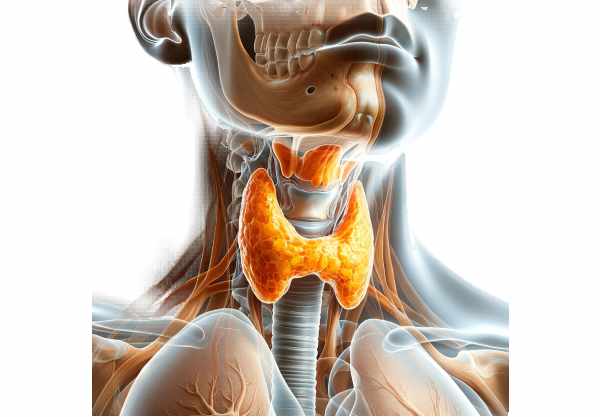
The thyroid gland is a vital endocrine organ responsible for regulating metabolism, growth, and development through the production of hormones. Shaped like a butterfly, it sits at the front of the neck and plays a crucial role in maintaining energy balance and overall health. Dysfunction in the thyroid can lead to widespread systemic effects, influencing everything from weight and energy levels to mood and heart health. This comprehensive guide delves into the complex anatomy of the thyroid, its essential physiological functions, common disorders, state-of-the-art diagnostic methods, diverse treatment options, and practical lifestyle tips to optimize thyroid health.
Table of Contents
- Anatomical Structure
- Cellular & Microstructure
- Vascular Supply, Innervation & Lymphatics
- Embryology & Variations
- Physiology & Hormonal Functions
- Common Thyroid Disorders
- Diagnostic Methods
- Treatment Options
- Supplements for Thyroid Health
- Lifestyle & Dietary Practices
- Trusted Resources
- Frequently Asked Questions
- Disclaimer & Sharing
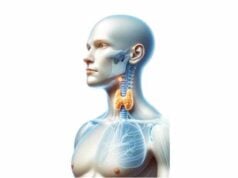
Anatomical Structure
The thyroid gland has a distinctive butterfly shape with two lateral lobes connected by a narrow isthmus. Positioned in the anterior neck over the trachea, it spans the level of the C5 to T1 vertebrae. Each lobe is asymmetrical in size—with the right lobe typically larger than the left—and is enclosed by a thin, fibrous capsule that offers both structural support and protection. The gland’s unique configuration enables it to efficiently produce and release hormones into the bloodstream. Notably, many individuals also possess a pyramidal lobe, an anatomical variant extending upward from the isthmus, which is a remnant of the embryonic thyroglossal duct.
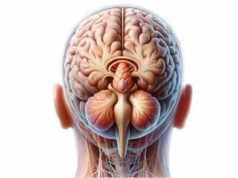
Cellular & Microstructure
At the microscopic level, the thyroid’s functional units are the thyroid follicles. Each follicle is a spherical structure lined by a single layer of cuboidal to columnar epithelial cells known as follicular cells. These cells are responsible for synthesizing thyroid hormones through a series of complex biochemical reactions. Within each follicle lies the colloid, a protein-rich substance predominantly composed of thyroglobulin, which serves as the precursor for thyroid hormone production. Interspersed among the follicular cells are parafollicular (C) cells, which produce calcitonin—a hormone involved in calcium homeostasis. Together, these cellular components orchestrate the dynamic production and release of hormones that regulate metabolic activity throughout the body.
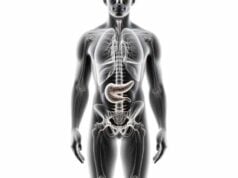
Vascular Supply, Innervation & Lymphatics
The thyroid gland is one of the most vascular organs in the body, receiving an abundant blood supply essential for its high metabolic demands. The gland is primarily supplied by two sets of arteries:
- Superior Thyroid Arteries: Branching from the external carotid arteries, these arteries supply the upper portions of the thyroid lobes and the isthmus.
