Glucose challenges help answer a practical question: how does your body handle a sugar surge in real life? The oral glucose tolerance test (OGTT) is standardized and focused; the mixed-meal tolerance test (MMTT) is closer to an actual meal. Both can reveal early metabolic shifts long before routine labs flag trouble. In this guide, you will learn what each test measures, where each shines, how to prepare, and how to interpret results alongside insulin and other markers. You will also see when retesting makes sense, how to minimize hassle, and how to translate numbers into everyday habits. For broader context on metabolic and cardiovascular tracking, explore our curated hub on longevity-focused biomarkers and tools.
Table of Contents
- What Each Test Measures: Glucose-Only vs Real-World Response
- Preparation: Carb Loading, Fasting, and Medications
- Protocols and Sampling Schedules
- Interpreting Curves: Peak, Area, and Insulin Patterns
- Pros and Cons: Cost, Convenience, and Tolerance
- When to Choose One Test over the Other
- How Often to Repeat and Pair with Other Markers
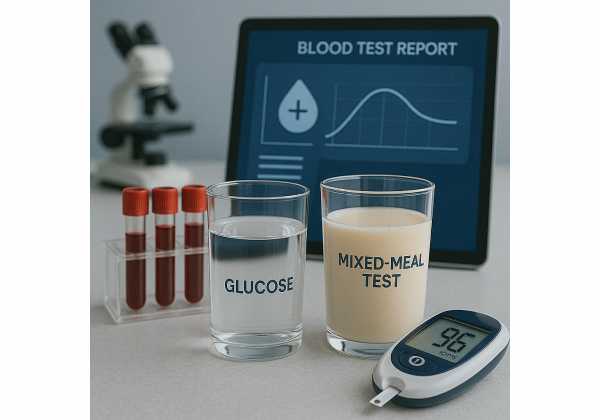
What Each Test Measures: Glucose-Only vs Real-World Response
If you want a clean, apples-to-apples measure of glucose handling, the OGTT is built for that purpose. You fast overnight and then drink a fixed dose of 75 g anhydrous glucose (adults). Blood draws at baseline and at specific intervals show how quickly your plasma glucose rises and returns toward normal. Because the “meal” is pure glucose, the signal is tightly standardized across clinics and populations. That standardization is why OGTT remains a reference tool for diagnosing impaired glucose tolerance and diabetes and for quantifying how your body responds to an acute carbohydrate load.
The mixed-meal tolerance test takes a different path. Instead of a glucose-only drink, you consume a defined meal that includes carbohydrates, protein, and fat—often a standardized liquid formula. This design triggers the full cascade of digestion, incretin signaling (e.g., GLP-1 and GIP), gastric emptying effects, and insulin secretion that occurs after real food. The MMTT therefore reveals not only glycemic control but also beta-cell function in a physiologic context, especially when insulin and C-peptide are measured alongside glucose. It can be highly informative in scenarios where insulin secretion capacity matters—such as suspected type 1 diabetes, long-standing type 2 diabetes with potential beta-cell burnout, or evaluation of therapy effects on endogenous insulin production.
Why do these differences matter for longevity? Early metabolic inflection points often appear after meals, not in fasting labs alone. Some people maintain normal fasting glucose yet demonstrate exaggerated post-challenge spikes or sluggish recovery. An OGTT isolates carbohydrate tolerance and insulin action in a controlled way. An MMTT approximates daily life, capturing the interplay of macronutrients, hormones, and gastric dynamics. In practice:
- Prefer OGTT when you need a standardized diagnostic benchmark or are comparing across time and labs.
- Prefer MMTT when you care about the integrated, meal-like response, especially insulin/C-peptide dynamics.
Both tests can be extended beyond “glucose at 2 hours.” Serial sampling (e.g., at 30–60–90–120 minutes) yields curves that highlight peak size and timing, recovery slope, and area-under-the-curve—metrics that add nuance to yes/no cutoffs.
