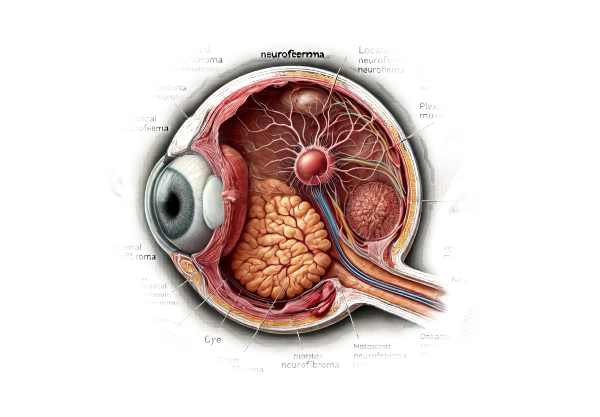
What is neurofibroma of the orbit?
Neurofibroma of the orbit is a benign tumor that develops from peripheral nerve sheath cells. It primarily affects the structures of the eye socket, or orbit, which include the muscles, nerves, and connective tissues that support the eyeball. This condition is frequently associated with neurofibromatosis type 1 (NF1), a genetic disorder in which tumors form on nerve tissue. While neurofibromas are typically not cancerous, their growth within the orbit can cause serious ocular complications such as vision loss, proptosis (eye bulging), and pain.
In-Depth Look at Orbital Neurofibromas
There are two types of neurofibromas: localized and plexiform. Both types can affect the orbit, but plexiform neurofibromas are more often associated with NF1 and are more widespread and invasive. The pathophysiology, clinical manifestations, risk factors, and potential complications of orbital neurofibromas provide a complete picture of this complex condition.
Pathophysiology
Schwann cells, which are responsible for peripheral nerve myelination, give rise to neurofibromas. In people with NF1, a mutation in the NF1 gene causes neurofibromin, a protein that normally regulates cell growth, to become inactive. This loss of function leads to uncontrolled cell proliferation and tumor formation. Neurofibromas in the orbit may affect a variety of structures, including the optic nerve, extraocular muscles, and orbital fat. Plexiform neurofibromas are particularly difficult to manage due to their diffuse nature and tendency to infiltrate surrounding tissues.
Clinical Features
The clinical presentation of orbital neurofibroma varies greatly depending on the size and location of the tumor. Common symptoms include:
- Proptosis: The most common presenting symptom, proptosis, results from the tumor’s mass effect pushing the eyeball forward.
- Vision Impairment: Tumors affecting the optic nerve or compressing the optic canal can cause progressive vision loss.
- Pain and Discomfort: Orbital neurofibromas can cause pain, especially when they compress nearby nerves or structures.
- Ptosis: Drooping of the upper eyelid can occur if the tumor affects the levator muscle or its innervation.
- Diplopia: Double vision can occur as a result of extraocular muscle involvement, which causes dysfunction and eye misalignment.
Associated Conditions
Orbital neurofibromas are frequently associated with neurofibromatosis type 1 (NF1), a genetic disorder characterized by numerous neurofibromas throughout the body. NF1 is an autosomal dominant condition, which means that a single mutation in the NF1 gene is sufficient to cause the disorder. Individuals with NF1 may exhibit other features, including:
- Café-au-lait Spots: Light brown skin patches that are frequently the first symptoms of NF1.
- Lisch Nodules: Slit-lamp examination reveals benign iris hamartomas.
- Freckling, especially in the axillary and inguinal regions.
- Other Tumors: People with NF1 are more likely to develop other types of tumors, such as malignant peripheral nerve sheath tumors (MPNST).
Complications
Orbital neurofibromas can cause a number of complications, primarily because of their location and potential for growth.
- Optic Nerve Compression: Neurofibromas affecting the optic nerve can cause progressive vision loss and blindness if not treated.
- Orbital Deformities: Large or invasive tumors can cause significant deformations of the orbital bones and surrounding structures, resulting in functional and cosmetic issues.
- Secondary Glaucoma: The tumor’s mass effect can cause increased intraocular pressure, which can lead to glaucoma.
- Intracranial Extension: In rare cases, orbital neurofibromas can spread into the intracranial cavity, creating significant surgical and therapeutic challenges.
Diagnostic methods
Ophthalmologists, radiologists, and pathologists must all collaborate to accurately diagnose orbital neurofibroma. Common diagnostic methods include the following:
Clinical Evaluation
A thorough clinical examination is the first step in diagnosing orbital neurofibroma. This evaluation includes:
- Patient history: Obtaining detailed information about the patient’s symptoms, duration, and any underlying conditions, such as NF1.
- Physical exam: A comprehensive examination of the eyes and surrounding structures to detect proptosis, ptosis, and other clinical signs. Visual acuity and field tests are also necessary to determine the impact on vision.
Imaging Studies
Orbital neurofibromas are difficult to diagnose and characterize without imaging. The most commonly used imaging modalities are:
- Magnetic Resonance Imaging (MRI) is the gold standard for diagnosing orbital neurofibromas. It produces detailed images of soft tissues, allowing for the evaluation of tumor size, extent, and involvement of nearby structures. T1-weighted and T2-weighted sequences, as well as gadolinium contrast, can help distinguish neurofibromas from other orbital masses.
