What is Juvenile Open Angle Glaucoma?
Juvenile open-angle glaucoma (JOAG) is a rare but serious eye condition that typically affects people aged three to forty. Unlike primary open-angle glaucoma, which is more common in older adults, JOAG develops earlier and frequently presents without symptoms in the early stages. If left untreated, this condition is characterized by increased intraocular pressure (IOP), which can cause optic nerve damage and vision loss. Understanding and early detection of JOAG are critical for avoiding irreversible damage and preserving visual function.
Detailed Examination of Juvenile Open-Angle Glaucoma
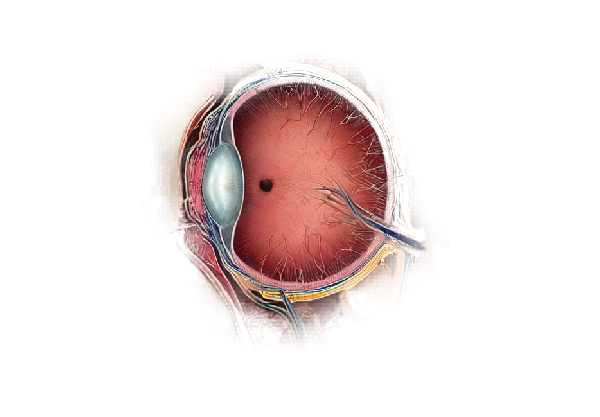
Juvenile open-angle glaucoma (JOAG) is a subset of primary open-angle glaucoma (POAG) that affects younger people, usually from childhood to early adulthood. It is a progressive condition that causes an increase in intraocular pressure (IOP) due to impaired aqueous humor drainage through the trabecular meshwork, the eye’s drainage system. Pressure buildup can damage the optic nerve, which transmits visual information from the eye to the brain.
Etiology and Pathophysiology
The exact cause of JOAG is unknown, but it is believed to be multifactorial, involving both genetic and environmental factors. Mutations in specific genes, such as the MYOC gene, have been associated with the development of JOAG. The MYOC gene encodes myocilin, a protein thought to be involved in trabecular meshwork function. Mutations in this gene can cause dysfunctional protein production, resulting in reduced aqueous humor outflow and elevated IOP.
In addition to genetic predispositions, ocular trauma, steroid use, and systemic conditions such as juvenile rheumatoid arthritis can all contribute to the development of JOAG. The pathophysiology of JOAG involves increased resistance to aqueous humor outflow through the trabecular meshwork, which results in elevated IOP. Chronic IOP elevation can cause progressive damage to the optic nerve fibers, resulting in glaucoma patients’ characteristic cupping of the optic disc.
Clinical Features and Symptoms
One of the challenges in diagnosing JOAG is that it is frequently asymptomatic in the early stages. Many patients do not exhibit any noticeable symptoms until significant optic nerve damage has occurred. When symptoms appear, they can include blurred vision, eye pain, halos around lights, and, in severe cases, loss of peripheral vision. However, these symptoms are not unique to JOAG and can be easily overlooked or attributed to other, less serious conditions.
As the disease progresses, JOAG can cause more severe visual field loss, usually beginning with peripheral vision and progressing to central vision. Advanced stages of JOAG can cause significant visual impairment and, if untreated, blindness.
Risk Factors
JOAG has several risk factors, including a family history of glaucoma, genetic mutations, and certain ethnicities. Individuals with a family history of glaucoma are more likely to develop the condition, indicating a hereditary component. Certain genetic mutations, such as those in the MYOC gene, have been found in families with a history of JOAG.
Ethnicity also plays a role, with research indicating that people of African, Latino, and Asian descent have a higher prevalence of JOAG than other populations. Furthermore, systemic conditions such as diabetes and high blood pressure increase the risk of developing glaucoma, including JOAG.