- Inferior Thyroid Arteries: These arteries branch from the thyrocervical trunk of the subclavian arteries and supply the lower portions of the thyroid.
Venous drainage is achieved through the superior, middle, and inferior thyroid veins, which ultimately drain into the internal jugular and brachiocephalic veins.
The thyroid also possesses an extensive network of lymphatic vessels that drain into the prelaryngeal, pretracheal, and deep cervical lymph nodes. This robust lymphatic network plays a crucial role in immune surveillance and is significant in the context of thyroid cancer metastasis.
Innervation of the thyroid is provided by both sympathetic and parasympathetic fibers. Sympathetic nerves, originating from the cervical sympathetic ganglia, regulate blood flow by controlling vascular tone, while parasympathetic input from branches of the vagus nerve—particularly the recurrent laryngeal nerve—plays a role in glandular regulation, although it does not directly influence hormone secretion.
Embryology & Variations
The thyroid gland develops from the endodermal lining of the primitive pharynx during the fourth week of gestation. The thyroid primordium descends along the midline, passing anteriorly to the hyoid bone and laryngeal cartilages, to reach its final position in the lower neck. This journey is guided by the thyroglossal duct, a transient structure that normally degenerates by the eighth week. However, remnants of this duct can persist as thyroglossal duct cysts.
Common anatomical variations include:
- Ectopic Thyroid Tissue: Thyroid tissue may be found outside the usual location, such as at the base of the tongue (lingual thyroid).
- Pyramidal Lobe: A small lobe extending from the isthmus, present in about 50% of individuals, is a normal variant.
- Developmental Anomalies: Congenital hypothyroidism may result from dysgenesis or agenesis of the thyroid gland, leading to insufficient hormone production.
Understanding the embryological development of the thyroid helps clinicians diagnose congenital anomalies and plan surgical interventions accordingly.
Physiology & Hormonal Functions
The thyroid gland is essential for regulating metabolism, growth, and development by producing two primary hormones: thyroxine (T4) and triiodothyronine (T3).
Hormone Synthesis
The process of thyroid hormone synthesis is a multi-step biochemical pathway:
- Iodine Uptake: Follicular cells actively transport iodine from the bloodstream using the sodium-iodide symporter (NIS).
- Thyroglobulin Production: Follicular cells synthesize thyroglobulin, a large glycoprotein, which is secreted into the colloid.
- Iodination: The enzyme thyroid peroxidase (TPO) catalyzes the iodination of tyrosine residues in thyroglobulin, forming monoiodotyrosine (MIT) and diiodotyrosine (DIT).
- Coupling Reaction: TPO then couples these iodotyrosine molecules to form T4 (two DITs) and T3 (one MIT and one DIT).
- Release: When stimulated by thyroid-stimulating hormone (TSH) from the anterior pituitary, the follicular cells endocytose colloid droplets, and lysosomal enzymes release T4 and T3 into the bloodstream.
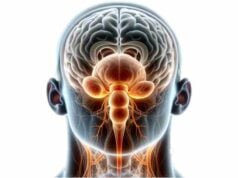
Regulation via the HPT Axis
The hypothalamic-pituitary-thyroid (HPT) axis tightly regulates thyroid hormone production:
- TRH (Thyrotropin-Releasing Hormone): Secreted by the hypothalamus, TRH stimulates the anterior pituitary to produce TSH.
- TSH (Thyroid-Stimulating Hormone): TSH binds to receptors on the thyroid gland, promoting hormone synthesis and secretion.
- Negative Feedback: Elevated levels of T3 and T4 inhibit TRH and TSH secretion, maintaining hormone levels within a narrow range.
Thyroid hormones are crucial for almost every cell in the body, influencing metabolism, energy expenditure, and growth. Their impact extends to neural development, cardiovascular function, and thermoregulation.
Common Thyroid Disorders
Thyroid disorders can result from autoimmune processes, iodine imbalance, genetic factors, or environmental influences. These conditions manifest in various ways, affecting hormone levels and metabolic processes.
