A smart return to training protects the gains you already own and rebuilds the ones you lost—without lighting up symptoms. The goal is not to “make up” missed workouts; it is to stack small, reliable sessions that restore energy, confidence, and tolerance. This guide gives you a clean clearance checklist, a stepwise ramp for time and volume, and simple rules for reintroducing cardio and strength. You will learn which red flags matter, how to anchor recovery habits, and when to ask for help. Think of it as a map back to normal training that respects age-related considerations without treating you as fragile. For how these sessions fit into a broader plan that supports VO₂max, strength, and everyday movement, start with our pillar on longevity-focused training essentials, then use this roadmap to move from “I’m back” to “I’m better.”
Table of Contents
- Clearance Checklist: Symptoms Resolved, Energy, and Sleep Readiness
- Ramp Protocol: Session Length, RPE/RIR, and Volume Progression
- Cardio Rebuild: Walks, Zone 2, and Intervals Reintroduced
- Strength Rebuild: Exercise Order, Range of Motion, and Tempo
- Red Flags: Pain, Heart Rate Responses, and Excess Fatigue
- Recovery Anchors: Hydration, Protein, and Light Mobility
- When to Seek Clinician Input or Modify the Plan
Clearance Checklist: Symptoms Resolved, Energy, and Sleep Readiness
Before you ramp, confirm that your body is ready to absorb training. A simple, honest checklist beats guesswork and saves you from relapses that cost weeks.
1) Symptoms resolved (or stable) for 48–72 hours.
- Illness: No fever for 24 hours without medication; cough, congestion, or GI symptoms settled to mild and trending better; appetite returning. Residual, mild symptoms can coexist with easy movement, but spikes or new symptoms suggest waiting.
- Musculoskeletal injury: Pain at rest ≤2/10, swelling minimal or absent, and daily tasks (stairs, carrying groceries) feel normal or trending better. Range of motion should allow your chosen exercises in a reduced form without sharp pain.
2) Morning checks look normal.
- Rested HR: Within ~5–7 bpm of your personal baseline.
- Sleep: Two consecutive nights of reasonable sleep (even if not perfect).
- Energy on waking: You feel “okay to move,” not “foggy and dragging.”
3) Movement tolerance today.
- A 10–15 minute easy walk leaves you at baseline within two hours.
- Light mobility (hips, ankles, T-spine) feels good, not aggravating.
- For injuries: five pain-free bodyweight reps of your simplest pattern (e.g., sit-to-stand, wall push-up, hip hinge) are possible with clean form.
4) Medications and co-conditions understood.
- New meds (antibiotics, steroids, antihypertensives) can change effort perception and HR response. Train conservatively for the first week after any change.
- If you manage chronic conditions (cardiovascular disease, diabetes, autoimmune disorders), align your return with your clinician’s guidance.
5) “Two-hour/next-day rule” commitment.
- Two-hour rule: Symptoms should settle to pre-session baseline within two hours.
- Next-day rule: You should wake at or near baseline. If you do not, scale duration or intensity before repeating a similar session.
6) Psychological green light.
- You can choose an easy plan without the urge to “make up” lost time.
- You accept stopping early if a red flag appears.
Pass this checklist, and your ramp will almost always go smoothly. If you fail at any step, delay one to three days, keep walking and mobility easy, and reassess. Confidence comes from stacking small wins and remaining pain-curious rather than pain-fearful.
Ramp Protocol: Session Length, RPE/RIR, and Volume Progression
Your first week back sets the tone. Keep sessions short, efforts submaximal, and progress predictable. Use RPE (rate of perceived exertion, 1–10) and RIR (reps in reserve) to steer intensity without chasing numbers.
Week 0 (first three to five sessions): “Half and easy.”
- Length: 50–60% of your pre-illness/injury session time (e.g., 25 minutes if you used to do 45–50).
- RPE: Cap at 5–6 for cardio; 4–5 for strength.
- RIR: Leave 3–4 reps in reserve on every strength set.
- Volume: One to two sets per exercise, total of 6–10 working sets.
- Purpose: Rehearse patterns, test tolerance, and end each session feeling you could have done more.
Week 1–2: Build time before intensity.
- Length: +10–20% time each successful session until you reach your usual session duration.
- RPE: Keep cardio mostly 5–6; include brief 20–60 second spurts at 6–7 only if the two-hour/next-day rules remain clean.
- RIR: Shift to 2–3 RIR on primary lifts; add one set to the primary movement if form stays crisp.
- Sets/Volume: Aim for 8–14 total working sets per session by the end of Week 2.
- Deload trigger: If you fail the next-day rule, repeat the prior successful session or cut volume by ~30% for two to three sessions.
