Vitamins B12 and folate power the enzymes that keep nerves wired, blood cells healthy, and DNA methylation on track. When they slip, the earliest signals are often biochemical—subtle shifts in homocysteine or methylmalonic acid—long before anemia or neuropathy appear. This article translates those labs into practical decisions: what to order, how to prepare, what the patterns mean, and when to act. You will also see common causes of abnormal results—diet, absorption, and medications—and a sensible follow-up plan. If you already track cardiometabolic markers or sleep, these tests add a brain-first lens to your longevity toolkit. For a broader testing roadmap that pairs well with B-vitamin evaluation, explore our curated guide to longevity biomarkers and tools.
Table of Contents
- Why These Markers Matter for Cognition, Nerves, and Methylation
- What to Order: Serum B12, Folate, Homocysteine (± MMA, holo-TC)
- Reading Patterns: Low-Normal B12 with High Homocysteine, and More
- Causes of Abnormal Results: Intake, Absorption, Medications
- Testing Cadence: Who Needs Periodic Rechecks
- When to Involve a Clinician: Neurologic Signs, Anemia, or GI Issues
- Record-Keeping: Tracking Symptoms Alongside Labs
Why These Markers Matter for Cognition, Nerves, and Methylation
B12 (cobalamin) and folate (vitamin B9) are co-factors in one-carbon metabolism—the network that recycles homocysteine to methionine and synthesizes nucleotides. In practice, this chemistry supports three systems that matter deeply for healthy aging:
- Nervous system. B12 enables myelin maintenance and methylation reactions in the brain and spinal cord. Deficiency can cause paresthesia, proprioceptive loss, gait imbalance, and cognitive changes. Folate deficiency typically presents with cognitive slowing or low mood rather than the posterior column signs often seen in B12 deficiency. Either way, early biochemical changes often precede symptoms.
- Hematology. B12 or folate deficits impair DNA synthesis in bone marrow, producing megaloblastic changes—enlarged red cells (macrocytosis), anemia, and sometimes neutrophil hypersegmentation. Yet normal hemoglobin does not exclude deficiency; labs may flag trouble years before anemia develops.
- Methylation economy. Homocysteine sits at the junction of these pathways. When B12 or folate is limited (or vitamin B6 is low), homocysteine accumulates. Elevated homocysteine is a useful risk signal: it correlates with vascular and cognitive outcomes in population data and nudges clinicians to search for reversible causes like low intake, malabsorption, hypothyroidism, kidney impairment, or drug effects.
Why use more than one test? Serum B12 reflects circulating cobalamin but not necessarily tissue sufficiency. Functional markers—methylmalonic acid (MMA) for the B12-dependent mitochondrial pathway and homocysteine for the methionine cycle—reveal enzyme-level effects. When tissue B12 is insufficient, MMA typically rises before anemia or neurologic symptoms. Homocysteine climbs with either B12 or folate shortfalls (and with B6 gaps), but also with kidney dysfunction and hypothyroidism, so context matters.
For longevity-minded readers, the real value is early detection and targeted correction. You can act long before nerve injury or cognitive decline. Equally important: avoid over-supplementation when labs are normal, which adds cost and sometimes confounds interpretation. The rest of this guide shows how to order wisely, read patterns clearly, trace causes, and follow up with purpose.
What to Order: Serum B12, Folate, Homocysteine (± MMA, holo-TC)
A practical, staged approach balances cost with clarity:
Core panel for most adults
- Serum B12. Typical lab cutoffs: deficiency often flagged at <200 pg/mL (≈148 pmol/L); “borderline” 200–300 pg/mL (≈148–221 pmol/L). Remember: normal serum B12 does not always mean normal tissue status.
- Serum folate. Most labs report sufficiency >4–5 ng/mL (≈10–12 nmol/L); interpret with diet history and medications. Red blood cell (RBC) folate reflects longer-term status but is less commonly needed in routine practice.
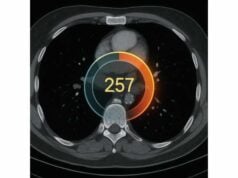
- Total homocysteine. Typical reference ranges are ~5–15 μmol/L. Persistent values >10–12 μmol/L merit a closer look, especially when paired with borderline B12 or low folate.