Differential Diagnosis
Differentiating JOAG from other types of glaucoma and ocular conditions is critical for effective treatment. Conditions like primary congenital glaucoma, secondary glaucoma, and other types of POAG must be considered. Primary congenital glaucoma usually appears in infancy with symptoms like photophobia, tearing, and buphthalmos (enlarged eye). Secondary glaucomas can result from trauma, inflammation, or steroid use, and distinguishing them from JOAG necessitates a thorough patient history and clinical examination.
Effects on Quality of Life
The impact of JOAG on quality of life can be significant, especially as the disease progresses and visual impairment worsens. Vision loss can impair daily activities like reading, driving, and recognizing faces, resulting in decreased independence and social isolation. The psychological toll of living with a chronic, progressive condition can also lead to anxiety and depression. Early diagnosis and intervention are critical for mitigating these effects and maintaining the patient’s quality of life.
Genetic Counseling and Testing
Given the hereditary nature of JOAG, genetic counseling and testing can help manage the condition. Genetic testing can help identify at-risk individuals, allowing for early detection and intervention, potentially slowing disease progression. Genetic counseling educates patients and their families about the condition, inheritance patterns, and potential consequences for other family members.
Identifying Juvenile Open-Angle Glaucoma
Diagnosing juvenile open-angle glaucoma necessitates a thorough and systematic approach that incorporates a variety of diagnostic tools and techniques. Early detection is critical for avoiding irreversible optic nerve damage and maintaining vision. The key diagnostic methods used in assessing JOAG are as follows:
Comprehensive Eye Examination
The first step in diagnosing JOAG is to have an ophthalmologist or optometrist perform a thorough eye examination. The examination includes a thorough patient history to identify risk factors such as family history, symptoms, and any prior ocular conditions or trauma. Visual acuity testing evaluates the patient’s ability to see at different distances and can reveal any existing vision impairment.
Intraocular Pressure Measurement
Measuring intraocular pressure (IOP) is an important part of the diagnostic process. Tonometry is the primary method for measuring IOP. The most common techniques are Goldmann applanation tonometry, which is considered the gold standard, and non-contact tonometry, which uses a puff of air to measure IOP. Elevated IOP is a defining feature of JOAG, and consistent readings above the normal range (10-21 mmHg) warrant further investigation.
Gonioscopy
Gonioscopy is a procedure that examines the anterior chamber angle, which contains the trabecular meshwork. This technique involves putting a specialized lens on the eye to see the angle structures. Gonioscopy can distinguish between open-angle and angle-closure glaucoma and detect any abnormalities in the drainage angle that may contribute to elevated IOP.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique for obtaining detailed cross-sectional images of the retina and optic nerve head. OCT is especially useful for determining the thickness of the retinal nerve fiber layer (RNFL) and identifying early signs of optic nerve damage. Changes in RNFL thickness can indicate glaucomatous damage even before visual field defects appear.
Visual Field Testing
Visual field testing, also known as perimetry, assesses both the patient’s peripheral and central vision. The Humphrey Field Analyzer is the most widely used automated static perimetry test. This test maps the patient’s visual field and detects any areas of vision loss. In JOAG, peripheral vision loss usually occurs first, and regular visual field testing is required to track disease progression.
Pachymetry
Pachymetry determines the thickness of the cornea, which can affect IOP readings. A thinner cornea may result in an underestimate of IOP, whereas a thicker cornea may result in an overestimation. Accurate corneal thickness measurements are critical for properly interpreting IOP readings and determining the risk of glaucoma progression.
Fundus Photography
Fundus photography captures detailed images of the optic nerve head and retina. These images enable the documentation and comparison of optic nerve changes over time. Serial fundus photographs can detect progressive cupping of the optic disc and thinning of the neuroretinal rim, both of which indicate glaucomatous damage.
Juvenile Open-Angle Glaucoma Treatment
The treatment of juvenile open-angle glaucoma (JOAG) focuses on lowering intraocular pressure (IOP) in order to prevent optic nerve damage and maintain vision. Medication, laser therapy, and surgical interventions are all treatment options, with emerging therapies showing promise for the future.
