What is hypertensive retinopathy?
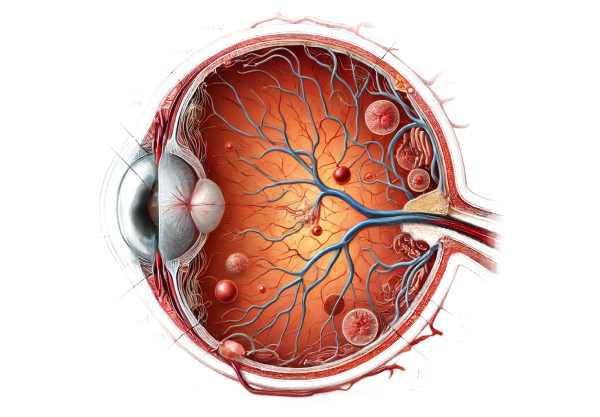
Chronic high blood pressure affects the retina, the light-sensitive tissue at the back of the eye, resulting in hypertensive retinopathy. Prolonged hypertension damages the blood vessels of the retina, resulting in a variety of visual symptoms and potential complications. The condition can cause vision impairment and, in severe cases, blindness. It is frequently detected during routine eye exams, as changes in retinal blood vessels can be a key indicator of systemic hypertension and other cardiovascular issues.
Hypertensive Retinopathy: Detailed Insights
Hypertensive retinopathy is a serious condition that results from high blood pressure affecting the retina’s microvasculature. The retina is essential for vision because it converts light into neural signals that the brain can use. When hypertension persists, it causes excessive pressure on the retinal arteries, resulting in a variety of pathological changes that can impair visual function.
Pathophysiology Of Hypertensive Retinopathy
The pathophysiological process of hypertensive retinopathy consists of several stages:
- Vasoconstriction: During the early stages, high blood pressure causes the retinal arterioles to constrict. This vasoconstriction is a compensatory mechanism that reduces blood flow while protecting the capillaries and arterioles.
- Sclerosis: Prolonged hypertension causes thickening and hardening of the arteriolar walls, which is known as arteriosclerosis. This process reduces the elasticity of blood vessels, making them stiffer and less capable of managing blood flow fluctuations.
- Exudation: As the disease progresses, increased vascular permeability causes plasma and blood components to leak into the retinal tissue. This leakage can produce hard exudates, cotton-wool spots (microinfarctions), and retinal edema.
- Hemorrhages: Weakened blood vessels can rupture, resulting in flame-shaped and dot-blot hemorrhages within the retinal layers. These hemorrhages further disrupt retinal function and have a significant impact on vision.
- Optic Disc Swelling: In severe cases, especially during hypertensive crises, the optic disc may swell (papilledema), indicating elevated intracranial pressure and significant systemic hypertension.
Clinical Feature and Grading
The severity of the retinal changes determines the grade of hypertensive retinopathy. The most widely used classification is the Keith-Wagener-Barker grading system:
- Grade 1: Mild retinal arteriolar narrowing and sclerosis, with no obvious symptoms. Frequently discovered incidentally during routine eye exams.
- Grade 2: More pronounced narrowing and focal constrictions of the retinal arterioles, frequently associated with changes in arteriovenous crossing (nicking). Patients may begin to experience mild visual disturbances.
- Grade 3: Evidence of retinal hemorrhages, cotton-wool spots, and hard exudates. Symptoms like blurred vision, visual field defects, and headaches appear more frequently.
- Grade 4: Severe retinopathy with optic disc swelling (papilledema), large hemorrhages, and hard exudates. This stage is commonly associated with hypertensive emergencies and carries a high risk of permanent vision loss.
Risk Factors and Causes
The main cause of hypertensive retinopathy is chronic high blood pressure. Several risk factors can worsen the condition:
- Genetic Predisposition: A family history of hypertension raises the possibility of developing hypertensive retinopathy.
- Age: Older adults are more vulnerable due to the cumulative effects of chronic hypertension.
- Lifestyle Factors: A poor diet, a lack of physical activity, smoking, and excessive alcohol consumption all contribute to hypertension and its associated retinal complications.
- Medical Conditions: Comorbidities like diabetes, hyperlipidemia, and chronic kidney disease can exacerbate hypertensive retinopathy.