Add when results are borderline or symptoms suggest deficiency
- Methylmalonic acid (MMA). A more specific functional marker for B12 status. Elevated MMA supports tissue-level B12 deficiency even when serum B12 is “normal.” Be cautious in renal impairment, which can raise MMA independent of B12.
- Holotranscobalamin (holo-TC). The “active B12” fraction bound to transcobalamin. Low holo-TC can indicate early B12 shortfall before total B12 drops.
When to reflex to MMA or holo-TC
- Serum B12 200–400 pg/mL with neurologic symptoms, macrocytosis, or elevated homocysteine.
- Clinical risk is high (older age, vegetarian/vegan pattern without B12 sources, metformin or PPI use, post-bariatric or ileal disease) even if B12 sits near the lower normal band.
Preparation and sampling notes
- Fast is optional; a morning, non-hemolyzed sample reduces pre-analytical noise.
- Pause high-dose biotin 48–72 hours before testing if safe (assay interference risk varies by lab).
- Document kidney function (eGFR) and thyroid status when interpreting homocysteine.
What not to over-order
- Broad genetic panels rarely change first-line management. If you are already exploring gene–nutrient questions (e.g., MTHFR variants), place them in a clinical context; see our overview of genetic testing context for what is actionable.
Used together, these tests separate true deficiency from borderline numbers, guide supplementation route (oral vs intramuscular), and set a baseline to judge response.
Reading Patterns: Low-Normal B12 with High Homocysteine, and More
Lab patterns tell a story. Here’s how to read the common ones with practical next steps.
1) Low-normal B12 with elevated homocysteine; MMA normal
Think folate insufficiency or B6 insufficiency, not necessarily B12. Review intake (leafy greens, legumes, fortified grains), alcohol, and medications that deplete folate (e.g., methotrexate, some antiepileptics). If folate is low and B12 mid-range, correcting folate should normalize homocysteine. Recheck in 8–12 weeks.
2) Low-normal B12 with elevated MMA (± homocysteine)
This suggests early or tissue-level B12 deficiency. Consider diet (low animal products), malabsorption (autoimmune gastritis, post-bariatric surgery, ileal disease), or drugs that impair absorption (metformin, PPIs). If symptoms exist—paresthesia, gait imbalance—start treatment without delay and investigate cause in parallel.
3) Normal B12 and folate with high homocysteine; MMA normal
Cast a wider net: kidney function, hypothyroidism, B6 status, lifestyle (smoking, heavy coffee intake), and age. Homocysteine rises as eGFR falls. If reversible contributors are found and addressed, repeat in 8–12 weeks. When kidney impairment is present, homocysteine becomes a less specific signal—look at the whole clinical picture alongside kidney markers.
4) Very low B12 (<200 pg/mL) with high MMA and homocysteine
Treat promptly. Neurologic risks justify parenteral B12 initially (e.g., intramuscular hydroxocobalamin or cyanocobalamin) and a search for pernicious anemia or other malabsorption causes. Once stable, many patients transition to high-dose oral maintenance if absorption permits.
5) Normal or high folate with low B12, high homocysteine
High folate can mask hematologic signs while neurologic injury progresses in B12 deficiency. Always check B12 before advising folate supplements in older adults or those with neuropathic symptoms. Correct B12 first; add folate only if low.
6) Macrocytosis (MCV >100 fL) with normal B12/folate
Think alcohol use, liver disease, hypothyroidism, certain medications, or early myelodysplasia—do not assume nutrition alone. Retest and expand the workup if macrocytosis persists.
7) Post-treatment interpretation
- B12 levels rise quickly with therapy; they may overshoot without indicating excess.
- MMA and homocysteine normalize more slowly—expect improvements over 2–12 weeks.
- Persistent elevation despite supplementation suggests non-adherence, ongoing malabsorption, renal impairment (MMA), or unaddressed folate/B6 gaps (homocysteine).
A single outlier rarely decides management. Patterns across symptoms, history, and repeat labs do.
Causes of Abnormal Results: Intake, Absorption, Medications
Low intake
- Vegetarian or vegan diets without fortified foods or B12 supplements. B12 is bound to animal proteins; fortified plant milks and nutritional yeast are common non-animal sources.
- Alcohol overuse, restricted eating, or low-quality diets can depress folate.
Gastric and ileal factors
- Autoimmune gastritis (pernicious anemia). Loss of intrinsic factor and parietal cells blocks B12 absorption; antibodies may be detectable.
