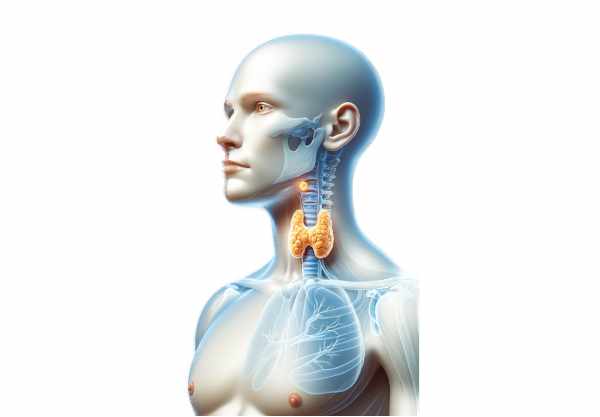
The parathyroid glands, though tiny, play a monumental role in regulating the body’s calcium and phosphorus balance, which is crucial for bone health, neuromuscular function, and overall metabolism. Located behind the thyroid gland, these small, oval-shaped structures secrete parathyroid hormone (PTH), a key regulator in calcium homeostasis. Disturbances in their function can lead to significant health issues ranging from osteoporosis and kidney stones to neuromuscular disorders. This comprehensive guide delves into the detailed anatomy, physiological roles, common disorders, diagnostic methods, and modern treatments of the parathyroid glands, along with lifestyle and nutritional tips to maintain their health.
Table of Contents
- Structural Insights
- Physiological Roles
- Common Disorders
- Diagnostic Methods
- Treatment Strategies
- Nutritional & Supplementary Support
- Lifestyle & Preventive Practices
- Trusted Resources
- Frequently Asked Questions
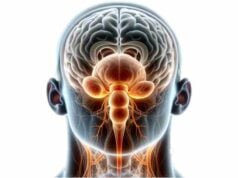
Structural Insights
The parathyroid glands are minute yet mighty components of the endocrine system. Typically, four in number, these glands are most commonly located on the posterior aspect of the thyroid gland in the neck. However, anatomical variations do occur—with some individuals presenting with supernumerary or ectopic parathyroid tissues, sometimes found in the mediastinum or along the carotid sheath.
General Location and Morphology
- Anatomical Position:
The parathyroid glands are generally found adjacent to the thyroid gland. They are arranged in two pairs: the superior pair and the inferior pair. The inferior parathyroid glands share a developmental pathway with the thymus, often descending further into the neck, while the superior glands remain near the upper pole of the thyroid. - Size and Appearance:
Despite their small size—each gland typically measures 3–5 mm in diameter and weighs between 30–50 mg—the parathyroid glands have a profound impact on calcium regulation. They exhibit an oval or bean-like shape and a characteristic yellowish-brown coloration, reflecting their high lipid content.
Microscopic Anatomy
At the microscopic level, the parathyroid glands reveal a cellular composition critical to their function:
- Chief Cells:
Predominantly, the parathyroid is made up of chief cells. These cells are responsible for synthesizing and secreting parathyroid hormone (PTH). Under the microscope, chief cells appear small and polygonal with centrally placed nuclei and pale cytoplasm due to the presence of glycogen. - Oxyphil Cells:
Larger than chief cells, oxyphil cells are rich in mitochondria, giving them a distinctive eosinophilic (pink) appearance. Although their exact role remains less clear, oxyphil cells are believed to contribute to the metabolic activity of the gland, and their numbers tend to increase with age.
Supporting Structures
- Capsule and Stroma:
A delicate connective tissue capsule envelops the parathyroid glands, extending inward to form septa that subdivide the gland into small lobules. This stroma not only provides structural support but also houses a dense network of blood vessels crucial for hormone secretion. - Vascular Supply:
The blood supply is robust, primarily delivered by branches of the inferior thyroid arteries, with contributions from the superior thyroid arteries. This rich vascularization is essential for rapid hormone release into the bloodstream. - Lymphatic and Neural Networks:
Lymphatic vessels from the parathyroid drain into the deep cervical and paratracheal lymph nodes, while autonomic nerve fibers—mostly from the cervical sympathetic ganglia—provide vasomotor regulation, ensuring proper blood flow through the glands.