Hypothyroidism
Hypothyroidism is characterized by insufficient production of thyroid hormones. The most common cause is Hashimoto’s thyroiditis, an autoimmune condition where the immune system attacks thyroid tissue.
- Symptoms: Fatigue, weight gain, cold intolerance, constipation, dry skin, hair loss, and depression.
- Treatment: Thyroid hormone replacement therapy (levothyroxine) is the standard treatment. Dosage adjustments are guided by regular TSH and free hormone level monitoring.
Hyperthyroidism
Hyperthyroidism results from excessive thyroid hormone production, with Graves’ disease being the most common cause. In Graves’ disease, autoantibodies stimulate the thyroid, leading to overactivity.
- Symptoms: Weight loss, heat intolerance, palpitations, anxiety, tremors, increased appetite, and insomnia.
- Treatment: Management options include antithyroid medications (methimazole, propylthiouracil), radioactive iodine therapy, beta-blockers for symptomatic relief, and thyroidectomy in refractory cases.
Goiter
Goiter refers to the enlargement of the thyroid gland and can occur in both hypothyroidism and hyperthyroidism.
- Causes: Iodine deficiency, autoimmune thyroid diseases, or nodular thyroid disease.
- Symptoms: Visible neck swelling, difficulty swallowing or breathing, and sometimes a feeling of tightness in the throat.
- Treatment: Based on the underlying cause; may include iodine supplementation, hormone therapy, or surgical removal in severe cases.
Thyroid Nodules
Thyroid nodules are discrete lesions within the thyroid that can be benign or malignant. They are frequently discovered incidentally on imaging.
- Diagnosis: Ultrasonography and fine-needle aspiration (FNA) biopsy help differentiate benign from malignant nodules.
- Management: Benign nodules are typically monitored, while malignant or suspicious nodules may require surgical removal.
Thyroid Cancer
Thyroid cancer, though relatively rare, is the most common endocrine malignancy. The major types include papillary, follicular, medullary, and anaplastic thyroid carcinoma.
- Symptoms: Often asymptomatic in early stages; later may include a neck mass, hoarseness, difficulty swallowing, and lymph node involvement.
- Treatment: Treatment usually involves surgical removal (thyroidectomy), radioactive iodine therapy, thyroid hormone suppression therapy, and, in advanced cases, chemotherapy and targeted therapy.
Thyroiditis
Thyroiditis is inflammation of the thyroid gland, which can be transient or chronic.
- Hashimoto’s Thyroiditis: An autoimmune disorder that gradually leads to hypothyroidism.
- Subacute (De Quervain’s) Thyroiditis: Typically follows a viral infection, causing temporary hyperthyroidism followed by hypothyroidism.
- Silent and Postpartum Thyroiditis: Usually mild and self-limiting, often requiring only symptomatic treatment.
Understanding these conditions and their underlying causes is essential for timely diagnosis and effective management, ensuring better long-term outcomes.
Diagnostic Methods
Accurate diagnosis of thyroid disorders relies on a combination of clinical evaluation, laboratory testing, imaging studies, and, when necessary, tissue sampling.
Clinical Evaluation
- Medical History:
Detailed assessment of symptoms such as weight changes, fatigue, neck swelling, and family history of thyroid disease. - Physical Examination:
Palpation of the thyroid gland to assess its size, texture, and presence of nodules, along with a general physical exam for signs of hyperthyroidism or hypothyroidism.
Laboratory Tests
- TSH Test:
The primary screening test for thyroid function. Elevated TSH suggests hypothyroidism, while low TSH is indicative of hyperthyroidism. - Free T4 and Free T3:
These tests measure the unbound thyroid hormones in circulation, providing a direct assessment of thyroid function. - Thyroid Antibodies:
Tests for anti-thyroid peroxidase (anti-TPO) and thyroid stimulating immunoglobulin (TSI) help diagnose autoimmune thyroid conditions like Hashimoto’s thyroiditis and Graves’ disease. - Tumor Markers:
In cases of suspected thyroid cancer, levels of thyroglobulin and calcitonin can aid in diagnosis and monitoring.