Symptoms and Complications
Hypertensive retinopathy frequently progresses silently, with many patients remaining asymptomatic in the early stages. However, as the condition progresses, symptoms can include:
- Blurred Vision: Blurred vision can occur gradually or suddenly as a result of retinal edema and hemorrhages affecting the macula.
- Visual Field Defects: Damage to the retinal nerve fiber layer can result in scattered vision or blind spots.
- Headache: Severe hypertension can cause headaches and visual disturbances.
- Double Vision: Severe hypertension can cause increased intracranial pressure and double vision.
Hypertensive retinopathy can lead to severe complications such as:
- Retinal Detachment: Severe exudation and hemorrhage can result in retinal detachment, which requires immediate medical attention.
- Ischemic Optic Neuropathy: Reduced blood flow to the optic nerve can result in ischemic damage and permanent vision loss.
- Choroidopathy: Hypertension can damage the choroid, resulting in fluid accumulation and potential vision loss.
Systematic Implications
Hypertensive retinopathy is not only an ocular issue, but also a sign of systemic hypertension and cardiovascular risk. Retinal changes indicate the severity of hypertension and can predict the risk of stroke, heart attack, and other cardiovascular events. As a result, detecting hypertensive retinopathy may prompt further investigation and treatment of systemic hypertension.
Management and Prognosis
The prognosis of hypertensive retinopathy is heavily reliant on timely diagnosis and effective treatment of the underlying hypertension. Lifestyle changes and antihypertensive medications can help manage the early stages of the disease and potentially reverse some retinal changes. However, advanced stages can cause irreversible damage and significant visual impairment.
Methods for Diagnosing Hypertensive Retinopathy
A comprehensive eye examination and several specialized tests are required to diagnose hypertensive retinopathy. Here are the main diagnostic methods used:
Comprehensive Eye Examination
A thorough eye examination by an ophthalmologist or optometrist is required to diagnose hypertensive retinopathy. The exam includes:
- Visual Acuity Test: This test determines the clarity of vision at various distances. It aids in the detection of vision impairments caused by retinal changes.
- Fundus Examination: With an ophthalmoscope, the doctor examines the retina for signs of arteriolar narrowing, hemorrhages, exudates, and papilledema. The examination allows a clear view of the retinal blood vessels and optic disc.
Fundus Photography
Fundus photography entails taking detailed photographs of the retina with a specialized camera. These images make it possible to document retinal changes over time and track the progression of hypertensive retinopathy. Fundus photography is also useful in informing patients about their condition.
Optical Coherence Tomography(OCT)
OCT is a noninvasive imaging test that produces cross-sectional images of the retina. It aids in detecting and quantifying retinal edema, exudates, and other structural changes within the retinal layers. OCT is especially useful for detecting macular involvement in hypertensive retinopathy.
Fluorescein angiogram
Fluorescein angiography involves injecting a fluorescent dye into the bloodstream and photographing the dye as it travels through the retinal blood vessels. This test aids in detecting areas of leakage, non-perfusion, and other vascular abnormalities that are not visible during a routine fundus examination.
Blood Pressure Measurement
Diagnosing hypertensive retinopathy requires accurate blood pressure measurement. Blood pressure readings taken at various times and locations assist in determining the severity of hypertension and its relationship to retinal findings.
Lab Tests
Laboratory tests may be performed to identify underlying systemic conditions that may contribute to hypertensive retinopathy. These tests include:
- Blood Tests: Assessing kidney function, lipid profile, and blood glucose levels can help identify comorbid conditions like diabetes and hyperlipidemia.
- Urine Analysis: Detection of proteinuria and other abnormalities may indicate renal involvement in hypertension.
Visual Field Testing
Visual field testing assesses peripheral vision and aids in the detection of visual field defects caused by retinal damage or optic nerve involvement. This test is useful in determining the functional impact of hypertensive retinopathy on vision.
Advanced Hypertensive Retinopathy Therapies
The treatment of hypertensive retinopathy is primarily concerned with managing the underlying hypertension and addressing retinal complications. Here are the standard treatment options, as well as some novel and emerging therapies:
- Blood Pressure Control: The primary goal of treating hypertensive retinopathy is to achieve optimal blood pressure control. This involves:
- Antihypertensive Medications: Beta-blockers, ACE inhibitors, calcium channel blockers, and diuretics are common blood pressure medications. Medication selection is based on the individual’s overall health, coexisting conditions, and specific needs.