Finally, remember what neither test shows directly: day-to-day patterns across varied meals, sleep, and activity. That is where ambulatory tools (like continuous glucose monitoring) complement single-day challenges. Used together, they paint a more complete picture of metabolic resilience.
Preparation: Carb Loading, Fasting, and Medications
Preparation shapes the validity of any challenge test. Small choices—like a very low-carb dinner—can skew next-day responses. For the OGTT, most labs ask for an overnight fast (typically 8–12 hours), only water in the morning, and avoidance of nicotine, caffeine, alcohol, and vigorous exercise before testing. Hydrate normally; dehydration can concentrate glucose and confound venous sampling. Sleep matters, too—poor sleep elevates sympathetic tone and can alter post-load glucose.
Carbohydrate loading is a frequent point of confusion. Many protocols still recommend consuming at least ~150 g/day of carbohydrates for three days before a diagnostic OGTT, particularly to avoid false positives after prolonged low-carb intake. That said, emerging data suggest the effect of short-term carbohydrate intake may vary by population (e.g., pregnancy vs non-pregnant adults, postpartum vs general). If you typically eat low-carb and want a standardized, guideline-aligned test, increase carbs for 3 days before the OGTT unless your clinician advises otherwise. Keep the rest of your routine stable.
For the MMTT, adhere to the same overnight fast and pretest behavior guidelines. The test is more “food-like,” but you still want apples-to-apples comparison across days. Ask in advance about the specific product or meal composition (calories and grams of carbs/protein/fat) and the drinking time window (e.g., finish within 5 minutes), because both affect results via gastric emptying and incretin responses. If your clinic uses a liquid formula, do not substitute your own smoothie or meal unless pre-approved—the point is standardization.
Regarding medications:
- Glucose-lowering agents: Your clinician may ask you to hold certain drugs the morning of the test (e.g., sulfonylureas, short-acting insulin) to avoid blunting diagnostic value or provoking hypoglycemia. Do not stop long-acting therapies without explicit instructions.
- GLP-1 receptor agonists/SGLT2 inhibitors: Policies differ. GLP-1 RAs slow gastric emptying, which can alter a meal test; SGLT2 inhibitors change renal glucose handling. Follow local protocol.
- Other agents and supplements: High-dose biotin can interfere with some immunoassays (insulin/C-peptide). If you routinely take biotin, ask whether you should pause it.
Finally, two practical notes to protect sample integrity: 1) confirm with the lab how samples are handled (e.g., immediate processing for insulin/C-peptide), and 2) arrive a bit early to relax; anxiety and rushing can shift autonomic tone and glucose dynamics.
Related reading on complementary laboratory markers: glucose markers beyond fasting.
Protocols and Sampling Schedules
OGTT (75 g glucose, adults): The minimal diagnostic protocol is a fasting draw (time 0) and a 2-hour draw after consuming 75 g anhydrous glucose within 5 minutes. Many longevity-oriented clinics add intermediate draws at 30, 60, and 90 minutes to capture peak magnitude and timing and to calculate area under the curve (AUC). If you want insight into insulin dynamics, ask for simultaneous insulin (and ideally C-peptide) at each time point. For people with hypoglycemia symptoms after high-carb loads, some protocols extend to 180 minutes to check for late dips.
MMTT (standardized meal): The specific formula varies, but common liquid options provide ~200–400 kcal with defined macronutrient composition (e.g., ~30–50 g carbohydrate, 10–20 g protein, 5–15 g fat). The participant typically consumes the drink over a fixed window (often 5 minutes). Sampling schedules range from practical (0, 30, 60, 90, 120 minutes) to extended (up to 180–240 minutes) when late responses matter (e.g., suspected reactive hypoglycemia or delayed gastric emptying). When beta-cell function is central, protocols emphasize insulin and C-peptide at each time point because C-peptide reflects endogenous insulin secretion independent of hepatic extraction.