- Gastric surgeries (bariatric, gastrectomy) and ileal disease or resection reduce absorption.
- Hypochlorhydria from aging or acid suppression reduces release of B12 from food; crystalline B12 in supplements is better absorbed.
Medications
- Metformin can lower B12 over time (mechanism likely involves altered ileal uptake).
- Proton pump inhibitors (PPIs) and H2 blockers reduce gastric acid, impairing food-bound B12 release.
- Folate antagonists (methotrexate), trimethoprim, and some antiepileptics can depress folate status.
- Nitrous oxide (recreational or procedural) oxidizes active B12, precipitating neurologic injury; this warrants urgent evaluation if symptoms occur after exposure.
Physiology and comorbidities
- Kidney dysfunction raises homocysteine and MMA independent of vitamin status; interpret with eGFR.
- Hypothyroidism can raise homocysteine and cause macrocytosis; treat thyroid first if abnormal.
- Pregnancy increases folate requirement; prenatal folic acid prevents neural tube defects but B12 must be adequate to support neurological development.
Laboratory nuance
- Assay interference (rare) and high-dose biotin can disrupt immunoassays.
- Reference ranges vary; interpret using the same lab over time.
- High folate with low B12 can mask anemia while neurologic injury continues—check B12 before high-dose folate in at-risk groups.
Iron status matters too
Iron deficiency can complicate macrocytosis patterns (mixed micro- and macrocytosis) and fatigue. If the picture is confusing, review iron and ferritin alongside B-vitamin testing.
In short, think in layers: intake, absorption, medications, and comorbidities. Correct what is modifiable, treat confirmed deficiencies, and set a timeline to verify biochemical response.
Testing Cadence: Who Needs Periodic Rechecks
Testing rhythm depends on baseline risk, how far labs fall from targets, and whether you are changing diet or medications.
Low-risk, normal baseline
- If diet includes reliable B12 sources (animal foods or fortified products) and folate-rich plants, and initial B12, folate, homocysteine are normal, recheck every 2–3 years or sooner if symptoms arise.
- Athletes or highly active individuals do not need special B-vitamin testing unless intake is restricted or symptoms appear.
Moderate risk
- Adults ≥60, vegetarians/vegans, metformin or PPI users, post-bariatric patients, and those with IBD or celiac disease benefit from annual B12 checks. Add homocysteine (and MMA if B12 is borderline).
- If starting or increasing metformin or long-term PPIs, obtain a baseline and recheck at 12 months, then annually.
High risk or symptomatic
- Neurologic symptoms (numbness, pins-and-needles, gait imbalance), macrocytosis, or unexplained cognitive changes warrant immediate testing (B12, folate, homocysteine, ± MMA) and treatment without delay if B12 is clearly low.
- After initiating therapy, recheck MMA and/or homocysteine in 8–12 weeks to confirm functional recovery. For ongoing malabsorption (e.g., pernicious anemia), maintenance dosing continues indefinitely, with 6–12-month checks.
During pregnancy or planning
- Confirm folate adequacy and B12 status pre-conception and early in pregnancy, especially with vegetarian eating patterns or prior gastric surgery. Prenatal folic acid is standard; ensure B12 is not overlooked.
When lifestyle changes
- Major diet shifts (e.g., moving to fully plant-exclusive) or long travel/work changes affecting food quality justify a 3–6-month check-in.
Helpful adjuncts between labs
- Simple tools—sleep regularity, fatigue trends, and cognitive focus—can flag issues early. If you already track night-to-night patterns, see how sleep and wearable trends correlate with your energy and concentration. These do not replace labs, but they can prompt timely re-testing.
Cadence is not about testing more; it is about testing when decisions change: starting supplements, stopping a drug that impairs absorption, or responding to new symptoms.
When to Involve a Clinician: Neurologic Signs, Anemia, or GI Issues
Certain findings call for prompt clinical evaluation and, often, treatment before every confirmatory result is back:
- Neurologic symptoms. Progressive numbness or tingling in the feet or hands, loss of vibration sense, imbalance, or cognitive decline—especially with low or borderline B12—warrant immediate therapy. Neurologic injury can become irreversible if correction is delayed.
- Megaloblastic anemia or macrocytosis. If MCV is >100 fL or there is anemia with hypersegmented neutrophils, treat and evaluate the cause in parallel (dietary, autoimmune gastritis, medications, malabsorption). Mixed deficiencies (iron plus B12/folate) can blur classic patterns.