- Lifestyle Modifications: Patients are encouraged to live healthier lifestyles, such as eating a balanced diet low in sodium, engaging in regular physical activity, managing their weight, and quitting smoking. These changes can help to improve blood pressure control and overall cardiovascular health.
- Management of Comorbid Conditions: It is critical to treat coexisting conditions such as diabetes, hyperlipidemia, and renal disease. This may involve:
- Glycemic Control: Maintaining optimal blood sugar levels through medication, diet, and exercise can help diabetic patients avoid additional retinal damage.
- Lipid-Lowering Therapy: Statins and other lipid-lowering medications can lower cholesterol levels, which reduces the risk of vascular complications.
- Retinal Treatments: In cases of severe retinal damage, specific ocular treatments may be required:
- Laser Therapy: Laser photocoagulation can be used to close leaking blood vessels and prevent future hemorrhages and exudates.
- Intravitreal Injections: Drugs such as anti-VEGF (vascular endothelial growth factor) agents can be injected into the eye to reduce retinal swelling and neovascularization.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy is currently underway, with the goal of targeting specific genetic pathways involved in hypertensive retinopathy. This approach could provide personalized treatment based on a person’s genetic makeup.
- Advanced Imaging Techniques: Advancements in retinal imaging, such as adaptive optics and ultra-widefield imaging, enable earlier detection and more accurate monitoring of retinal changes. These techniques improve the ability to tailor treatments to the individual needs of the patient.
- Telemedicine: Telemedicine and remote monitoring tools can improve the management of hypertensive retinopathy. Patients can have their blood pressure monitored remotely and receive timely advice from healthcare providers without requiring frequent in-person visits.
- Artificial Intelligence (AI) and Machine Learning: AI algorithms are being developed to analyze retinal images and detect hypertensive retinopathy earlier than conventional methods. This technology can help to screen large populations and identify those at risk.
Combining these treatment options allows healthcare providers to effectively manage hypertensive retinopathy, reduce its impact on vision, and improve patients’ overall quality of life.
Best Practices for Avoiding Hypertensive Retinopathy
- Regular Blood Pressure Monitoring: Check your blood pressure on a regular basis to detect changes early. Home blood pressure monitors can help you keep track of your readings in between doctor visits.
- Take Prescribed Medications: Follow your healthcare provider’s instructions for taking all prescribed antihypertensive medications. Consistent medication use is critical for blood pressure management.
- Healthy Diet: Eat a diet low in sodium, saturated fat, and cholesterol. Include plenty of fruits, vegetables, whole grains, and lean protein. The DASH diet (Dietary Approaches to Stop Hypertension) is especially recommended for controlling blood pressure.
- Regular Exercise: Most days of the week, engage in at least 30 minutes of brisk walking, swimming, or cycling. Exercise promotes normal blood pressure and cardiovascular health.
- Weight Management: Maintaining a healthy weight helps to reduce the strain on your heart and vessels. Even a minor weight loss can have a big impact on blood pressure management.
- Limit Alcohol and Avoid Tobacco: Consume alcohol in moderation and avoid tobacco use. Both can worsen hypertension and increase the likelihood of cardiovascular complications.
- Stress Management: Try stress-reduction techniques like meditation, yoga, deep breathing exercises, and relaxing hobbies. Chronic stress can lead to high blood pressure.
- Regular Eye Exams: Schedule regular eye exams to detect hypertensive retinopathy at its early stages. Early intervention can help prevent serious retinal damage and vision loss.
- Manage Comorbid Conditions: Effectively manage other health conditions such as diabetes, high cholesterol, and kidney disease, which can all contribute to the development and progression of hypertensive retinopathy.
- Stay Informed: Learn more about hypertension and its complications. Understanding the risks and symptoms can help you take proactive steps to improve your health.
Individuals who follow these preventive measures can lower their risk of developing hypertensive retinopathy while also maintaining good eye and cardiovascular health.
Trusted Resources
Books
- “Retina” by Stephen J. Ryan
- “Vascular Diseases of the Retina” by A.M. Joussen, T.W. Gardner, B. Kirchhof, S.J. Ryan
- “Ophthalmology” by Myron Yanoff and Jay S. Duker
Online Resources
- American Academy of Ophthalmology (AAO)
- National Eye Institute (NEI)
- American Heart Association (AHA)
- Mayo Clinic – Hypertensive Retinopathy
- MedlinePlus – Hypertensive Retinopathy