Overview of Glaucomatocyclitic Crisis
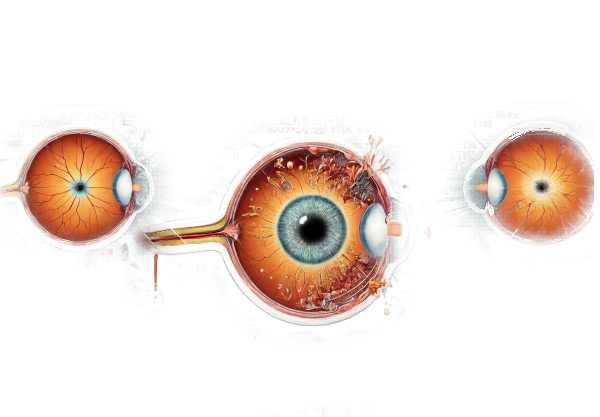
Glaucomatocyclitic crisis, also known as Posner-Schlossman Syndrome (PSS), is a rare eye condition marked by recurrent episodes of significantly elevated intraocular pressure (IOP) and mild anterior uveitis. PSS typically affects young to middle-aged adults and manifests as acute, self-limiting episodes of increased eye pressure with minimal inflammation. Regardless of how short-lived these episodes are, repeated occurrences can cause glaucomatous optic nerve damage over time. Understanding PSS’s pathophysiology, clinical features, and diagnostic challenges is critical for successful long-term vision loss management and prevention.
In-depth Look at Glaucomatocyclitic Crisis
Posner-Schlossman Syndrome (PSS), also known as glaucomatocyclitic crisis, is a distinct ocular condition characterized by glaucoma and anterior uveitis. PSS, first described by Posner and Schlossman in 1948, is characterized by unilateral, episodic attacks of high intraocular pressure (IOP) and mild inflammation in the anterior chamber of the eye. These episodes can last anywhere from a few hours to several weeks and often reoccur over months or years. Despite the typically benign nature of individual attacks, chronic or recurring episodes can cause cumulative damage to the optic nerve, resulting in glaucomatous changes and potential vision loss.
Pathophysiology
The exact pathophysiology of PSS is unknown, but several mechanisms have been proposed:
- Trabecular Meshwork Dysfunction: According to one theory, dysfunction of the trabecular meshwork, which drains aqueous humor from the eye, causes intermittent blockages and subsequent increases in IOP. This dysfunction may be transient and resolve spontaneously, explaining PSS’s episodic nature.
- Inflammatory Mediators: Another hypothesis proposes that mild anterior uveitis causes the release of inflammatory mediators such as prostaglandins. These mediators can increase vascular permeability and disrupt aqueous outflow, resulting in a temporary rise in IOP.
- Herpes Virus Infection: A growing body of evidence links PSS to herpes simplex virus (HSV) and cytomegalovirus (CMV) infections. These viruses can cause recurrent inflammation and trabecular meshwork dysfunction, which contributes to the episodic IOP elevation observed in PSS.
- Immune Dysregulation: Some researchers believe that PSS is caused by immune dysregulation, in which the body’s immune response intermittently targets ocular structures, resulting in inflammation and elevated IOP.
Clinical Presentation
PSS typically affects adults aged 20 to 50, with no clear gender preference. PSS is distinguished by recurrent, unilateral episodes of elevated IOP in the presence of mild anterior uveitis. Key clinical characteristics include:
- Elevated Intraocular Pressure: During an attack, IOP can range between 40 and 60 mmHg, which is significantly higher than the normal range of 10-21 mmHg. Elevated IOP frequently resolves spontaneously or with minimal treatment.
- Mild Anterior Uveitis: Unlike more severe forms of uveitis, inflammation in PSS is usually mild and limited to the anterior chamber. Symptoms may include mild eye redness, photophobia, and a feeling of ocular discomfort or ache.
- Corneal Edema: High IOP can cause corneal edema, resulting in blurry vision and halos around lights. This symptom usually resolves as the IOP drops.