Imaging Techniques
- Ultrasonography:
The first-line imaging modality for evaluating thyroid nodules and goiters. It provides detailed information on nodule size, composition (solid vs. cystic), and vascularity. - Radioiodine Scintigraphy:
Assesses thyroid function by evaluating iodine uptake, helping to differentiate between hyperfunctioning (“hot”) and nonfunctioning (“cold”) nodules. - CT and MRI:
These advanced imaging techniques are useful for evaluating large goiters, retrosternal extensions, and invasive thyroid cancers. - PET/CT:
Used primarily for staging thyroid cancer and evaluating metastatic disease by detecting areas of increased metabolic activity.
Biopsy Procedures
- Fine-Needle Aspiration (FNA) Biopsy:
The gold standard for evaluating thyroid nodules, FNA allows for cytological examination to distinguish benign from malignant lesions. - Core Needle Biopsy:
Employed when FNA results are inconclusive, providing a larger tissue sample for histopathological analysis.
Molecular Testing
- Gene Expression Classifiers and Mutation Analysis:
These tests assess the genetic profile of thyroid nodules, aiding in the prediction of malignancy in indeterminate cases and guiding clinical management.
Treatment Options
Treatment strategies for thyroid disorders are tailored to the specific condition and the patient’s overall health. Options range from medical management to surgical interventions and advanced therapies.
Hypothyroidism Treatment
- Thyroid Hormone Replacement:
The cornerstone of hypothyroidism treatment is levothyroxine, a synthetic T4 hormone. Dosage is individualized based on weight, age, and severity of hypothyroidism, with regular TSH monitoring to ensure appropriate dosing. - Natural Desiccated Thyroid (NDT):
For some patients, NDT offers an alternative by providing both T4 and T3. However, careful monitoring is required due to variability in hormone levels.
Hyperthyroidism Treatment
- Antithyroid Medications:
Drugs such as methimazole and propylthiouracil (PTU) inhibit thyroid hormone synthesis. Methimazole is preferred in most cases due to its favorable side-effect profile. - Radioactive Iodine Therapy:
Oral administration of radioactive iodine-131 selectively destroys overactive thyroid tissue. This is a common treatment for Graves’ disease and toxic multinodular goiter, though it may lead to subsequent hypothyroidism. - Beta-Blockers:
Medications like propranolol provide symptomatic relief by controlling heart rate, tremors, and anxiety associated with hyperthyroidism. - Thyroidectomy:
Surgical removal of part or all of the thyroid is considered in cases of large goiters, nodules suspicious for malignancy, or when other treatments are contraindicated. Post-surgery, patients typically require lifelong thyroid hormone replacement.
Treatment of Thyroid Nodules and Goiter
- Observation:
Many benign nodules and small goiters can be managed with regular monitoring through ultrasound and thyroid function tests. - Ethanol Ablation and Radiofrequency Ablation (RFA):
Minimally invasive procedures used to shrink or eliminate benign nodules, providing relief from symptoms without the need for surgery. - Surgical Excision:
Indicated for nodules that are suspicious for malignancy or when there is significant compression of surrounding structures.
Thyroid Cancer Treatment
- Surgery:
Total or partial thyroidectomy is the primary treatment for thyroid cancer, often followed by lymph node dissection if metastasis is suspected. - Radioactive Iodine Therapy:
Used postoperatively to destroy residual thyroid tissue or metastatic cancer cells, particularly in differentiated thyroid cancers. - Thyroid Hormone Suppression Therapy:
High doses of levothyroxine are administered to suppress TSH, thereby reducing the risk of cancer recurrence. - External Beam Radiation & Chemotherapy:
Reserved for advanced, inoperable, or aggressive forms of thyroid cancer, these treatments are used to control tumor growth. - Targeted Therapy:
New agents, such as tyrosine kinase inhibitors (e.g., sorafenib, lenvatinib), are available for advanced thyroid cancers that do not respond to conventional therapies.
