What is internuclear ophthalmoplegia?
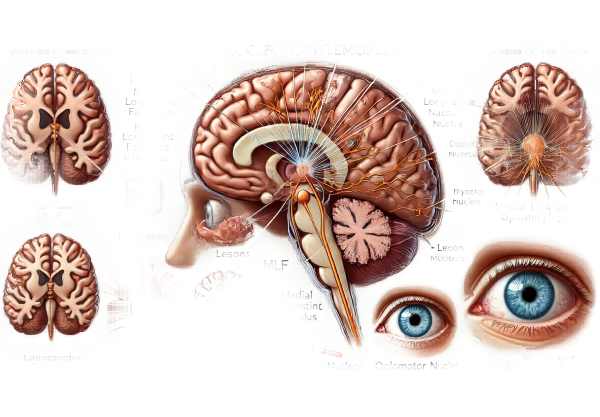
Internuclear Ophthalmoplegia (INO) is a rare ocular motility disorder defined by an inability to coordinate horizontal eye movements. A lesion in the medial longitudinal fasciculus (MLF), a critical brainstem pathway that connects the nuclei of cranial nerves III (oculomotor) and VI (abducens), causes it. This condition causes the affected eye’s adduction (movement towards the nose) to be impaired, as well as nystagmus (involuntary rapid movement) of the abducting eye. INO frequently indicates an underlying neurological condition, such as multiple sclerosis (MS) in younger patients or stroke in older patients.
Comprehensive Study of Internuclear Ophthalmoplegia
Internuclear Ophthalmoplegia (INO) is a complex disorder affecting the intricate network of neurons that coordinate eye movements. The medial longitudinal fasciculus (MLF) connects the abducens nucleus in the pons to the oculomotor nucleus in the midbrain, which is critical for coordination. A lesion in the MLF disrupts this connection, resulting in the distinctive features of INO.
Pathophysiology
The pathophysiology of INO revolves around the disruption of the MLF, which is necessary for horizontal gaze coordination. The MLF sends signals from the abducens nucleus, which controls the lateral rectus muscle (responsible for eye abduction), to the oculomotor nucleus, which controls the medial rectus muscle (in charge of eye adduction). When the MLF is damaged, the ipsilateral eye’s adduction is impaired, while the contralateral eye develops abduction nystagmus.
Causes
INO can occur from a variety of causes, the most common of which are:
- Multiple Sclerosis (MS): In younger patients, particularly those under 50, MS is the leading cause of INO. MS’s demyelinating lesions frequently target the MLF.
- Stroke: Cerebrovascular accidents (strokes) are a common cause of death among the elderly. Ischemic lesions in the brainstem can interrupt the MLF pathway.
- Trauma: Head injuries can damage the brainstem, causing INO.
- Infections and Inflammation: Encephalitis, meningitis, and brainstem inflammation can all have an effect on the MLF.
- Neoplasms: Tumors in the brainstem or those that put pressure on the MLF can cause INO.
- Neurodegenerative Diseases: Progressive supranuclear palsy (PSP) and amyotrophic lateral sclerosis (ALS) can occasionally be associated with INO.
Clinical Presentation
The clinical presentation of INO varies according to the size of the lesion and the underlying cause. The key features include:
- Impaired Adduction: The affected eye has limited movement toward the nose.
- **Abduction. When the contralateral eye attempts to look outward, it exhibits nystagmus.
- Diplopia: Eye misalignment causes double vision, which is a common complaint.
- Gaze Palsy: If the lesion extends beyond the MLF, patients may develop gaze palsy, which is the inability to move both eyes in a specific direction.
Variants of INO
There are several variants of INO, each with unique clinical features:
- Bilateral INO: This is a condition in which both MLFs are affected, as seen in MS. Patients have impaired adduction in both eyes and bilateral nystagmus.
- One-and-a-Half Syndrome: A severe form in which a unilateral MLF lesion spreads to include the adjacent abducens nucleus, causing complete gaze palsy on one side and INO on the other.
- Wall-Eyed Bilateral INO (WEBINO): Bilateral INO with primary gaze deviation and outward-facing eyes (exotropia).