Choosing a sampling density: More time points improve curve resolution but increase burden. A useful compromise for either test is 0/30/60/90/120 minutes with glucose and insulin; add C-peptide if available. This captures early-phase secretion (0–30 minutes), peak behavior (usually 30–60 minutes), and recovery (90–120 minutes). If late hypoglycemia is a concern, include 150 and 180 minutes. For research-level inference (e.g., oral minimal model estimates of insulin sensitivity and beta-cell responsivity), you need more points and specialized analysis; for clinical decision-making, the pragmatic five-point curve is often enough.
Pre-analytics and logistics:
- Confirm whether the lab uses plasma (fluoride/oxalate) or serum; OGTT cut points are defined for plasma glucose.
- For insulin/C-peptide, ensure prompt processing (many clinics centrifuge within 30 minutes and keep samples cool).
- Bring a snack for after the final draw to prevent feeling woozy.
Safety and comfort: Most people tolerate both tests well. Nausea is more common with the OGTT’s hyper-sweet drink. If you are prone to motion sickness or have gastroparesis, mention this beforehand; a slower ingestion window may be possible with an MMTT. Stay seated, avoid walking laps during the test (it changes glucose uptake), and tell the staff if you feel faint.
To extend insights beyond a single day, some readers pair a one-time challenge with short-term sensor use; see CGM setup and accuracy for a primer.
Interpreting Curves: Peak, Area, and Insulin Patterns
Think of a glucose challenge curve as a story with three acts: takeoff (0–30 minutes), peak and plateau (30–60 minutes), and recovery (60–120+ minutes). Each act contains information about insulin sensitivity and beta-cell function.
Key glucose features
- Peak height: Higher peaks suggest reduced first-phase insulin response and/or slower peripheral uptake. Peaks above ~180 mg/dL at 30–60 minutes warrant attention even if the 2-hour value normalizes.
- Time to peak: A delayed peak can reflect slower gastric emptying or delayed insulin release.
- Recovery slope: A brisk drop from 60 to 120 minutes points toward adequate insulin action; a flat or rising pattern suggests impaired disposal or insufficient secretion.
- Area under the curve (AUC): Integrates amplitude and duration—useful for comparing two tests in the same person.
Insulin and C-peptide patterns
- Early surge (0–30 minutes): A clear early rise signals competent first-phase secretion. A sluggish or absent early bump with a later rise often accompanies enlarged glucose peaks.
- Hyperinsulinemic curve with modest glucose: May indicate compensatory hypersecretion in early insulin resistance.
- Low insulin across the curve with high glucose: Points toward beta-cell insufficiency, more common in long-standing type 2 diabetes or autoimmune forms.
- C-peptide vs insulin: C-peptide avoids hepatic extraction bias and clarifies endogenous secretion when exogenous insulin is used.
Composite indices (when you have insulin):
- Insulinogenic index: ΔInsulin(30–0) / ΔGlucose(30–0); a proxy for early secretion.
- Matsuda index: Uses multiple time points to estimate whole-body insulin sensitivity during OGTT.
- Disposition index: Secretion adjusted for sensitivity—key for understanding whether secretion is appropriate for the prevailing resistance.
Context matters
- Lipid status: Elevated fasting triglycerides often travel with insulin resistance. A high TG\:HDL ratio supports that hypothesis when you see hyperinsulinemic curves.
- Body composition: More visceral adiposity often correlates with impaired recovery slopes.
- Sleep and stress: Recent sleep loss or acute stress can transiently worsen peaks; interpret in light of the week leading up to testing.
MMTT-specific nuance
Protein and fat slow gastric emptying and stimulate incretins, sometimes producing a lower glucose peak than OGTT for the same person, but with prolonged tailing. Insulin and C-peptide during MMTT better match everyday eating, so a strong early insulin/C-peptide rise with a contained glucose peak is reassuring; a blunted secretory pattern with prolonged hyperglycemia suggests limited beta-cell capacity in a real-world context.