- Open Angle: Gonioscopy during an attack usually shows an open anterior chamber angle, which distinguishes PSS from angle-closure glaucoma.
- Optic Nerve Changes: Recurrent episodes of elevated IOP can damage the optic nerve, resulting in an increased cup-to-disc ratio and glaucomatous visual field defects over time.
Differential Diagnosis
Several conditions can mimic the presentation of PSS, so differential diagnosis is crucial:
- Primary Open-Angle Glaucoma (POAG): POAG causes elevated IOP but lacks the episodic nature and mild uveitis found in PSS. POAG typically manifests as chronic, progressive optic neuropathy.
- Acute Angle-Closure Glaucoma: This condition is distinguished by a sudden, severe elevation in intraocular pressure (IOP), as well as a closed anterior chamber angle and more severe symptoms such as severe pain, nausea, or vomiting.
- Herpetic Anterior Uveitis: Similar to PSS, herpes simplex or herpes zoster anterior uveitis can cause recurrent episodes of elevated intraocular pressure and inflammation. Laboratory testing for viral DNA can help distinguish these conditions.
- Fuchs’ Heterochromic Iridocyclitis: This chronic condition also causes mild uveitis and elevated IOP, but it is more commonly associated with heterochromia (differences in iris color), cataract formation, and a lack of acute IOP spikes.
Complications
While individual episodes of PSS are usually self-limiting and respond well to treatment, chronic or recurrent attacks can cause serious complications.
- Glaucomatous Optic Neuropathy: If not treated properly, repeated episodes of elevated IOP can cause progressive optic nerve damage, resulting in visual field loss and, potentially, blindness.
- Secondary Glaucoma: Persistent changes in the trabecular meshwork and outflow pathways can lead to chronic secondary glaucoma, which requires long-term treatment.
- Cataract Formation: Chronic inflammation and long-term use of corticosteroids to treat PSS can lead to cataract development.
Understanding the pathophysiology, clinical presentation, and differential diagnosis of PSS is critical for timely diagnosis and effective management, which reduces the risk of long-term complications and preserves vision.
Diagnostic Tools for Glaucomatocyclitic Crisis
Posner-Schlossman Syndrome is diagnosed using a combination of clinical evaluation, imaging studies, and laboratory tests to confirm the diagnosis and rule out other conditions that present similarly.
Clinical Evaluation
- Comprehensive Eye Examination: A thorough eye exam is required to detect signs of high IOP, corneal edema, and anterior uveitis. Measuring IOP during an attack can reveal significantly elevated levels.
- Slit-Lamp Biomicroscopy: This technique detects mild anterior chamber inflammation, corneal edema, and keratic precipitates. These findings support the PSS diagnosis.
- Gonioscopy: Gonioscopy is used to inspect the anterior chamber angle. PSS is distinguished from angle-closure glaucoma by the presence of an open angle.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT can produce detailed images of the optic nerve head and retinal nerve fiber layer. It aids in the assessment of any glaucomatous damage caused by recurring IOP spikes.
- Ultrasound Biomicroscopy (UBM): UBM is useful for evaluating anterior segment structures and detecting subtle abnormalities in the trabecular meshwork or ciliary body.
Lab Tests
- Aqueous Humor Analysis: Examining the aqueous humor for inflammatory cells, herpes virus DNA (HSV or CMV), and other biomarkers can aid in the diagnosis and rule out herpetic anterior uveitis.
- Polymerase Chain Reaction (PCR) Testing: Testing aqueous humor samples for viral DNA (HSV, CMV) is critical when a viral etiology is suspected.
- Blood Tests: Comprehensive blood tests to rule out systemic conditions, such as autoimmune diseases or infections, which may present with similar ocular symptoms.
Glaucomatocyclitic Crisis Treatments
Posner-Schlossman Syndrome (PSS), also known as glaucomatocyclitic crisis, is treated by controlling inflammation during episodes and managing the acute elevation of intraocular pressure (IOP). Long-term management may be required to prevent recurrent attacks and reduce the risk of glaucomatous complications. Here are the conventional and emerging treatment options:
- Topical Medications: – Beta-Blockers: Timolol and betaxolol can reduce aqueous humor production and lower IOP.