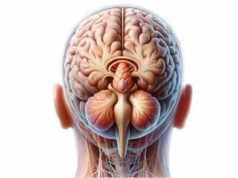
Embryological Development
During embryogenesis, the parathyroid glands develop from the third and fourth pharyngeal pouches:
- Third Pharyngeal Pouch:
Gives rise to the inferior parathyroid glands and thymus. As development proceeds, the inferior glands descend, sometimes resulting in ectopic locations. - Fourth Pharyngeal Pouch:
Develops into the superior parathyroid glands, which migrate less extensively.
These developmental pathways explain the common anatomical variations observed in clinical practice.
Physiological Roles
The paramount function of the parathyroid glands is to maintain calcium homeostasis, which is essential for neuromuscular activity, bone metabolism, and various cellular processes.
Regulation of Calcium Homeostasis
Parathyroid Hormone (PTH) Secretion
- Calcium-Sensing Mechanism:
Chief cells are equipped with calcium-sensing receptors (CaSR) that monitor blood calcium levels. When calcium levels drop, these receptors stimulate the secretion of PTH; conversely, high calcium levels suppress PTH release. - Synthesis and Release:
PTH is synthesized initially as a preprohormone, converted to pro-PTH, and finally processed into mature PTH, which is stored in secretory granules until needed. When released, PTH acts on multiple target organs to restore calcium balance.
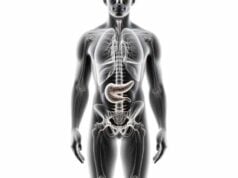
Mechanisms of PTH Action
PTH exerts its effects primarily through its actions on three major organs:
- Bone:
PTH stimulates osteoclast activity indirectly by acting on osteoblasts, promoting bone resorption and the release of calcium (and phosphate) into the bloodstream. This process is tightly regulated to maintain bone density while ensuring adequate serum calcium levels. - Kidneys:
In the kidneys, PTH:
- Increases calcium reabsorption in the distal convoluted tubules, thus reducing urinary calcium loss.
- Decreases phosphate reabsorption in the proximal tubules, promoting phosphate excretion.
- Stimulates the conversion of 25-hydroxyvitamin D to calcitriol, the active form of vitamin D, which in turn enhances intestinal calcium absorption.
- Intestines:
Although the intestines are not direct targets of PTH, the hormone’s effect on vitamin D activation significantly enhances the absorption of calcium and phosphate from the diet, further contributing to serum calcium regulation.
Integration of Hormonal Feedback
PTH operates within a negative feedback loop:
- Low Serum Calcium:
Triggers increased PTH secretion, which acts to raise calcium levels through bone resorption, kidney reabsorption, and enhanced intestinal absorption. - High Serum Calcium:
Inhibits further PTH release, preventing hypercalcemia.
This dynamic balance is essential for maintaining optimal calcium levels and ensuring proper neuromuscular and skeletal function.
Interaction with Other Hormones
- Calcitonin:
Secreted by the thyroid’s parafollicular (C) cells, calcitonin antagonizes the effects of PTH by inhibiting osteoclast activity and reducing blood calcium levels. - Vitamin D (Calcitriol):
Calcitriol, whose synthesis is stimulated by PTH, enhances calcium absorption from the gut and works synergistically with PTH to regulate serum calcium levels.
Physiological Impact
Proper parathyroid function is vital for:
- Neuromuscular Function:
Adequate calcium levels are critical for nerve impulse transmission and muscle contraction. - Bone Integrity:
Regulation of bone remodeling is essential to prevent osteoporosis and other bone diseases. - Cellular Signaling:
Calcium serves as a secondary messenger in various intracellular processes, influencing everything from muscle contraction to hormone secretion.
Common Disorders
Disruptions in parathyroid function can lead to serious health problems, often manifesting as imbalances in calcium and phosphate homeostasis. The primary conditions affecting the parathyroid glands include hyperparathyroidism, hypoparathyroidism, and parathyroid cancer.
