What is an Oculomotor Nerve Palsy?
Oculomotor Nerve Palsy, also known as Third Nerve Palsy, is a neurological condition characterized by dysfunction of the third cranial nerve, which controls the majority of eye movements. This nerve controls the majority of the eye muscles, including those that enable eyelid elevation and pupil constriction. Damage to the oculomotor nerve can cause a variety of symptoms, including double vision, drooping eyelids (ptosis), and an outward deviation of the affected eye. Understanding this condition is critical because it can indicate serious medical issues.
Comprehensive Analysis of Oculomotor Nerve Palsy
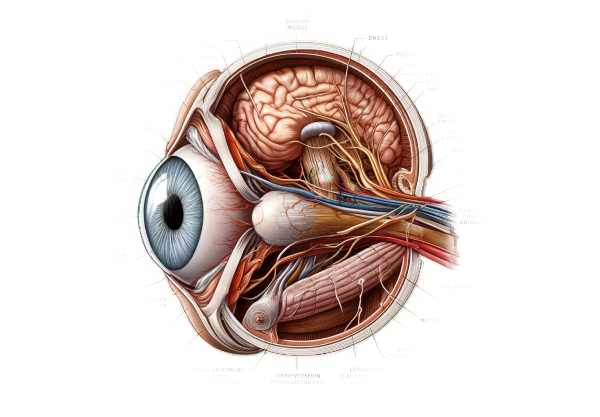
Structure and Function of the Oculomotor Nerve
The oculomotor nerve, also known as the third cranial nerve, originates in the midbrain and passes through the cavernous sinus before entering the orbit via the superior orbital fissure. It innervates the following eye muscles: superior rectus, inferior rectus, medial rectus, inferior oblique, and levator palpebrae superioris. It also sends parasympathetic fibers to the pupil, which are responsible for pupillary constriction and accommodation.
Etiology
Oculomotor nerve palsy can result from various etiologies, broadly classified into ischemic, compressive, traumatic, and inflammatory causes:
- Ischemic Causes: Diabetes mellitus and hypertension can cause microvascular ischemia, resulting in oculomotor nerve damage. This is more common in older adults and is characterized by pupil sparing.
- Compressive Causes: Aneurysms, particularly those in the posterior communicating artery, tumors, and high intracranial pressure can all compress the oculomotor nerve. Compressive lesions frequently affect the pupil due to the superficial location of parasympathetic fibers.
- Trauma Causes: Head injuries can cause direct or indirect damage to the oculomotor nerve, resulting in palsy. Fractures to the skull base or orbit are particularly dangerous.
- Inflammatory Causes: Infections (e.g., meningitis, syphilis) and autoimmune diseases (e.g., multiple sclerosis, sarcoidosis) can both cause inflammation in the oculomotor nerve.
- Congenital Causes: Some people are born with oculomotor nerve palsy as a result of birth trauma or developmental abnormalities.
Clinical Presentation
Patients with oculomotor nerve palsy frequently present with the following constellation of symptoms:
- Ptosis: Upper eyelid drooping due to levator palpebrae superioris muscle involvement.
- Ophthalmoplegia: Eye movement is limited, particularly in the upward, downward, and inward directions, due to paralysis of the superior rectus, inferior rectus, medial rectus, and inferior obliques.
- Outward Deviation of the Eye: The unopposed action of the superior oblique and lateral rectus muscles, innervated by the sixth and fourth cranial nerves, causes the eye to deviate outward and downward.
- Diplopia: Double vision occurs when the eyes are misaligned.
- Mydriasis: Pupil dilation caused by paralysis of the sphincter pupillae muscle, which impairs pupillary constriction. This is common in compressive lesions.
- Loss of Accommodation: Inability to focus on nearby objects due to ciliary muscle paralysis.
Pathophysiology
The pathophysiology of oculomotor nerve palsy is different depending on the underlying cause:
- Ischemic Neuropathy: In ischemic cases, small blood vessels supplying the nerve become occluded, resulting in nerve infarction. The central portion of the nerve, which contains motor fibers, is more vulnerable to ischemia than the peripheral parasympathetic fibers.