- Prostaglandin Analogs: Medications such as latanoprost and bimatoprost promote the flow of aqueous humor.
- Alpha Agonists: Brimonidine reduces aqueous humor production while increasing outflow.
- Carbonic Anhydrase Inhibitors: Dorzolamide and brinzolamide lower aqueous humor production.
- Steroids: Topical corticosteroids like prednisolone acetate are used to reduce inflammation. In some cases, oral steroids may be prescribed to treat severe inflammation.
- Cycloplegics: Cycloplegic medications, such as cyclopentolate, can be used to relieve pain and prevent synechiae formation by paralyzing the ciliary body and relaxing the iris.
- Antiviral Agents: If a viral cause (e.g., herpes simplex virus, cytomegalovirus) is suspected or confirmed, antiviral medications like acyclovir or ganciclovir may be prescribed to treat the underlying infection.
Innovative and Emerging Therapies
- Selective Laser Trabeculoplasty (SLT): SLT may be considered for patients with recurrent PSS who do not respond well to medical treatment. It targets the trabecular meshwork to increase aqueous humor outflow and lower IOP.
- Minimally Invasive Glaucoma Surgery (MIGS): For patients with chronic high IOP and optic nerve damage, MIGS procedures such as the iStent or Xen Gel Stent provide less invasive surgical options for improving aqueous humor drainage.
- Immunomodulatory Therapy: New therapies that target specific inflammatory pathways are being investigated. Biologic agents that modulate the immune response may help manage inflammation in PSS.
- Gene Therapy: The goal of gene therapy research is to identify the genetic factors that cause trabecular meshwork dysfunction and inflammation. Despite being experimental, these therapies show promise for long-term management.
- Sustained-Release Drug Delivery: To improve adherence and efficacy, researchers are developing sustained-release ocular implants and punctal plugs that deliver anti-inflammatory and IOP-lowering medications over extended periods of time.
PSS management requires a personalized approach that takes into account the frequency and severity of attacks, underlying causes, and the patient’s overall health. Regular monitoring and follow-up are essential for avoiding long-term complications and preserving vision.
Tips to Avoid Glaucomatocyclitic Crisis (Posner-Schlossman Syndrome)
- Regular Eye Examinations: Have comprehensive eye exams to detect early signs of PSS and monitor IOP. Early detection enables timely intervention.
- Adherence to Treatment Plans: Carefully follow prescribed treatment regimens to manage acute episodes and prevent recurrence.
- Control Systemic Conditions: Treat systemic conditions like hypertension, diabetes, and viral infections, which can all contribute to ocular inflammation and high IOP.
- Avoid Triggers: Identify and avoid potential triggers that can cause PSS episodes, such as stress, lack of sleep, and exposure to bright lights.
- Use Protective Eyewear: Keep your eyes safe from injury and exposure to harmful substances that may cause inflammation.
- Maintain a Healthy Lifestyle: To improve overall eye health, engage in regular exercise, eat a well-balanced diet rich in antioxidants, and avoid smoking and alcohol consumption.
- Monitor for Symptoms: Keep an eye out for symptoms like eye pain, blurred vision, halos around lights, and eye redness. If you experience these symptoms, seek medical attention right away.
- Educate Yourself: Learn about PSS, including risk factors and symptoms. Knowledge enables you to take proactive steps towards managing your eye health.
- Use Antiviral Medication: If you have a history of herpes virus infections, talk to your doctor about prophylactic antiviral medication to reduce the risk of PSS episodes.
Individuals who follow these preventive measures can lower their risk of experiencing PSS episodes while also maintaining good ocular health.
Trusted Resources
Books
- “Primary Care Ophthalmology” by David B. Elliott
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
- “Ocular Inflammatory Disease and Uveitis Manual” by John J. Huang and James P. Dunn