Hyperparathyroidism
Primary Hyperparathyroidism
- Etiology:
Most commonly caused by a benign adenoma in one of the parathyroid glands, primary hyperparathyroidism results in excessive PTH secretion. - Clinical Features:
Patients typically present with hypercalcemia, bone pain, kidney stones, gastrointestinal disturbances, and neuropsychiatric symptoms. - Diagnosis:
Elevated serum calcium coupled with high PTH levels is diagnostic. Imaging such as ultrasound and sestamibi scans localize abnormal tissue. - Management:
The primary treatment is surgical removal of the overactive gland(s). In non-surgical candidates, calcimimetics or bisphosphonates may be used.
Secondary Hyperparathyroidism
- Etiology:
Occurs as a compensatory mechanism in response to chronic hypocalcemia, commonly seen in chronic kidney disease or vitamin D deficiency. - Clinical Features:
Despite low or normal calcium levels, PTH levels are elevated, leading to bone pain, skeletal abnormalities, and soft tissue calcifications. - Management:
Focuses on treating the underlying cause, with vitamin D supplementation, phosphate binders, and sometimes calcimimetics.
Tertiary Hyperparathyroidism
- Description:
After prolonged secondary hyperparathyroidism, the parathyroid glands may become autonomously hyperfunctional even when calcium levels normalize. - Clinical Impact:
Patients experience persistent hypercalcemia with symptoms similar to primary hyperparathyroidism. - Treatment:
Surgical removal of hyperplastic parathyroid tissue is often necessary.
Hypoparathyroidism
- Etiology:
Most commonly results from inadvertent removal or damage to the parathyroid glands during thyroid or neck surgery. Autoimmune processes and genetic disorders can also lead to hypoparathyroidism. - Clinical Features:
Characterized by hypocalcemia, which may manifest as muscle cramps, tetany, paresthesia, seizures, and cardiac arrhythmias. - Diagnosis:
Low serum calcium, low PTH, and high phosphate levels are diagnostic. - Management:
Treatment includes calcium and active vitamin D supplementation, and in refractory cases, recombinant PTH therapy may be considered.
Parathyroid Cancer
- Rarity and Aggressiveness:
Parathyroid cancer is a rare but aggressive malignancy that typically presents with severe hypercalcemia. - Clinical Features:
Symptoms include significant hypercalcemia, bone pain, kidney stones, and a palpable neck mass. - Diagnosis:
Based on markedly elevated calcium and PTH levels, along with imaging and histopathological confirmation. - Management:
The primary treatment is surgical resection, often involving en bloc removal of the tumor and surrounding tissues. Adjunct therapies such as radiation and chemotherapy may be considered, although the prognosis remains guarded.
Pseudohypoparathyroidism
- Definition:
A genetic disorder characterized by resistance to PTH in target tissues, resulting in hypocalcemia and hyperphosphatemia despite elevated PTH levels. - Clinical Features:
Patients may present with physical features such as short stature, obesity, and skeletal abnormalities. - Diagnosis:
Laboratory findings show high PTH with low calcium and high phosphate, confirmed by genetic testing for GNAS mutations. - Management:
Focuses on correcting the calcium-phosphate imbalance through supplementation and dietary modifications.
Diagnostic Methods
A meticulous diagnostic approach is essential for identifying parathyroid disorders, as early detection can significantly improve treatment outcomes. The evaluation process includes clinical assessments, laboratory tests, imaging studies, and sometimes invasive procedures.
Clinical Evaluation
- History and Physical Examination:
A detailed history addresses symptoms such as bone pain, muscle cramps, kidney stones, fatigue, and neuropsychiatric disturbances. Physical examination may reveal signs of hypercalcemia or hypocalcemia, including dry skin, muscle spasms, or a palpable neck mass. - Neurological and Musculoskeletal Assessment:
Evaluating muscle strength, reflexes, and bone tenderness can provide additional clues regarding calcium imbalances.