Thyroiditis Management
- Hashimoto’s Thyroiditis:
Treated primarily with thyroid hormone replacement to alleviate hypothyroid symptoms. In some cases, selenium and vitamin D supplementation may help modulate the autoimmune response. - Subacute Thyroiditis:
Often self-limiting; treatment focuses on symptom relief with NSAIDs or corticosteroids, and beta-blockers for hyperthyroid symptoms. - Postpartum and Silent Thyroiditis:
These conditions usually require supportive care and temporary thyroid hormone replacement, as they tend to resolve over time.
Supplemental & Nutritional Support for Thyroid Health
Proper nutrition and targeted supplementation can bolster thyroid function, support hormone synthesis, and mitigate oxidative stress. The following supplements have demonstrated benefits for thyroid health:
Key Nutrients and Vitamins
- Iodine:
Essential for thyroid hormone synthesis. Iodine-rich foods (e.g., seafood, dairy, and iodized salt) or supplements help prevent iodine deficiency disorders such as goiter. - Selenium:
Crucial for the conversion of T4 to the active T3 hormone and for protecting the thyroid from oxidative damage. Brazil nuts, seafood, and supplements can provide this mineral. - Zinc:
Supports thyroid hormone metabolism and immune function. Adequate zinc levels are vital for maintaining thyroid health. - Vitamin D:
Plays a role in immune regulation and may influence thyroid hormone production. Sun exposure, fortified foods, and supplements can help maintain optimal levels. - Vitamin C:
An antioxidant that aids in immune support and reduces oxidative stress, helping to protect thyroid tissue.
Herbal and Natural Supplements
- Ashwagandha:
An adaptogenic herb known to reduce stress and promote thyroid function by enhancing hormone production. - Turmeric (Curcumin):
Provides potent anti-inflammatory and antioxidant effects, which can help modulate autoimmune thyroid conditions. - Green Tea Extract:
Rich in catechins, this supplement has antioxidant properties that may support thyroid health and overall metabolism.
Omega-3 Fatty Acids
- Fish Oil:
High in omega-3 fatty acids, fish oil reduces inflammation and supports cell membrane integrity in thyroid tissue. - Flaxseed Oil:
A plant-based alternative that also offers anti-inflammatory benefits, aiding in overall endocrine health.
Antioxidants and Amino Acids
- Alpha-Lipoic Acid (ALA):
A potent antioxidant that protects thyroid cells from oxidative damage and supports energy production. - Coenzyme Q10 (CoQ10):
Essential for mitochondrial function, CoQ10 supports energy metabolism and reduces oxidative stress in thyroid cells. - L-Tyrosine:
An amino acid that serves as a precursor for thyroid hormone synthesis. Supplementation can be particularly beneficial in individuals with low tyrosine levels.
Lifestyle & Dietary Practices for Thyroid Health
Maintaining optimal thyroid function requires a holistic approach that includes healthy lifestyle and dietary practices. The following strategies can help ensure the thyroid operates efficiently:
Diet and Nutrition
- Balanced Diet:
Consume a diet rich in fruits, vegetables, lean proteins, and whole grains to provide the necessary nutrients for thyroid hormone production. - Iodine-Rich Foods:
Incorporate seafood, dairy products, and iodized salt to support hormone synthesis. - Antioxidant-Rich Foods:
Foods high in antioxidants—such as berries, leafy greens, and nuts—can help mitigate oxidative stress on the thyroid. - Limit Goitrogens:
While many nutritious foods contain goitrogens (e.g., cruciferous vegetables), cooking can deactivate these compounds. Moderation is key, especially for individuals with thyroid dysfunction.