Diagnostic Challenges
INO can be difficult to diagnose because it shares similarities with other neurological conditions. A thorough clinical examination and detailed patient history are required for a correct diagnosis. The key diagnostic steps are as follows:
- Neurological Examination: Evaluate eye movements for signs of impaired adduction and abduction nystagmus.
- Imaging: Magnetic Resonance Imaging (MRI) of the brain is critical in determining the location and cause of the lesion. MRI can detect demyelinating plaques in MS, ischemic changes in strokes, and other structural abnormalities.
Effects on Quality of Life
INO has a significant impact on a patient’s quality of life, especially when combined with underlying chronic conditions such as MS. Diplopia and visual disturbances can interfere with daily activities like reading, driving, and other tasks that require precise visual coordination. Furthermore, the presence of INO frequently indicates a more severe neurological disease, necessitating comprehensive medical treatment.
Examination Methods for Internuclear Ophthalmoplegia
To accurately identify the location and underlying cause of internuclear ophthalmoplegia, a combination of clinical evaluation and advanced imaging techniques is required.
Clinical Evaluation
Diagnosing INO begins with a thorough clinical evaluation. Key components are:
- History Taking: A thorough patient history is required to identify any underlying conditions such as MS, recent stroke, trauma, or infections.
- Neurological Examination: The evaluation of eye movements is critical. The examiner is looking for impaired adduction in the affected eye and abduction nystagmus in the contralateral eye. Other neurological signs may also appear, depending on the underlying cause.
Imaging Techniques
Imaging is critical in confirming the diagnosis of INO and determining the underlying cause.
- Magnetic Resonance Imaging (MRI) is the gold standard for detecting INO. High-resolution images of the brainstem can reveal demyelinating lesions associated with MS, ischemic changes from a stroke, or other structural abnormalities such as tumors. Specific MRI sequences, such as T2-weighted and FLAIR, are especially effective in detecting these lesions.
- Diffusion Tensor Imaging (DTI): An advanced MRI technique for mapping white matter tracts in the brain. DTI can provide detailed images of the MLF, allowing you to assess its integrity and detect subtle lesions that may not be visible on standard MRI sequences.
Lab Tests
Laboratory tests may be required to identify or rule out specific underlying causes.
- Lumbar Puncture: In cases of suspected MS, cerebrospinal fluid (CSF) analysis can be performed. The detection of oligoclonal bands in the CSF aids in the diagnosis of MS.
- Blood Tests: Comprehensive blood tests to detect signs of infection, inflammation, or autoimmune disease. Specific infections (such as syphilis and Lyme disease) may also be tested if necessary.
Electrophysiological tests
Electrophysiological tests can help evaluate the function of the neural pathways involved in eye movements:
- Electrooculography (EOG): Assesses the electrical activity of the extraocular muscles during eye movements. EOG can detect abnormalities in the coordination of eye movements that are characteristic of INO.
- Visual Evoked Potentials (VEP): Evaluate the integrity of the visual pathways. Abnormal VEP results may indicate demyelination or other neuropathologies that contribute to INO.
Therapeutic Approaches to Internuclear Ophthalmoplegia
The primary goals of treating internuclear ophthalmoplegia (INO) are to address the underlying cause, manage symptoms, and prevent complications. The treatment strategy varies according to whether the INO is caused by multiple sclerosis (MS), stroke, trauma, infection, or another condition.
Symptomatic Treatment
- Prism Glasses: These can help manage diplopia (double vision) by realigning the visual fields, alleviating one of INO’s most common and troublesome symptoms.
- Eye Patching: Patching one eye can provide immediate relief from diplopia, especially in an acute setting. This is typically a temporary measure.
- Botulinum Toxin Injections: In some cases, injecting botulinum toxin into the extraocular muscles can temporarily reduce nystagmus and improve eye alignment.
Disease-Specific Treatments
- Multiple Sclerosis (MS): Because MS is a common cause of INO, addressing the underlying condition is critical. Disease-modifying therapies (DMTs) such as interferons (e.g., interferon beta-1a), glatiramer acetate, and newer agents like natalizumab and ocrelizumab can reduce relapses and slow disease progression.