Laboratory Testing
- Serum Calcium and Phosphate Levels:
Measurement of these electrolytes is fundamental. Elevated calcium with high PTH suggests hyperparathyroidism, while low calcium and low PTH indicate hypoparathyroidism. - Parathyroid Hormone (PTH) Assays:
PTH levels are crucial for assessing parathyroid activity. Elevated PTH with hypercalcemia typically indicates primary hyperparathyroidism. - Vitamin D Levels:
Assessing 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels helps differentiate between primary parathyroid disorders and secondary changes due to vitamin D deficiency. - Urinary Calcium Excretion:
A 24-hour urinary calcium test can help distinguish primary hyperparathyroidism from familial hypocalciuric hypercalcemia.
Imaging Modalities
- Neck Ultrasound:
A non-invasive imaging tool that helps visualize the parathyroid glands, particularly useful for detecting enlarged or adenomatous glands. - Sestamibi Scans:
Technetium-99m sestamibi scintigraphy is a nuclear medicine technique that identifies hyperfunctioning parathyroid tissue by its increased uptake of the radiotracer. - 4D CT Scans:
Four-dimensional CT imaging provides detailed anatomical and functional information, enabling precise localization of abnormal parathyroid tissue. - MRI:
Although used less frequently, MRI can be helpful in cases where ultrasound and sestamibi scans are inconclusive, especially in detecting ectopic glands.
Genetic Testing
- Hereditary Syndromes:
Genetic testing for mutations associated with MEN1, MEN2A, and familial isolated hyperparathyroidism is recommended for patients with a family history or early-onset disease. - Pseudohypoparathyroidism:
Testing for GNAS gene mutations confirms the diagnosis in suspected cases.
Bone Density Evaluation
- DEXA Scans:
Dual-energy X-ray absorptiometry is used to assess bone mineral density in patients with long-standing parathyroid disorders, particularly in hyperparathyroidism where bone resorption is accelerated.
Intraoperative Monitoring
- Rapid PTH Assay:
During parathyroid surgery, intraoperative PTH monitoring confirms the successful removal of hyperactive tissue by showing a significant drop in PTH levels shortly after excision.
Treatment Strategies
Effective treatment of parathyroid disorders depends on the underlying pathology and the severity of the condition. Treatment modalities range from conservative medical management and lifestyle modifications to surgical interventions and advanced therapies.
Medical Management
For Hypoparathyroidism
- Calcium and Vitamin D Supplementation:
Essential for maintaining serum calcium levels, these supplements are the mainstay of treatment for hypoparathyroidism. Dosages are adjusted based on regular blood test monitoring. - Phosphate Binders:
Used to reduce dietary phosphate absorption in patients with high phosphate levels, thereby preventing complications associated with hypoparathyroidism. - Recombinant PTH Therapy:
In refractory cases, recombinant human PTH can be administered to better regulate calcium homeostasis.
For Hyperparathyroidism
- Calcimimetics:
Medications such as cinacalcet enhance the sensitivity of calcium-sensing receptors on the parathyroid glands, thereby reducing PTH secretion and normalizing serum calcium levels. - Bisphosphonates:
These drugs are sometimes used to manage bone loss associated with hyperparathyroidism, reducing the risk of fractures. - Observation:
In mild cases of hyperparathyroidism, especially in asymptomatic patients, careful monitoring may be appropriate if surgical risks are high.
Surgical Interventions
Parathyroidectomy
Surgical removal of the abnormal parathyroid gland(s) is the definitive treatment for primary hyperparathyroidism, parathyroid cancer, and tertiary hyperparathyroidism.
- Minimally Invasive Parathyroidectomy (MIP):
A targeted procedure using a small incision and guided by preoperative imaging and intraoperative PTH monitoring. This approach minimizes tissue trauma and shortens recovery. - Bilateral Neck Exploration:
When imaging is inconclusive or multiple glands are suspected of being abnormal, this technique allows the surgeon to examine all parathyroid tissues. - En Bloc Resection:
In cases of parathyroid carcinoma, a more extensive removal of the tumor along with surrounding tissues and lymph nodes is necessary to reduce recurrence.