- Compression: Aneurysms and tumors apply external pressure to the oculomotor nerve. The parasympathetic fibers on the nerve’s surface are often the first to be affected, resulting in pupil involvement.
- Trauma:* Direct trauma can cause nerve transection or avulsion, whereas indirect trauma can stretch or compress the nerve.
- Inflammation: Inflammatory processes can cause demyelination and axonal damage to nerve fibers, resulting in functional impairment.
Differential Diagnosis
The differential diagnosis of oculomotor nerve palsy is:
1) Myasthenia Gravis: An autoimmune disorder that causes weakness in the voluntary muscles that control eye movements and eyelids. It can mimic the symptoms of oculomotor nerve palsy.
- Thyroid Eye Disease: Hyperthyroidism can cause inflammation and swelling of the eye muscles, which can result in abnormal eye movements similar to oculomotor nerve palsy.
- Chronic Progressive External Ophthalmoplegia is a mitochondrial disorder that causes gradual weakness of the eye muscles, resulting in similar symptoms.
- Orbital Apex Syndrome: A condition caused by lesions in the orbital apex that affects multiple cranial nerves and results in a complex presentation, including oculomotor nerve palsy.
Complications
Untreated or poorly managed oculomotor nerve palsy can result in a variety of complications:
- Persistent Diplopia: Constant double vision can impair daily activities and quality of life.
- Vision loss: Severe cases involving compressive lesions such as aneurysms can result in vision loss if not treated promptly.
- Aneurysm Rupture: When an aneurysm is the underlying cause, it has the potential to rupture, resulting in subarachnoid hemorrhage, which can be fatal.
- Strobismus: Misalignment of the eyes can become permanent if the nerve does not heal, resulting in strabismus.
- The Psychosocial Impact: Ptosis and eye misalignment can cause significant psychological distress and social difficulties.
Prognosis
The prognosis of oculomotor nerve palsy is dependent on the underlying cause.
- Ischemic Neuropathy: In general, the prognosis is good, with many patients recovering partially or completely within a few months.
- Compressive lesions: The prognosis is determined by the timing of treatment and the type of compressive lesion. Surgical intervention for aneurysms or tumors can lead to a significant recovery.
- Trauma:* Recovery is variable and dependent on the severity of nerve damage. Some cases may lead to permanent deficits.
- Inflammatory Causes: The prognosis is often favorable with proper medical treatment of the underlying inflammatory condition.
- Congenital Cases: The prognosis varies, and in some cases, surgical intervention is required to correct ptosis and strabismus.
How Oculomotor Nerve Palsy is Diagnosed?
Oculomotor nerve palsy requires a comprehensive approach that includes clinical examination, imaging studies, and, in some cases, laboratory tests to determine the underlying cause.
Clinical Examination
Diagnosing oculomotor nerve palsy begins with a thorough clinical examination. Key aspects of the exam include:
- History Taking: Obtain a thorough patient history to identify potential risk factors such as diabetes, hypertension, head trauma, and previous infections.
- Visual Acuity Test: Determine the impact on vision.
- Pupil Examination: Look for anisocoria (unequal pupil sizes) and the light reflex to determine the involvement of parasympathetic fibers.
- Eye Movement Testing: Evaluating the eyes’ range of motion in all directions to detect muscle paralysis.
- Eyelid Position: Measuring the degree of eyelid drooping to determine ptosis.
Imaging Studies
Imaging is critical in determining the cause of oculomotor nerve palsy, particularly in cases of suspected compressive lesions or trauma.
- Magnetic Resonance Imaging (MRI): MRI with contrast is the preferred imaging modality for evaluating soft tissue structures such as the brainstem, cavernous sinus, and orbit. It aids in the identification of tumors, aneurysms, and inflammatory lesions.
- Magnetic Resonance Angiography (MRA) or Computed Tomography Angiography (CTA): These are used to see blood vessels and identify aneurysms or vascular malformations.
- Computed Tomography (CT) Scan: Used to identify bony fractures in trauma cases as well as to detect calcified lesions.
Treatment Options for Oculomotor Nerve Palsy
Treatment for Oculomotor Nerve Palsy (Third Nerve Palsy) is tailored to the condition’s underlying cause, with the goal of restoring normal function, alleviating symptoms, and preventing complications. Medical, surgical, and rehabilitative treatment options may be considered.