Week 3–4: Reintroduce “threshold” stress carefully.
- Cardio: Add one controlled interval set per week (e.g., 5×1 minute at RPE 7 with 1–2 minutes easy).
- Strength: Nudge to 1–2 RIR on a single main lift, keep everything else 2–3 RIR.
- Density: Maintain rest periods; don’t compress rest to “work harder.”
- Ceiling: If any joint feels sketchy, hold at this level until a full week of clean next-day mornings accumulates.
Injury-specific pacing (musculoskeletal).
- Range first, then load, then speed. Start with reduced range or supportive variations (e.g., box squats, incline push-ups), build to full range, then add load, and only later speed or plyo intent.
- Single-limb symmetry checks: Compare left/right effort and control; keep volume slightly higher on the quieter side, not the painful one.
Session endings should feel tidy, not heroic. Leave the gym or close your workout app with breath calm and joints relaxed. That discipline compounds. For help formatting sets, reps, and rest into a clean session, skim our primer on simple session design and plug in the “return” numbers above.
Cardio Rebuild: Walks, Zone 2, and Intervals Reintroduced
Cardio tolerance returns fastest when you restore frequency and time at Zone 2 (steady, conversational pace) before adding intensity. Think “more easy minutes, then a little spice.”
Phase A (3–7 days): Easy, frequent walks.
- Dose: 10–30 minutes, 4–6 days in the first week. If fatigue lingers, split into two short bouts (e.g., 2×12 minutes).
- Terrain: Flat to gentle inclines. Avoid heat, wind, and heavy packs early on.
- Breath: You should speak in full sentences throughout. If not, slow down.
Phase B (1–2 weeks): Build Zone 2.
- Minutes: Increase daily walk durations by ~10–20% per successful session until one or two sessions reach 35–50 minutes.
- Variety: Add gentle hills or a steady bike/rower session to disperse load on legs and feet.
- Checks: HR sits near your pre-illness Zone 2 for similar paces, or your RPE feels easier at the same pace.
Phase C (weeks 2–4): Controlled intervals.
- Template 1 (intro): 6–8×1 minute at RPE 7 with 1–2 minutes easy.
- Template 2 (stepped): 3×3 minutes at RPE 6–7 with 2 minutes easy.
- Frequency: Once weekly at first; twice only after two clean weeks.
- Stop-rules: If HR stays elevated >15–20 bpm above baseline during recovery, or breathing remains labored, finish with an easy cooldown and reduce the next session’s intensity.
Returning after respiratory illness.
- Progress the exhale. Long, soft exhales during walks (4–6 seconds) help settle breathing rate.
- Uphill guardrails: Early incline work is fine if it keeps you conversational; avoid steep descents that spike effort and joint load.
- Cough or chest tightness: Keep intensities at RPE ≤6 until symptoms are gone for a full week.
Returning after non-cardiac surgery or extended bed rest.
- Short, frequent bouts trump single long sessions (e.g., 3×10–15 minutes).
- Seated/upper-body options (bike/erg) reduce leg swelling while keeping HR training consistent.
- Compression and elevation post-walk may reduce dependent swelling in the first week.
Hills and stairs later.
- Reintroduce a hill or stair session after you’ve logged two consistent Zone 2 weeks. Start with short, steady climbs (RPE 6) before any intervals. For a deeper menu of gentle outdoor progressions, see Zone 2 pacing ideas that pair well with flat and hilly terrain.
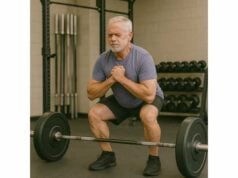
Strength Rebuild: Exercise Order, Range of Motion, and Tempo
Good strength returns when you respect order, range, and tempo. Your first goal is positions; load and effort follow.
Order: large patterns before accessories.
- Main patterns: squat or sit-to-stand, hip hinge, push, pull, and a carry or hold.
- Accessories: calf raises, rows/rotations, cuff or glute work.
- Core: anti-extension and anti-rotation holds to finish—short, high-quality sets.
Range of motion (ROM): scale and restore.
- Squat family: Start with box squats or assisted sit-to-stands; progress depth as knees and hips tolerate.
- Hinge family: Hip hinges with a dowel or light RDLs teach position without back irritation.
- Pressing: Start with incline or push-up to a box before flat or overhead pressing if shoulders or ribs feel stiff.
- Pulling: Cable rows and assisted pull-downs are usually well tolerated; keep ribs “stacked” to avoid low-back arching.
Tempo: slower lowers, calm pauses.
- Rule of three: Lower in ~3 seconds, pause 1 second at end range, stand or press smoothly without jerking.