Autotransplantation
In patients undergoing extensive parathyroidectomy, a portion of healthy parathyroid tissue may be transplanted to a more accessible location (often the forearm) to preserve some parathyroid function and reduce the risk of permanent hypoparathyroidism.
Advanced Therapies
Minimally Invasive Techniques
- Intraoperative PTH Monitoring:
This technique is crucial during surgery to ensure that all hyperfunctioning tissue has been removed, as evidenced by a significant drop in PTH levels.
Emerging Interventions
- Targeted Molecular Therapy:
For parathyroid cancer, novel therapies targeting specific genetic mutations are under investigation. - Radiofrequency Ablation:
Minimally invasive ablation techniques may be used for certain benign parathyroid lesions in patients who are not surgical candidates.
Nutritional & Supplementary Support
Optimal parathyroid function is intimately linked with proper nutrition and supplementation. Supporting the parathyroid glands with the right nutrients can help maintain calcium homeostasis and overall bone and neuromuscular health.
Essential Nutrients and Vitamins
- Calcium:
Critical for maintaining healthy bones and proper neuromuscular function, calcium supplementation is essential for patients with hypoparathyroidism. - Vitamin D:
Enhances calcium absorption from the gut and is crucial in regulating blood calcium levels. Adequate vitamin D levels also support overall bone density. - Magnesium:
Magnesium plays a role in PTH secretion and action. Sufficient magnesium intake is necessary for effective calcium absorption and utilization. - B Vitamins:
Vitamins B6, B12, and folic acid support metabolic processes and contribute to cellular repair, indirectly benefiting parathyroid function. - Antioxidants (Vitamins C & E):
These antioxidants protect parathyroid cells from oxidative stress and support cellular health.
Herbal Supplements
- Alfalfa:
Rich in calcium, magnesium, and vitamin K, alfalfa supports bone health and may help maintain balanced serum calcium levels. - Horsetail:
A natural source of silica, horsetail can improve calcium absorption and promote the structural integrity of bones. - Nettle:
Nutrient-dense and high in minerals, nettle supports healthy PTH levels and overall bone metabolism.
Enzymes and Cellular Support
- Pancreatic Enzymes:
Though primarily used for digestive support, these enzymes can improve overall nutrient absorption, thereby indirectly supporting parathyroid health. - Alpha-Lipoic Acid:
This potent antioxidant improves cellular energy production and protects against oxidative damage in parathyroid tissues. - Coenzyme Q10 (CoQ10):
Essential for cellular energy production, CoQ10 shields parathyroid cells from oxidative stress and supports endocrine function.
Hormonal Support
- Calcifediol:
As a precursor to active vitamin D, calcifediol supplementation can be beneficial in individuals with impaired kidney function, ensuring that adequate levels of active vitamin D are maintained. - Adaptogenic Hormones:
Supporting overall endocrine health with hormones such as DHEA may indirectly benefit parathyroid function, particularly in the context of aging or chronic disease.
Probiotics
- Gut Health and Calcium Absorption:
A healthy gut microbiome plays a role in nutrient absorption, including calcium. Probiotics help maintain gut health, which in turn supports the parathyroid glands and bone metabolism.
Lifestyle & Preventive Practices
Maintaining parathyroid health requires an integrative approach that combines dietary management, physical activity, and regular health monitoring. By adopting a healthy lifestyle, individuals can promote endocrine balance and reduce the risk of parathyroid-related disorders.
- Adopt a Balanced Diet:
- Include plenty of calcium-rich foods such as dairy products, leafy greens, and fortified foods.
- Emphasize whole, unprocessed foods that provide essential vitamins, minerals, and antioxidants.
- Exercise Regularly:
- Engage in weight-bearing and resistance exercises to promote bone health.
- Aim for at least 150 minutes of moderate exercise per week to maintain overall metabolic health and enhance calcium utilization.
- Manage Stress Effectively:
- Practice mindfulness, meditation, yoga, or deep breathing exercises to lower stress levels, which can affect endocrine function.
- Regular stress management contributes to hormonal balance and overall wellness.
- Ensure Adequate Sleep:
- Aim for 7–9 hours of quality sleep per night to support hormonal regulation and cellular repair.