- Stroke: If INO is caused by a stroke, acute treatment may include thrombolytic therapy if the patient presents early enough. Long-term management entails secondary prevention strategies such as antiplatelet therapy, anticoagulation in atrial fibrillation, blood pressure control, and lifestyle changes.
- Infections: Proper antimicrobial therapy is required for INO caused by infections. Antibiotics for bacterial infections, antivirals for viral infections, and antifungal treatments for fungal infections are all possible options.
- Inflammatory and Autoimmune Disorders: When INO is associated with conditions such as lupus or sarcoidosis, immunosuppressive therapy, such as corticosteroids, methotrexate, or other immunosuppressants, may be required.
Rehabilitation and Support
- Vision Therapy: Tailored vision therapy programs can help improve coordination and strengthen the eye muscles. Neuro-optometry or physical therapy specialists frequently oversee these programs.
- Physical Therapy: Physical therapy can help patients with INO due to systemic neurological conditions by improving overall coordination and balance.
- Occupational Therapy: This can assist patients in adjusting to vision changes and continuing to perform daily activities safely and effectively.
Innovative and Emerging Therapies
- Stem Cell Therapy: Researchers are investigating the use of stem cell therapy for neuroregeneration in MS and other neurodegenerative diseases that cause INO. Early results are promising, but this treatment is still experimental.
- Gene Therapy: Advances in gene therapy have the potential to correct genetic defects associated with certain neurodegenerative diseases. While not widely available, this is a rapidly developing field with enormous potential.
- Neuroplasticity-Based Therapies: These treatments capitalize on the brain’s ability to reorganize and form new neural connections. Techniques such as transcranial magnetic stimulation (TMS) and neurofeedback are being investigated for their ability to improve outcomes in neurological conditions that cause INO.
Monitoring and Follow-up
Patients with INO should have regular follow-up appointments with a neurologist and an ophthalmologist to monitor disease progression, assess treatment efficacy, and adjust management plans as needed. This multidisciplinary approach ensures comprehensive care while also addressing the neurological and ocular aspects of the condition.
Effective Ways to Improve and Prevent Internuclear Ophthalmoplegia
- Manage Underlying Conditions: Effective management of chronic conditions such as multiple sclerosis or cardiovascular disease can lower the risk of developing INO.
- Regular Medical Check-Ups: Routine check-ups can aid in the identification and management of risk factors for stroke and other conditions that can lead to INO.
- Healthy Lifestyle: Adopting a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking can lower the risk of stroke and other health problems.
- Blood Pressure Control: Keeping blood pressure within normal limits is critical for avoiding strokes, which can lead to INO.
- Diabetes Management: Proper diabetes management, including medication, diet, and regular monitoring, can help prevent complications such as strokes.
- Protective Eyewear: Wearing protective eyewear during activities that may cause head trauma can help prevent injuries that could lead to INO.
- Stress Management: Meditation, yoga, and getting enough sleep can help manage autoimmune conditions like MS.
- Stay Informed: Staying current on the latest research and advances in treatments for conditions such as MS and stroke can provide more options for prevention and management.
- Medication Adherence: Following the instructions of healthcare providers when taking prescribed medications for chronic conditions can help prevent complications that could lead to INO.
- Avoiding Infections: To avoid infections that could lead to neurological complications, practice good hygiene and get vaccinations.
Trusted Resources
Books
- “Neuro-Ophthalmology: Diagnosis and Management” by Grant T. Liu, Nicholas J. Volpe, and Steven L. Galetta
- “Clinical Pathways in Neuro-Ophthalmology: An Evidence-Based Approach” by Andrew G. Lee and Paul W. Brazis
- “Manual of Neuro-Ophthalmology” by Amar Agarwal
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Institute of Neurological Disorders and Stroke (NINDS): www.ninds.nih.gov
- Multiple Sclerosis Society: www.nationalmssociety.org
- MedlinePlus: medlineplus.gov
- Neuro-Ophthalmology Virtual Education Library (NOVEL): novel.utah.edu