Physical Activity
- Regular Exercise:
Moderate physical activity enhances metabolism, improves hormone balance, and supports overall endocrine health. - Consistency:
A consistent exercise routine can also help regulate stress hormones, indirectly benefiting thyroid function.
Stress Management
- Mindfulness and Meditation:
Practices like yoga, meditation, and deep breathing exercises reduce stress and cortisol levels, which can adversely affect thyroid function. - Adequate Sleep:
Aim for 7–9 hours of quality sleep each night to support hormone regulation and cellular repair.
Environmental and Lifestyle Considerations
- Avoid Toxins:
Limit exposure to environmental pollutants, pesticides, and endocrine disruptors by choosing organic foods and natural personal care products. - Stay Hydrated:
Adequate water intake is vital for metabolic processes and overall health. - Limit Caffeine and Alcohol:
Reducing the intake of stimulants and depressants can help maintain hormonal balance and reduce stress on the thyroid. - Regular Medical Check-Ups:
Routine screenings and thyroid function tests help detect and manage thyroid disorders early, ensuring timely intervention.
Trusted Resources for Thyroid Health
For further information on thyroid health, consider the following reputable sources, which offer evidence-based insights and comprehensive guidance:
Books
- “Thyroid Healing: The Truth behind Hashimoto’s, Graves’, Insomnia, Hypothyroidism, Thyroid Nodules & Epstein-Barr” by Anthony William
Explores the multifaceted causes of thyroid disorders and offers natural healing strategies including diet, supplements, and lifestyle changes. - “The Thyroid Connection: Why You Feel Tired, Brain-Fogged, and Overweight – and How to Get Your Life Back” by Amy Myers, MD
Provides an in-depth look at thyroid dysfunction, highlighting both conventional and holistic approaches to diagnosis and treatment. - “Hashimoto’s Thyroiditis: Lifestyle Interventions for Finding and Treating the Root Cause” by Izabella Wentz, PharmD
Focuses on autoimmune thyroid conditions with practical advice on managing symptoms and addressing underlying triggers.
Academic Journals
- Thyroid
The official journal of the American Thyroid Association, offering cutting-edge research on thyroid biology, diseases, and treatment modalities. - Journal of Clinical Endocrinology & Metabolism
A leading publication that features clinical studies, reviews, and guidelines on endocrine disorders, including thyroid conditions.
Mobile Apps
- Thyroid Tracker:
An app that helps users log symptoms, medication dosages, and lab results, offering insights into thyroid health and trends over time. - Boost Thyroid:
Designed specifically for those with hypothyroidism and Hashimoto’s, this app provides personalized advice, tracking tools, and educational resources. - MyThyroid:
A comprehensive tool for managing thyroid disorders, including reminders for medication, self-examination guides, and symptom tracking.
Frequently Asked Questions
What is the primary function of the thyroid gland?
The thyroid gland regulates metabolism, growth, and development by producing thyroid hormones (T3 and T4). These hormones influence almost every cell in the body, affecting energy levels, weight, and overall physiological processes.
How are thyroid hormones produced?
Thyroid hormone production involves iodine uptake, thyroglobulin synthesis, iodination, coupling reactions, and hormone release—all regulated by the hypothalamic-pituitary-thyroid axis through TRH and TSH.
What causes hypothyroidism?
Hypothyroidism is often caused by autoimmune thyroiditis (Hashimoto’s), iodine deficiency, thyroid surgery, radiation therapy, or medications that disrupt thyroid hormone production, leading to a decrease in hormone levels.
How is hyperthyroidism treated?
Hyperthyroidism is typically managed with antithyroid medications, radioactive iodine therapy, beta-blockers for symptomatic relief, and in some cases, surgical removal of thyroid tissue.
Can lifestyle changes improve thyroid health?
Yes, a balanced diet rich in iodine, selenium, and antioxidants, regular exercise, stress management, adequate sleep, and avoiding environmental toxins can significantly support thyroid health and proper hormone production.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized diagnosis and treatment.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness and promote thyroid health.