- Benefits: Control protects joints, retrains groove, and keeps RPE lower for the same load.
Sets, reps, and RIR.
- Week 0–1: 2×8–10 on main patterns at 3–4 RIR; accessories 1–2×10–12 at 2–3 RIR.
- Week 2–3: 3×6–8 on one main lift at 2–3 RIR; other patterns stay 2×8–10 at 2–3 RIR.
- Week 4: Allow a single top set at 1–2 RIR if all morning checks are clean, then back-off sets at 2–3 RIR.
Pain and stiffness rules.
- Green: Muscle effort during sets, no joint pain, and baseline next day.
- Yellow: Mild joint awareness that clears in two hours—hold volume steady and keep RIR higher for 3–4 sessions.
- Red: Sharp, localized joint pain or swelling—swap the pattern for a friendlier variant (e.g., split squat → heel-elevated split squat; press → incline press) and reduce volume.
Accessory priorities for older lifters.
- Calves/feet: Heel raises (straight-knee and bent-knee) for tendon health and walking efficiency.
- Upper back: Face pulls and chest-supported rows for posture and shoulder comfort.
- Carries: Suitcase carries and farmer carries to rebuild anti-rotation and grip.
Technique support.
- Add a light mobility primer (hips, shoulders, ankles) before sessions so ROM gains stick. For step-by-step cues on squat, hinge, push, and pull, check our quick guide to technique fundamentals and overlay the tempo guidelines above.
Red Flags: Pain, Heart Rate Responses, and Excess Fatigue
Most setbacks are avoidable if you know what to watch for. Treat the signs below as course-correct now signals, not panic buttons.
Pain signals that matter.
- Sharp, localized joint pain during a set or stride that worsens on each rep—stop the exercise and swap for a friendlier variant.
- Swelling or heat around a joint later the same day.
- Night pain that wakes you or throbs at rest.
Cardiovascular and breathing cues.
- Disproportionate HR response: HR rises unusually fast for easy efforts or stays elevated >15–20 bpm above normal during rests—reduce intensity and lengthen recoveries.
- Chest pain/pressure, dizziness, or unusual shortness of breath—stop immediately and seek medical assessment.
- Irregular pulse awareness with lightheadedness—also stop and consult.
Fatigue and recovery markers.
- Two-hour rule failure: You still feel wrung out or symptomatic two hours after a session.
- Next-day slump: You wake with heavy legs, a resting HR elevated >7–10 bpm, or “brain fog.”
- Sleep disruption: Training late or too hard fragments sleep—shift intensity earlier or lower it.
Injury-specific watchouts.
- Tendons (Achilles, patellar): Morning stiffness that worsens week to week—reduce plyo/step-down volume by 30–50%, bias isometrics briefly (20–30 second holds), and reintroduce slow eccentrics later.
- Back/hip: Pinch or zinger with hinge patterns—shorten range, reset brace, and return to the dowel hinge to groove setup.
- Shoulder: Painful arc during presses—swap to neutral-grip incline, reduce range, and add low-load cuff and scapular control work.
Environment and heat illness.
- In heat or high humidity, lower intensity by one RPE point, extend rest, and prioritize shade and fluids. Early warning signs (goosebumps, chills, confusion) mean stop now and cool.
What to do when a red flag appears.
- Stop that exercise and switch to a non-provocative pattern.
- Trim the session by 30–50% and end with light mobility or a walk.
- Note the trigger (exercise, load, surface, time of day, heat, shoes).
- Repeat the last successful session next time; only progress after two clean attempts.
If repeated red flags cluster despite conservative choices, press pause and seek a second opinion. A short, skilled assessment often saves weeks of trial and error. On days when you feel shaky, favor easy walks and mobility—your base grows on recovery days as much as training days. For ideas on organizing those lighter days, see active recovery strategies that speed the rebound.
Recovery Anchors: Hydration, Protein, and Light Mobility
Returning strong is less about the single hard workout and more about stringing good days together. These anchors keep the engine fueled and tissues calm while your training minutes climb.
Hydration you can stick to.
- Daily aim: Pale-yellow urine most of the day.
- Pre-session: Drink a glass of water or unsweetened tea ~60 minutes before you train.
- Session length guide: For sessions <45 minutes, you usually don’t need intra-workout fluids beyond preference; for 45–75 minutes, sip water; for hotter or longer sessions, consider a light electrolyte mix.
- After illness: If you had fever or GI loss, bias fluids and electrolytes for several days—small, frequent sips beat chugging.
Protein and energy.
- Daily protein: Aim for ~1.2–1.6 g/kg/day (older adults benefit from the higher end).
- Per meal: 25–40 g high-quality protein, especially the first meal of the day to blunt muscle loss from detraining or bed rest.