Bottom line: do not over-weight a single cutoff. Look at peak, recovery, and insulin/C-peptide together, then integrate with fasting labs and lifestyle factors.
Pros and Cons: Cost, Convenience, and Tolerance
OGTT—Strengths
- Standardized stimulus: 75 g anhydrous glucose, fixed timing. This makes between-test and between-clinic comparisons more reliable.
- Diagnostic utility: Widely accepted thresholds for impaired glucose tolerance and diabetes.
- Shorter window: Minimal protocol requires only 0 and 120 minutes; optional intermediate draws add detail without a full morning commitment.
OGTT—Limitations
- Less physiologic: Pure glucose ignores effects of protein/fat on incretins and gastric emptying, so it may overstate responses relative to typical meals.
- Tolerance: Some people feel nauseated or light-headed; rare vomiting invalidates the test.
- Specificity for insulin dynamics: Without insulin/C-peptide, you cannot tell if a high peak is secretion failure, insulin resistance, or both.
MMTT—Strengths
- Real-world relevance: Includes mixed macronutrients, thus engaging incretin signaling and gastric physiology.
- Beta-cell assessment: With insulin and C-peptide, MMTT is excellent for estimating endogenous secretory capacity in clinical and research settings.
- Tolerance: Many find a flavored liquid meal easier to drink than glucose syrup.
MMTT—Limitations
- Standardization challenges: Different products and compositions make cross-study comparisons harder. Even small shifts in protein/fat can change curves.
- Longer visits: Common protocols run 120–180 minutes with multiple blood draws.
- Less codified thresholds: Unlike OGTT, fewer universally recognized cut points exist for diagnosis; interpretation leans on patterns and composite indices.
Cost and access
OGTT kits are inexpensive and widely available. MMTT requires purchasing or stocking specific formulas and measuring more analytes, which can raise costs. Ask your clinic about out-of-pocket estimates and whether insurance recognizes the indication (e.g., evaluation of hypoglycemia or beta-cell function).
Choosing for comfort and goals
If your main question is “Do I meet established criteria for impaired glucose tolerance or diabetes?” the OGTT suffices. If your priority is “How does my pancreas perform with a real meal, and do I still produce meaningful insulin?” the MMTT is a better tool—especially when matched with C-peptide.
Because wearables are now common, many readers use short stints of sensors to reduce clinic time and add context; see body composition’s link to insulin sensitivity when you interpret real-world glycemic responses as you train or lose fat.
When to Choose One Test over the Other
Choose OGTT when:
- You need a standardized diagnostic assessment for impaired glucose tolerance or diabetes, including pre-procedure clearance or program eligibility.
- You want to compare progress over time with a consistent, codified stimulus.
- You are early in a metabolic tune-up and want a baseline that aligns with established cutoffs.
Choose MMTT when:
- You need to evaluate residual beta-cell function (e.g., suspected autoimmune diabetes, long-standing type 2 diabetes with escalating needs).
- You have symptoms suggestive of post-prandial dysglycemia (e.g., fatigue or shakiness 1–3 hours after meals) and want a physiologic stimulus.
- You are assessing therapy effects on endogenous insulin (e.g., after weight-loss, changes in GLP-1 therapy, or remission attempts).
Choose both (staggered) when:
- You want diagnostic clarity and a real-world check. For example, do an OGTT for the formal benchmark, then an MMTT weeks later with insulin/C-peptide to quantify secretion under everyday conditions.
- You suspect gastric factors alter responses (delayed emptying can flatten OGTT peaks yet prolong meal glucose). The contrast between OGTT and MMTT curves can clarify mechanisms.
Special populations and caveats
- Athletes and low-carb eaters: If you follow very low-carb patterns, consider the 3-day carbohydrate normalization before OGTT to avoid an artifactually high response. For MMTT, discuss whether to use a composition closer to your usual meals versus a lab standard; know that changing the meal limits cross-test comparability.