- Computed Tomography (CT): CT scans are useful in determining bone involvement and orbital deformities. They produce high-resolution images of the bony orbit and can detect calcifications within the tumor.
Histopathologic Examination
While imaging studies can provide useful information, a definitive diagnosis often requires histopathological confirmation. This involves:
- Biopsy: Obtaining a tissue sample via surgical biopsy enables microscopic examination. The presence of spindle-shaped Schwann cells and collagenous stroma confirms the diagnosis of neurofibroma.
- Immunohistochemistry: Additional staining techniques, such as S-100 protein staining, can help with the diagnosis by emphasizing Schwann cell origin.
Differential Diagnosis
Several conditions can mimic the appearance of orbital neurofibroma, necessitating a careful differential diagnosis. These conditions include the following:
- Dermoid Cyst: A congenital lesion that can cause proptosis but is best identified by its characteristic fat content on imaging.
- Lymphoma: An orbital mass that can cause similar symptoms but has different imaging and histopathological characteristics.
- Orbital Cellulitis: An infection of the orbital tissues that can cause pain, swelling, and proptosis, but usually manifests as systemic infection.
- Meningioma: A tumor of the meninges that can spread to the orbit and cause similar symptoms, often distinguished by dural attachment on imaging.
Neurofibroma of the Orbit Treatment
The size, location, and symptoms of orbital neurofibroma determine the best course of treatment. While some neurofibromas may be stable and asymptomatic, others require treatment because they impair vision and ocular function.
Surgical Treatment
- Excision: Complete surgical removal of the neurofibroma is frequently the preferred treatment for symptomatic tumours. The goal is to reduce the pressure on the optic nerve and other orbital structures while preserving as much normal tissue as possible. Plexiform neurofibromas are infiltrative and close to critical structures, making surgical excision difficult.
- Debulking: When complete excision is not possible, debulking surgery may be used to reduce the tumor mass and relieve symptoms. This approach is frequently used for large plexiform neurofibromas that cannot be completely removed without causing significant damage to surrounding tissues.
- Orbital Decompression: For patients with severe proptosis or optic nerve compression, orbital decompression surgery may be required. This procedure removes bone or expands the orbital space to relieve pressure on the ocular structures.
Radiotherapy
- Stereotactic Radiosurgery: This precise type of radiation therapy targets the tumor and delivers high doses of radiation while minimizing exposure to healthy tissue. It is an option for tumors that are not surgically treatable or in cases where residual tumor remains after surgery.
- Conventional Radiotherapy: Conventional fractionated radiotherapy may be used in some cases, but it is less common due to the potential for long-term side effects on ocular tissues.
Medical Therapy
- MEK Inhibitors: Targeted therapies, such as MEK inhibitors (e.g., selumetinib), have shown promise in treating plexiform neurofibromas caused by NF1. These drugs work by inhibiting the MAPK/ERK pathway, which is frequently overactive in NF1-related tumors. In some patients, clinical trials showed tumor shrinkage and symptom relief.
- Pain Management: Patients who are experiencing pain as a result of their neurofibromas may require pain management strategies such as medications and nerve blocks.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy seeks to correct the underlying genetic mutation in NF1 that causes neurofibroma formation. While still in the experimental stage, these approaches have the potential to lead to future treatments that prevent or slow tumor growth.
- Immunotherapy: Immunotherapeutic approaches, such as checkpoint inhibitors and other immune-modulating agents, are being investigated for their ability to target and reduce neurofibroma growth.
Effective Methods to Improve and Avoid Neurofibroma in the Orbit
Orbital neurofibroma prevention requires proactive management of associated conditions as well as early detection strategies. Here are a few effective methods:
- Regular Monitoring: For people with NF1, regular ophthalmologic exams are essential for detecting early signs of orbital neurofibroma. Early diagnosis allows for more timely intervention and management.
- Genetic Counseling: Families with a history of NF1 should seek genetic counseling to better understand their risk and explore options for early detection and treatment of neurofibromas.
- Healthy Lifestyle: Leading a healthy lifestyle that includes a balanced diet and regular exercise can improve overall health and potentially reduce complications associated with NF1.
- Trauma Avoidance: Keeping the eyes and orbit out of harm’s way can help prevent neurofibromas from getting worse. Wear protective eyewear when participating in activities that may cause injury.
- Pain Management: For people with symptomatic neurofibromas, effective pain management strategies can improve their quality of life and lessen the condition’s impact on daily activities.
- Regular Follow-Up: Consistent follow-up with healthcare providers who specialize in NF1 and neurofibromas ensures that any changes in the condition are addressed quickly.
- Awareness and Education: Educating patients and families on the signs and symptoms of orbital neurofibromas can lead to earlier detection and treatment.
- Support Groups: Joining a support group for people with NF1 and neurofibromas can provide emotional support, resources, and information on the most recent treatment options and research advances.
Trusted Resources
Books
- “Neurofibromatosis: A Handbook for Patients, Families, and Health Care Professionals” by Bruce R. Korf and Allan E. Rubenstein
- “The Eye in Systemic Disease” by Frederick T. Fraunfelder
- “Clinical Neuro-Ophthalmology” by Frank B. Walsh






