunological studies may include analyzing T-cell subsets and cytokine profiles to better understand the underlying immune mechanisms that cause the disease.
Imaging Studies
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT generates high-resolution images of the conjunctiva and cornea, allowing for the assessment of scarring and structural changes.
- Ocular Surface Staining: Dyeing with fluorescein and lissamine green can highlight areas of epithelial damage and aid in determining the severity of ocular surface involvement.
Ocular Cicatricial Pemphigoid Treatment
Medical Management
- Corticosteroids: Because of their potent anti-inflammatory effects, corticosteroids are frequently the first line of treatment for OCP. They can be given topically, systemically, or via periocular injections, depending on the severity of the disease. While corticosteroids are effective in reducing inflammation, long-term use can result in serious side effects such as cataracts, glaucoma, and systemic complications.
- Immunosuppressive Agents: Immunosuppressive agents are used for patients who need long-term therapy or do not respond well to corticosteroids. These include medications such as azathioprine, methotrexate, and mycophenolate mofetil, which help reduce the immune system’s attack on the conjunctiva. Regular monitoring for potential side effects, such as liver damage and bone marrow suppression, is required.
- Biologic Agents: Rituximab and infliximab are examples of biologics that target specific immune system components. Rituximab, an anti-CD20 monoclonal antibody, has shown promise in treating refractory OCP by depleting the B-cells that produce autoantibodies. Infliximab, a TNF-alpha inhibitor, reduces inflammation. These agents provide targeted therapy, but they are costly and require close monitoring for side effects.
- Antibiotic Therapy: Tetracyclines, such as doxycycline, have anti-inflammatory properties and can help treat OCP. They help to lower matrix metalloproteinase activity, which is involved in tissue remodeling and scarring.
Surgical Management
- Symblepharon Lysis: Surgically removing the symblepharon can help restore normal anatomy and improve ocular surface function. This procedure may include the use of amniotic membrane grafts to prevent adhesions from reforming and to promote healing.
- Eyelid Surgery: Procedures to correct entropion (inward turning of the eyelids) and trichiasis (misdirected eyelashes) are critical for preventing further corneal damage and alleviating discomfort. These surgeries can significantly improve a patient’s quality of life by reducing mechanical discomfort.
- Corneal Transplantation: In severe cases of corneal scarring and vision loss, corneal transplantation (penetrating keratoplasty) may be required. However, the ongoing inflammatory process of OCP may limit the procedure’s success.
Emerging and Innovative Therapeutics
- Stem Cell Therapy: Research into the use of limbal stem cell transplantation shows promise for restoring the ocular surface in patients with severe limbal stem cell deficiency due to OCP. This approach seeks to regenerate damaged tissues and improve long-term results.
- Gene Therapy: Gene therapy is a growing field that aims to correct the underlying genetic defects that cause autoimmune responses. Although this approach is still experimental, it has the potential to treat autoimmune diseases such as OCP in the future.
- Targeted Molecular Therapies: Advances in understanding the molecular mechanisms of OCP are enabling the development of targeted therapies that inhibit specific pathways involved in inflammation and fibrosis. These include small molecule inhibitors and monoclonal antibodies that aim to disrupt the disease process at the cellular level.
Effective Ways to Manage and Prevent Ocular Cicatricial Pemphigoid
- Regular Monitoring: For people diagnosed with OCP, regular follow-ups with an ophthalmologist are essential for monitoring disease progression and adjusting treatment plans as needed. Early intervention can prevent serious complications.
- Avoiding Triggers: Identifying and avoiding potential environmental and chemical triggers that may exacerbate autoimmune responses can aid in symptom management and flare-up prevention.
- Protective Eyewear: Wearing protective eyewear can help shield the eyes from irritants and reduce the risk of injury, both of which can cause or worsen OCP.
- Moisture and Lubrication: Using preservative-free artificial tears and ocular lubricants on a regular basis can help maintain ocular surface health while also relieving dryness and irritation symptoms.
- Managing Associated Autoimmune Conditions: Patients with other autoimmune diseases should collaborate with their healthcare providers to manage these conditions, as well-managed systemic health can improve OCP.
- Healthy Diet: A well-balanced diet rich in anti-inflammatory foods like omega-3 fatty acids, fruits, and vegetables can improve overall immune health and potentially reduce inflammation.
- Stress Management: Chronic stress can worsen autoimmune disorders. Mindfulness, meditation, and regular physical activity can all help reduce stress and improve overall well-being.
- Education and Support: Participating in support groups and staying informed about OCP can provide emotional support as well as practical advice on how to manage the condition. Educating family members and caregivers about the disease can also strengthen support networks.
- Prompt Treatment of Eye Infections: Treating any eye infections as soon as possible can help prevent complications and reduce the risk of exacerbating OCP.
- Adherence to Treatment Plans: Strict adherence to prescribed treatment regimens, including medication schedules and follow-up appointments, is critical for successful OCP management.
Trusted Resources
Books
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis
- “Immunology of the Eye” by Steven W. J. Kowalski and C. Stephen Foster
- “Cicatricial Pemphigoid and Related Disorders” by Neil S. Sadick
Online Resources
- American Academy of Ophthalmology: AAO.org
- National Eye Institute: NEI.nih.gov
- Mayo Clinic: MayoClinic.org
- All About Vision: AllAboutVision.com
- MedlinePlus: MedlinePlus.gov
- Ocular Surface Society of Optometry: OSSO.org
- International Pemphigus and Pemphigoid Foundation: Pemphigus.org
- PubMed: PubMed.gov