- Weight-loss or GLP-1 therapy: Because gastric emptying and appetite change, an MMTT may better reflect your new physiology than OGTT alone.
- Gastrointestinal symptoms: If nausea is a barrier, a well-tolerated MMTT formula may help.
Decision workflow
- Define your primary question (diagnosis vs physiology vs therapy effect).
- Pick the test whose design answers that question most directly.
- Add insulin/C-peptide if beta-cell function matters.
- Plan a repeat only when the result would change your next step (therapy, training, nutrition).
If you are also monitoring day-to-day patterns, pairing the chosen challenge with a week of home data can be powerful; a sensor trial or structured finger-stick plan adds practical texture to the lab result.
How Often to Repeat and Pair with Other Markers
Most people do not need frequent challenge tests. Repeat only when results will inform a decision. Here is a pragmatic cadence:
If your baseline test is normal and risk is low
- Emphasize routine surveillance (fasting glucose, A1c, lipids, waist-to-height ratio) and lifestyle. Consider a repeat OGTT in 2–3 years if you have a strong family history or your weight, sleep, or activity substantially change. Use earlier retesting if you develop symptoms of post-meal fatigue or excessive thirst/urination.
If your baseline test is borderline
- Re-test in 6–12 months after a focused training and nutrition block. Choose the same modality to allow fair comparison. If your goal is to understand why a borderline OGTT shifted (secretion vs sensitivity), an MMTT with insulin/C-peptide can clarify mechanisms.
If your baseline test is clearly abnormal
- Use the result to guide action (nutrition, resistance training, sleep, pharmacotherapy). Re-test at ~3–6 months if you start or change therapy or if you want objective feedback on a lifestyle program. Again, repeat the same test for comparability; add the other test only if it will change management (e.g., considering medication de-intensification based on improved beta-cell output).
What to pair with challenge tests
- A1c and fasting insulin/glucose: Track medium-term exposure and basal insulin demand. The three together triangulate chronic vs acute control.
- ApoB or non-HDL cholesterol: Metabolic dysfunction often co-travels with atherogenic lipoproteins; improving insulin sensitivity can help, but lipids deserve their own targets.
- Body composition: Shifts in fat-free mass and visceral fat strongly influence insulin action; waist measurements are a simple proxy.
- Blood pressure and sleep quality: Both affect insulin sensitivity and post-meal glycemia.
Avoid overtesting
Challenge tests are time-consuming and can provoke unpleasant symptoms in sensitive individuals. Once you have a clear direction and the tools to act, let training, nutrition, sleep, and medication changes run for several months before checking again. The exception is if symptoms worsen or a clinician needs information sooner to adjust therapy.
Finally, translate numbers into practice. A steeper recovery slope after training is encouraging. A rising early insulin bump with lower peak glucose during MMTT can indicate better first-phase secretion—an early win even before A1c shifts. Use the data to reinforce the habits that moved those curves.
References
- 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2025 2025 (Guideline)
- Carbohydrate Intake and Oral Glucose Tolerance Test Results in the Postpartum Period 2023
- A simplified protocol based on a standardized meal‐stimulated beta‐cell response to stratify people living with non-insulin-treated type 2 diabetes 2025
- Assessment of Insulin Secretion and Insulin Resistance in Humans and Animal Models 2021 (Systematic Review)
- Lessons From the Mixed-Meal Tolerance Test: Use of 90-Minute and Fasting C-Peptide in Pediatric Diabetes 2013
Disclaimer
This article provides general educational information on glucose challenge testing and related markers. It is not a substitute for personalized medical advice, diagnosis, or treatment. Always discuss testing choices, preparation, and interpretation with your clinician, especially if you take glucose-lowering medications, have symptoms of hypoglycemia, or have other medical conditions.
If you found this useful, please consider sharing it with friends or colleagues on Facebook, X, or your preferred platform, and follow us for future updates. Your support helps us keep producing practical, high-quality content.