- Carbs around training: Add a fist-sized portion (fruit, oats, rice, potatoes) within two hours before or after training to restore glycogen and support immune function.
Micronutrients and timing.
- Prioritize whole foods, colorful plants, and a baseline multivitamin only if advised. Most people returning from routine illness do not need high-dose supplements; consistency beats novelty.
Sleep that actually restores.
- Keep a stable wake time; align last caffeine ~8 hours before bed.
- Short unwinding routine (dim light, 10 minutes of quiet reading or breath work).
- If nights are choppy, move higher-effort sessions earlier and shorten evening workouts.
Light mobility that sticks.
- 10-minute daily flow: ankle rocks (10/side), half-kneeling hip flexor opener (20–30 seconds/side), T-spine openers (6/side), wall slides (8–10), glute bridge holds (2×20 seconds), and a 2-minute easy walk.
- Dose around sessions: Before training, use short, dynamic prep; after, use gentle holds and breathing to downshift the nervous system.
Isometrics for sore tendons.
- 3–5×20–30 second mid-range holds (e.g., calf raises at the top, wall sits at ~60–70° knee angle) can reduce symptom irritability without delaying the return. Reintroduce slow eccentrics later.
Pacing for busy weeks.
- When work or family stress spikes, maintain frequency with shorter sessions rather than canceling—we’re protecting habit memory as much as physiology.
- Use the “3 by 20” rule on chaotic days: 20 minutes Zone 2, 20 controlled strength minutes, 20 minutes to prep food for tomorrow. Even one of the three keeps momentum.
Your recovery anchors should feel mundane, almost boring. That’s the point—boring works. For a plug-and-play warm-up that slides into any comeback session, see our short list of joint prep and activation options you can rotate.
When to Seek Clinician Input or Modify the Plan
Most comebacks fit in the simple framework above. Sometimes, you need sharper eyes or medical clearance before pushing on.
Seek clinician input promptly if you notice:
- Cardiovascular signs: Chest pain, unexplained shortness of breath, dizziness, fainting, or HR responses that are wildly out of proportion to effort.
- Neurologic symptoms: New weakness, loss of coordination, numbness/tingling that spreads or persists, or changes in balance not explained by deconditioning.
- Infection concerns: Fever returning after it resolved, persistent productive cough with shortness of breath, or any red flag your doctor highlighted at discharge.
- Musculoskeletal red flags: Night pain that wakes you, joint locking/giving way, visible deformity, or swelling that recurs after easy sessions.
Modify your plan (without waiting) if you notice:
- Two consecutive next-day rule failures. Halve intensity/volume for two to three sessions, then reattempt.
- Localized tendon flare. Swap fast or deep work for isometrics and reduced ROM variants; use a slower ramp across two to four weeks.
- Sleep falling apart. Shorten evening sessions, reduce intensity after 6 p.m., and favor walking + mobility on late-training days.
- Psychological drag. If you dread sessions, cut the plan in half and re-earn momentum with quick wins; enjoyment predicts adherence better than any metric.
Special populations and scenarios.
- Cardiometabolic disease: Follow your clinician’s limits for HR, BP, and symptom thresholds; keep a log and bring it to follow-ups.
- Long layoff (>6–8 weeks): Treat yourself as a beginner for four weeks; you will regain faster than a novice, but your connective tissue likes patience.
- Post-surgery: Prioritize the surgeon’s protocol; when cleared, fold those steps into this framework rather than the other way around.
- Recurrent overuse injuries: Identify and change one load driver—surface, volume spikes, shoe wear, or poor sleep—before adding more training.
Bottom line. The comeback is successful when it feels mostly uneventful: simple sessions, steady energy, symptoms quiet. Err on the side of “slightly less today so I can definitely train tomorrow.” Your future self benefits more from a hundred quiet workouts than from one heroic one.
References
- WHO guidelines on physical activity and sedentary behaviour 2020 (Guideline)
- 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease 2020 (Guideline)
- ACSM Expert Consensus Statement on Exertional Heat Illness: Recognition, Management, and Return to Activity 2023 (Guideline)
Disclaimer
This article provides general educational guidance for returning to exercise after illness or injury. It is not a substitute for personal medical advice, diagnosis, or treatment. Seek professional evaluation if you experience chest pain, unusual shortness of breath, dizziness, marked or worsening pain, joint swelling, neurologic symptoms, or if symptoms persist despite conservative adjustments. Follow your clinician’s instructions when they differ from general recommendations.
If you found this resource helpful, please consider sharing it on Facebook, X (formerly Twitter), or any platform you prefer, and follow us for future updates. Your support helps us continue creating practical, high-quality content for long-term health.