Medications
The first line of treatment for JOAG is usually the use of topical medications that lower IOP. These medications include:
- Prostaglandin analogs: Drugs like latanoprost and bimatoprost increase the outflow of aqueous humor, effectively lowering IOP.
- Beta-blockers: Medications such as timolol reduce the production of aqueous humor, lowering IOP.
- Alpha agonists: Drugs like brimonidine reduce aqueous humor production while increasing outflow.
- Carbonic anhydrase inhibitors: These can reduce aqueous humor production by using eye drops (e.g., dorzolamide) or orally (e.g., acetazolamide).
- Rho kinase inhibitors: A newer class of medications, including netarsudil, that lower IOP by increasing trabecular meshwork outflow.
Laser Therapy
When medications are insufficient, laser therapy may be used. The most common procedures are:
- Selective Laser Trabeculoplasty (SLT): SLT directs laser energy at the trabecular meshwork, increasing aqueous humor outflow and lowering IOP.
- Argon Laser Trabeculoplasty (ALT): Like SLT, ALT employs a different type of laser to improve drainage through the trabecular meshwork.
Surgical Interventions
Patients who do not respond well to medications or laser therapy may require surgical intervention. This includes:
- Trabeculectomy: This procedure creates a new drainage pathway for aqueous humor to exit the eye, which lowers IOP.
- Glaucoma Drainage Devices: The Ahmed valve or Baerveldt implant are used to facilitate the outflow of aqueous humor.
- Minimally Invasive Glaucoma Surgery (MIGS): Procedures such as the iStent or trabecular micro-bypass provide less invasive options for improving aqueous humor outflow and reducing recovery time.
Emerging Therapies
Emerging therapies for JOAG aim to target the underlying mechanisms while also providing neuroprotection to preserve the optic nerve. This includes:
- Gene Therapy: Research is currently underway to develop gene therapy approaches that can correct genetic defects associated with JOAG, such as MYOC mutations.
- Neuroprotective Agents: Compounds that protect optic nerve cells from damage are under investigation. These include brimonidine and other novel agents designed to prevent retinal ganglion cell apoptosis.
- Stem Cell Therapy: Investigating the ability of stem cells to regenerate damaged optic nerve fibers is a promising area of research with long-term implications.
Effective Ways to Improve and Prevent Juvenile Open-Angle Glaucoma
- Regular Eye Examinations: Have comprehensive eye exams every 1-2 years, especially if you have a family history of glaucoma or other risk factors. Early detection is critical to preventing damage.
- Maintain a Healthy Lifestyle: Exercise regularly, eat a well-balanced diet high in antioxidants, and maintain a healthy weight to improve overall eye health.
- Protect Eyes from Injury: Wear protective eyewear during sports or activities that may cause eye injury, as trauma can increase the risk of developing glaucoma.
- Manage Systemic Conditions: Control systemic conditions such as diabetes and high blood pressure, which can increase your risk of developing glaucoma.
- Avoid Smoking: Smoking has a negative impact on overall eye health and raises the risk of glaucoma. Avoiding tobacco products can help protect your vision.
- Restrict Caffeine Intake: Excessive caffeine consumption can temporarily increase IOP. To keep your eye pressure stable, consume caffeine in moderation.
- Follow Medication Regimens: If you have JOAG, stick to the medication regimens prescribed to you and see your eye doctor on a regular basis to monitor IOP and adjust treatment as needed.
- Stay Informed: Learn more about JOAG and stay up to date on new research and treatments. Knowing more allows you to make proactive decisions about your eye health.
Trusted Resources
Books
- “Glaucoma: A Patient’s Guide to the Disease” by Graham E. Trope
- “The Glaucoma Handbook: A Guide for Patients and Caregivers” by David L. Epstein