- Gastrointestinal flags. Chronic diarrhea, weight loss, history of gastric or ileal surgery, or autoimmune gastritis symptoms suggest absorption problems. Testing may include intrinsic factor antibodies, H. pylori evaluation, or endoscopy as guided by a specialist.
- Medication triggers. New or long-term metformin or acid suppression with emerging symptoms merits testing and, if low, treatment plus a plan for monitoring.
- Recreational nitrous oxide exposure. New neurologic symptoms after exposure require urgent B12 assessment and treatment.
- Complex differentials. When homocysteine remains elevated despite normal B12/folate and good kidney function, consider hypothyroidism, rare inborn errors, or other systemic contributors. Concurrent endocrine issues can complicate the picture; if TSH or free T4/T3 are off, address those first using thyroid checkpoints.
Route and dosing decisions are clinical.
- Parenteral B12 is preferred for severe deficiency, neurologic involvement, or malabsorption (e.g., pernicious anemia) because it bypasses intrinsic factor.
- High-dose oral B12 (e.g., 1,000 mcg/day) can maintain levels in many patients once stabilized, even with some malabsorption, thanks to passive diffusion.
- Folate should be replaced when low—but avoid high-dose folate until B12 deficiency is excluded or treated.
Finally, involve a clinician if results do not fit symptoms, if there is no biochemical response after appropriate therapy, or if new red flags appear (fever, night sweats, marked weight loss), which point away from simple nutrient deficiency.
Record-Keeping: Tracking Symptoms Alongside Labs
Clear records turn numbers into decisions. Build a lightweight system that pairs symptoms, diet, medications, and labs across time.
What to log (briefly)
- Symptoms: paresthesia, balance changes, fatigue, mood, memory, tongue soreness, headaches. Note onset, severity (0–10), and changes after interventions.
- Diet highlights: weekly counts of animal-based B12 sources (eggs, dairy, fish, meat) or fortified items; leafy greens, legumes, and fortified grains for folate.
- Supplements and meds: B12 dose/form (cyanocobalamin, methylcobalamin, hydroxocobalamin), folate form (folic acid vs methylfolate), start/stop dates; metformin, PPIs, H2 blockers, methotrexate, antiepileptics, nitrous oxide exposure.
- Comorbid checks: weight trend, alcohol frequency, thyroid labs, kidney function (eGFR).
- Lab dates and results: B12 (with units), folate, homocysteine, MMA, CBC with MCV. Use the same lab when possible for consistency.
How to interpret your own trendline
- Improvements in MMA and homocysteine after treatment lag 2–12 weeks; do not chase weekly changes.
- A rising B12 level after therapy confirms exposure, but functional markers tell you whether enzymes recovered.
- If symptoms improve but MMA stays mildly elevated, look for confounders: low eGFR (raises MMA), low B6 (raises homocysteine), or adherence issues.
Practical guardrails
- Avoid megadoses “just in case.” Use targeted trials with follow-up labs and clear stop/continue rules.
- Re-evaluate the cause, not only the deficiency. If pernicious anemia or chronic malabsorption is present, plan for lifelong maintenance and periodic monitoring.
- Share your one-page chart—symptoms, doses, and lab dates—with your clinician. It shortens visits and improves decisions.
Good records are the cheapest diagnostic tool you own. They reveal patterns, shorten time to the right treatment, and prevent both under- and over-supplementation.
References
- Vitamin B12 deficiency in over 16s: diagnosis and management 2024 (Guideline)
- Homocysteine, B vitamins, and cardiovascular disease 2021 (Mendelian Randomization)
- Vitamin B12 – Health Professional Fact Sheet 2025
- Folate – Health Professional Fact Sheet 2022
- Age-specific reference ranges are needed to interpret serum methylmalonic acid concentrations in the U.S. population 2019
Disclaimer
This article is educational and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your clinician about testing, interpretation, and treatment—especially if you have neurologic symptoms, anemia, kidney or thyroid disease, are pregnant, or take prescription medications. If you develop sudden neurologic changes, chest pain, severe weakness, or other alarming symptoms, seek urgent care.
If you found this helpful, please consider sharing it on Facebook, X, or any platform you prefer, and follow us for future updates. Your support helps us continue producing careful, evidence-based guides.