Medical Treatment
- Ischemic Causes: Management of ischemic neuropathy, which is common in patients with diabetes or hypertension, focuses on controlling the underlying disease. This includes optimizing blood sugar levels, controlling blood pressure, and enhancing overall vascular health. Antiplatelet therapy, such as aspirin, may be recommended to reduce the risk of future ischemic events.
- Inflammatory and infectious causes: When inflammation or infection is the root cause, special treatments are required. Corticosteroids are a common anti-inflammatory. Antimicrobial or antiviral therapy is used to treat infectious causes based on the pathogen identified.
Surgical Treatment
1) Aneurysms and Tumors: Surgical intervention is frequently required to treat compressive lesions such as aneurysms or tumors. Aneurysm clipping or endovascular coiling can be used to remove the aneurysm and relieve pressure on the oculomotor nerve. Tumors may require surgical resection, with the approach varying according to the tumor’s location and type.
2) Trauma: For severe traumatic injuries to the oculomotor nerve, surgical repair may be required, especially if there is associated damage to the surrounding structures.
Rehabilitation Treatments
- Prism Glasses: Prism glasses can help with diplopia (double vision). These glasses help to align the visual fields, which reduces or eliminates double vision.
2) Occlusion Therapy: Patching one eye can help with diplopia temporarily by blocking visual input from the misaligned eye.
- Orthopic Exercises: These exercises aim to strengthen the eye muscles and improve coordination and control.
Innovative and Emerging Therapies
- Botulinum toxin Injections: Botulinum toxin (Botox) injections can temporarily paralyze the overactive muscles that cause the misalignment. This can help to balance muscular forces and improve eye alignment.
- Neuroplasticity-Based Therapies: New research is looking into the potential of neuroplasticity-based therapies to improve the brain’s ability to adapt and compensate for impaired nerve function. TMS and neurofeedback are two techniques under investigation.
- Genetic Therapy: While still in the experimental stages, gene therapy has the potential to treat congenital forms of oculomotor nerve palsy by identifying and correcting underlying genetic defects.
Monitoring and Follow-up
Regular follow-up with an ophthalmologist or neurologist is essential for monitoring recovery progress and making necessary adjustments to treatment. Visual acuity tests, eye movement assessments, and imaging studies are all part of the follow-up process to ensure proper management and early detection of any recurrence or complications.
Effective Ways to Improve and Prevent Oculomotor Nerve Palsy
- Maintain optimal blood sugar and blood pressure levels with regular monitoring, medication, and healthy lifestyle habits. This lowers the likelihood of ischemic neuropathy affecting the oculomotor nerve.
- To prevent head injuries, wear protective gear like helmets during high-risk activities and create safe environments to reduce the risk of traumatic injuries to the head and eyes.
- Effectively manage chronic conditions, such as diabetes and hypertension, to reduce the risk of complications and oculomotor nerve palsy. Consult healthcare providers on a regular basis.
- Seek prompt medical attention for infections, especially those affecting the nervous system like meningitis or encephalitis, to avoid complications.
- Schedule regular eye exams, especially if you have underlying health conditions or symptoms that indicate ocular issues. Early detection and intervention can halt progression.
- Quit smoking and avoid secondhand smoke to prevent vascular and nerve damage.
- Maintain overall health and lower risk of vascular diseases by following a balanced diet rich in fruits, vegetables, and whole grains, as well as engaging in regular physical activity.
- Stay Hydrated: – Proper hydration is crucial for maintaining blood flow and lowering the risk of ischemic events.
- Educate Yourself: – Be aware of the signs and symptoms of oculomotor nerve palsy and other neurological conditions to seek immediate medical attention if necessary.
Trusted Resources
Books
- “Neuro-Ophthalmology: Diagnosis and Management” by Grant T. Liu, Nicholas J. Volpe, and Steven L. Galetta
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Ophthalmology” by Myron Yanoff and Jay S. Duker
Online Resources
- American Academy of Ophthalmology (AAO)
- National Eye Institute (NEI)
- National Institute of Neurological Disorders and Stroke (NINDS)
- PubMed – Oculomotor Nerve Palsy Research