- Establish a consistent sleep routine and create a conducive sleep environment.
- Stay Hydrated:
- Drink plenty of water throughout the day to support metabolic processes and kidney function, which in turn helps regulate serum calcium.
- Proper hydration can also reduce the risk of kidney stones, a complication of hyperparathyroidism.
- Monitor Nutrient Intake:
- Ensure you’re consuming adequate amounts of calcium, vitamin D, magnesium, and other key nutrients.
- Consider regular nutritional assessments and consult with a healthcare provider about supplementation if needed.
- Regular Health Check-Ups:
- Schedule routine visits with your healthcare provider to monitor parathyroid function and bone density.
- Early detection of any abnormalities can lead to more effective intervention and better long-term outcomes.
- Limit Processed Foods and Phosphorus:
- Reduce consumption of processed foods and beverages high in phosphorus, which can disrupt calcium balance.
- Choose whole, natural foods to support endocrine health.
- Avoid Smoking and Limit Alcohol:
- Smoking and excessive alcohol consumption can negatively affect bone health and endocrine function.
- Maintain a healthy lifestyle by avoiding these substances.
- Educate Yourself:
- Stay informed about parathyroid health through reliable sources and continuous learning.
- Engage with support groups or online communities to share experiences and tips.
Trusted Resources
For those seeking additional information on parathyroid gland health, the following resources provide valuable insights from clinical, academic, and patient perspectives.
Recommended Books
- “The Parathyroid Gland: Physiology and Pathophysiology” by John P. Bilezikian:
This comprehensive volume covers everything from the fundamental physiology of the parathyroid glands to the clinical management of parathyroid disorders. - “Vitamin D: Physiology, Molecular Biology, and Clinical Applications” by Michael F. Holick:
An essential resource for understanding the role of vitamin D in calcium homeostasis and its impact on parathyroid function. - “Clinical Guide to Parathyroid Disorders: Diagnosis and Management” by Aliya A. Khan:
A practical guide offering evidence-based approaches to diagnosing and managing parathyroid gland diseases.
Academic Journals
- Journal of Clinical Endocrinology & Metabolism (JCEM):
A leading journal that publishes cutting-edge research on endocrine disorders, including parathyroid diseases. - Bone:
This journal focuses on bone biology and metabolism, providing valuable insights into the effects of parathyroid hormone on bone health.
Mobile Applications
- Calcium Pro:
An app designed to help users track calcium intake, manage supplements, and monitor symptoms related to parathyroid disorders. - MyFitnessPal:
A comprehensive nutrition and fitness tracker that assists in maintaining a balanced diet crucial for parathyroid and bone health. - Medscape:
A valuable resource for healthcare professionals and patients alike, offering up-to-date medical news, clinical guidelines, and information on parathyroid conditions.
Frequently Asked Questions
What is the primary function of the parathyroid glands?
The parathyroid glands regulate calcium and phosphate balance in the body by secreting parathyroid hormone (PTH), which acts on bones, kidneys, and indirectly on the intestines to maintain optimal serum calcium levels.
How does parathyroid hormone (PTH) affect the body?
PTH increases blood calcium levels by stimulating bone resorption, enhancing calcium reabsorption in the kidneys, and promoting the conversion of vitamin D into its active form, which increases intestinal calcium absorption.
What are common signs of hyperparathyroidism?
Symptoms of hyperparathyroidism include high blood calcium levels, bone pain, kidney stones, gastrointestinal disturbances, and neuropsychiatric issues such as fatigue and depression.
How is hypoparathyroidism diagnosed and treated?
Hypoparathyroidism is diagnosed by low serum calcium, low PTH, and high phosphate levels. Treatment typically involves calcium and vitamin D supplementation, and in severe cases, recombinant PTH therapy may be used.
What lifestyle changes can support parathyroid health?
A balanced diet rich in calcium, vitamin D, and magnesium; regular exercise; proper hydration; stress management; and avoiding smoking and excessive alcohol are key lifestyle practices that help maintain healthy parathyroid function.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider regarding any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to maintain optimal parathyroid health.